Madison B. Sharp*, Andrew R. Milewski*, Claire Lamneck, and Katherine McKenzie
Abstract
Individuals applying for asylum must demonstrate a well-founded fear of persecution. By documenting signs of torture and other forms of abuse, medical evaluations can provide forensic evidence to support asylum claims. The backlog of pending immigration cases in the United States recently exceeded one million. Student-run asylum medicine clinics conduct forensic evaluations to assist in the asylum adjudication process. The Physicians for Human Rights National Student Advisory Board administered surveys to student-run clinics in the US in 2017 and 2018. Retrospective analysis evaluated the completion rates of forensic evaluations, caseload capacities, and training frequencies. Student-run asylum clinics completed 38.8% more forensic evaluations in 2017 than in 2016. In 2016, 33% of clinics received forensic evaluation requests that exceeded their capacity, a figure that rose to 50% in 2017. The number of clinicians trained by asylum clinics increased nearly fourfold between 2016 and 2017, and the number of students trained grew by 81%. A recent surge in armed conflict has contributed to record numbers of asylum applications in the US. The results of this survey reveal the burgeoning capability of student-run asylum clinics to provide evaluations, a trend that underscores medical students’ ability to significantly impact human rights issues. Student-run asylum clinics are poised to fill an increasingly important role in supporting victims of torture and persecution.
Introduction
An asylum seeker is a person who has left their country of origin due to persecution or fear of future persecution and whose request for sanctuary has yet to be processed. They are seeking the right to be recognized as a refugee and be granted legal and other protection. There are two ways to apply for asylum in the United States (US): the affirmative process and the defensive process. To apply affirmatively, an individual must be present within the US and submit Form I-589 within a year of arriving. A person in the defensive asylum process requests asylum in immigration court as a defense against deportation. Tens of thousands of individuals seek asylum in the US each year to escape persecution or torture in their home countries.1 Human rights violations, armed conflict, and worsening humanitarian crises have contributed to the nearly 1.7 million new asylum applications reported worldwide in 2017, a substantial increase from years prior.2 With 331,700 new claims, the US received the most asylum applications of any country in 2017.3 The backlog of immigration cases in the US, including pending asylum claims, reached 642,700 in 2017, nearly 50% more than in 2016.4 Fewer than 40% of applicants are granted asylum in the US: only 26,568 individuals obtained asylum in 2017.5
Individuals seeking asylum bear the burden of proof to demonstrate persecution, most of whom carry scars on their bodies and minds as the only forensic evidence of the abuses they have suffered. Through forensic evaluations, trained clinicians identify sequelae of trauma and document their findings in affidavits.6 These medico-legal documents can help corroborate the experiences of asylum seekers and consequently help victims of torture or abuse access justice through asylum. However, lawyers have only limited access to trained physicians.7 By connecting immigration attorneys to clinicians, asylum clinics housed at medical schools significantly expand access to pro bono forensic evaluations and critical documentation. These clinics, many of which are student-led initiatives, serve as organizing hubs that pair clinicians with students to perform evaluations, educate providers and trainees about asylum and human rights, and connect asylum seekers to medical and social services. These organizations generally comprise a team of medical students that manages the clinic’s operations and receives guidance from student and faculty leaders.8
Physicians for Human Rights (PHR), a non-governmental organization devoted to advocating for health and human rights, works closely with asylum clinics and provides resources to train the next generation of evaluators. The PHR National Student Advisory Board comprises a team of medical students who streamline communication between PHR student chapters and the PHR national office. The board aims to inspire medical students to address health and human rights violations now and in their future careers. Within the PHR National Student Advisory Board, the Asylum and Refugee Committee is tasked with guiding nascent student-run asylum clinics and with troubleshooting challenges that existing clinics are facing. Student-run organizations that perform forensic evaluations now exist at 19 medical schools across the US.9
The utility of forensic evaluations in asylum proceedings has been examined previously: in one study, 89% of US asylum seekers with legal representation who also received a PHR medical evaluation were granted protective status, far exceeding the national average of 37.5% among asylum seekers—with and without legal representation—who did not receive PHR evaluations.10 The impact of student-run asylum clinics, however, has not yet been documented. Here, we report the growth of the Weill Cornell Center for Human Rights (WCCHR), the first student-run organization to partner with PHR, and we share the results of the 2017 and 2018 national surveys of student-run asylum clinics that investigated caseloads, asylum evaluation trainings, clinician and student involvement, and operational challenges.
Methods
Study setting
The Asylum and Refugee Committee of the PHR National Student Advisory Board conducted two surveys of all student-run asylum clinics, including those affiliated and not affiliated with PHR, across the nation; the first was administered from September to December of 2017 and the second over the same time interval in the following year. Clinics were emailed a link to the online, standardized questionnaire. Data was collected for the preceding year and for the clinic’s entire history. The survey sought to evaluate the impact of student-run asylum clinics and to identify ways that clinics could improve the services offered to clients. The Institutional Review Board at Yale University was consulted and concluded that the data obtained by this study did not constitute human subjects research.
Questionnaire design
The survey (included here as an appendix) contained queries that addressed several topics: caseloads, client outcomes, asylum-evaluation trainings, active clinician and student involvement, and challenges faced. Regarding caseloads, the survey asked for the total number of forensic evaluations performed and the number of clients evaluated in the preceding year and since a clinic’s inception; the numbers of physical, psychological, and gynecological evaluations performed in the preceding year and throughout the clinic’s history; the number of evaluations performed in detention facilities; and the volume of forensic-evaluation requests received compared to the organization’s capacity to perform evaluations.
The number of evaluations performed by a clinic may not equal the number of clients served for two reasons: Firstly, some clients require multiple types of evaluations. Secondly, certain clinicians may perform multiple types of evaluations for a client in the same session and the clinic may employ different conventions for how such evaluations are counted. These discrepancies were clarified during annual conference calls with each clinic as part of a quality-improvement initiative administered by the Asylum and Refugee Committee. Additionally, a convention was adopted wherein the total number of evaluations performed by a clinic was calculated as the sum of the numbers of physical, psychological, and gynecological evaluations performed.
The survey’s section on client outcomes requested information about the number of cases granted and denied asylum or other forms of legal protection. Clinics were asked to report the number of asylum evaluation trainings and the numbers of clinicians and students trained in 2016 or 2017 and since the organization’s founding. Finally, clinics were asked to provide the number of clinicians and students involved in performing forensic evaluations. In the second survey, administered in 2018, clinics were asked whether they provided services in addition to forensic evaluations and whether recent legislative changes had affected their operations. No incentives were offered for participation.
Statistical analysis
Categorical variables are reported as counts and percentages, and continuous variables as means and standard errors. The linear least squares method was employed to identify the best-fit quadratic curve that estimates the rate of growth in the WCCHR’s capacity to perform evaluations. All calculations were performed by using Mathematica (Version 10.1; Wolfram).
Results
The Weill Cornell Center for Human Rights: A case study
The WCCHR is the first student-run asylum clinic to collaborate with PHR. Since its founding in 2010, the WCCHR has trained 386 clinicians and 845 students to conduct forensic medical evaluations of asylum seekers. The trainings with the largest attendance were held in 2017 and 2018. Strikingly, the number of clinicians trained in 2017 was nearly fourfold greater than the number trained in 2016 (Figure 1a).
The WCCHR has performed a total of 553 evaluations for 479 clients from 7/14/2010 through 5/4/2019. Because some clients require multiple types of evaluations, the number of evaluations performed exceeds the number of clients evaluated. Plotting the cumulative number of evaluations performed versus time yields a curve with a rising slope, reflecting the clinic’s expanding capacity to perform evaluations (Figure 1b). In contradistinction, a constant slope would be seen for an unchanging number of evaluations performed per unit time. The change in the curve’s slope, calculated as the second derivative of the best-fit quadratic curve, estimates that each year the WCCHR performs on average nine evaluations more than the number performed in the previous year. However, the rate of increase observed for 2019 so far exceeds this estimate.
Tabulating the number of evaluations performed annually by the WCCHR again demonstrates the clinic’s expanding capacity (Figure 1c). On average, the number of evaluations performed in a year increased by 12 cases, corresponding to an average annual growth of 40%. Assuming that the volume of cases remains constant throughout the year, the WCCHR is projected to perform 145 evaluations in 2019.
Forty-six percent of the clients evaluated by the WCCHR were men, 53% were women, and 1% were transgender. The average age of a client was 31 (age range was three to 65). The WCCHR offers three types of evaluations: 27% of the evaluations performed were physical, 65% psychological, and 8% gynecological. Clients most frequently hailed from Central America (38.2% of clients), Africa (26.9%), South America (12.9%), and Asia (11.9%), with the greatest numbers of clients coming from Honduras (n=72 clients), El Salvador (n=60), and Guatemala (n=37) (Figure 1d). The most common ground for claiming asylum was membership in a particular social group (78.7% clients), followed by political opinion (35.9%), religion (8.8%), race (5.6%), and nationality (3.6%). Of the clients whose cases were adjudicated, 95% received asylum or another form of legal protection. Immigration courts in New York decided the vast majority of these cases and had the highest rate of granting asylum or other legal protection in 2018 (Figure S1a) and with the third-largest backlog of pending immigration cases in the same year (Figure S1b).11
Figure 1
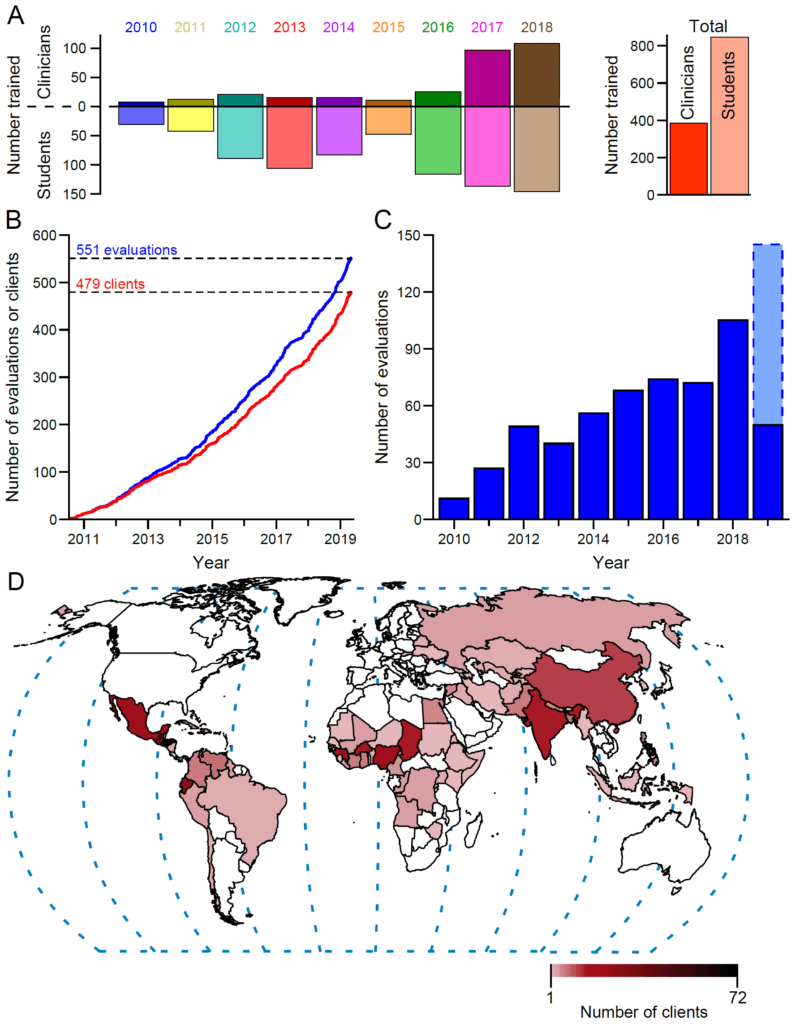
(a) Numbers of clinicians and students trained by the WCCHR each year (left) and in total (right). The upright, darkly shaded bars in the left panel show the numbers of clinicians trained, whereas the downward, lightly shaded bars show the numbers of students trained.
(b) Cumulative number of clients seen (red) or forensic evaluations performed (blue) by the WCCHR from 7/14/2010 through 5/4/2019.
(c) Number of evaluations performed annually by the WCCHR. The lightly shaded bar with the dashed border indicates the projected number of evaluations for 2019.
(d) Map showing the 74 countries from which the WCCHR’s clients fled to seek asylum in the United States. Darker shades indicate greater numbers of clients from those countries; white indicates that no clients were seen from those countries. The color bar indicates the range of the number of clients seen.
National trends in clinic caseloads and outcomes
Of the 15 clinics contacted in 2017, 14 responded, whereas 15 of 18 clinics contacted in 2018 responded (Figure 2a). Between 2017 and 2018, two new organizations were founded and one existing clinic was identified; all three were added to the list of surveyed clinics in 2018. Two clinics that responded in 2017 did not respond in 2018. Complete caseload data were obtained by both the 2017 and 2018 surveys for 11 clinics. In 2016, these 11 clinics performed a total of 227 evaluations for 192 individual clients: 87 (38%) of the evaluations were physical, 122 (54%) were psychological, and 18 (8%) were gynecological. Fifteen evaluations were performed in detention centers. The same 11 clinics completed 315 evaluations for 275 clients in 2017. The number of evaluations performed thus grew by 38.8% or by an average of 8 ± 3 cases per clinic over the preceding year, and the number of clients served grew by 43.2% (Figure 2b). Nine clinics performed more evaluations in 2017 than in 2016, whereas two clinics performed fewer evaluations. One hundred and fifty (48%) of the 2017 evaluations were physical evaluations, 130 were psychological (41%), and 35 (11%) were gynecological (Figure 2c, inset). Compared to the 2016 data, these figures constitute an increase in physical evaluations by 72.4%, an increase in psychological evaluations by 6.6%, and an increase in gynecological evaluations by 94.4% (Figure 2c). Thirty-one evaluations were performed in detention centers in 2017, more than double the number performed in 2016. In both years, nine clinics served clients who required multiple types of evaluations. Several entities referred forensic evaluation requests to clinics, including PHR, non-profit organizations, law clinics, and attorneys.
To date, student-run clinics have performed more than 1,600 evaluations, of which approximately 39% were physical evaluations, 52% were psychological evaluations, and 9% were gynecological evaluations. Ninety evaluations were completed at detention centers. Outcomes were reported for 774 clients: 754 clients (97.4%) were granted asylum or another form of legal protection, and 20 clients (2.6%) were denied asylum. The majority of student-run asylum clinics are located in states whose immigration courts grant asylum or other protections at a rate that exceeds the nation’s average grant rate (Figure S1a) and in states with long backlogs of pending immigration cases (Figure S1b).12
In 2016, half of the clinics stated that the volume of forensic evaluation requests received by their organization was commensurate with their capacity to perform evaluations, 33% claimed their capacity for forensic evaluations exceeded the number of requests they received, and 17% stated the forensic evaluation requests they received exceeded their organization’s capacity. By 2017, 50% of clinics received evaluation requests exceeding their organization’s capacity, 25% received evaluation requests commensurate with their organization’s capacity, and 25% of clinics’ capacity exceeded the number of requests (Figure 2d).
Figure 2
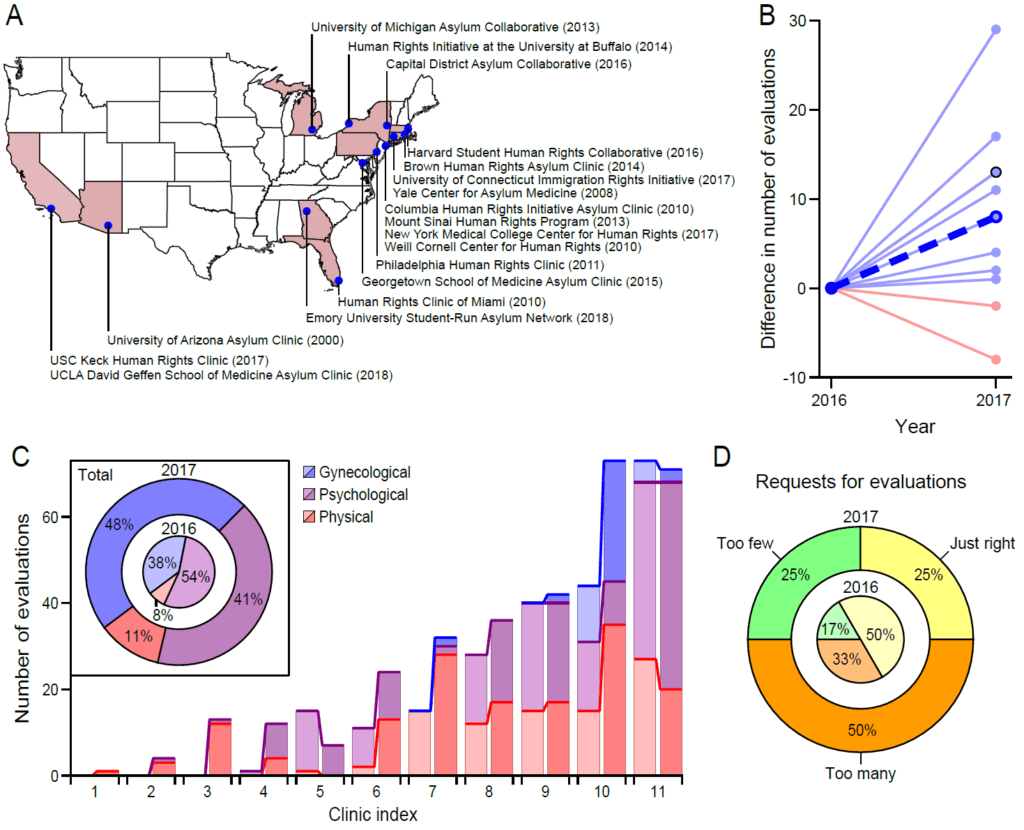
(a) Map showing the 18 active organizations that received the survey in 2018. The founding year of each clinic is listed in parentheses. Because they had not yet performed a forensic evaluation by the end of 2018, the student-run organizations at the Albert Einstein College of Medicine, CUNY School of Medicine/Sophie Davis, Geisel School of Medicine at Dartmouth, Touro College of Osteopathic Medicine, NYIT College of Osteopathic Medicine, and UTMB at Galveston are not shown.
(b) Differences in the numbers of evaluations performed between 2017 and 2016. Data is shown only for the eleven clinics from which complete training data were obtained for both surveys. Light-blue lines indicate an increase in the number of evaluations, whereas light-red lines indicate a decrease. The thick, blue, and dashed line represents the average difference across clinics. A black circle indicates that the same difference was obtained for two clinics.
(c) Bar chart depicting the numbers of each type of evaluation (physical, psychological, and gynecological) performed by each clinic. Light shades of each color correspond to data from 2016, and darker shades portray data from 2017. The inset displays the proportions of evaluation types among all evaluations performed in 2016 (inner circle) and in 2017 (outer circle).
(d) Pie chart showing the proportion of clinics that reported receiving a number of evaluation requests that exceeded the organization’s capacity (“too many”), receiving a number of evaluation requests that was commensurate with the organization’s capacity (“just right”), or having capacity that exceeded the number of received evaluation requests (“too few”). Data are shown for 2016 (inner circle) and for 2017 (outer circle).
National trends in asylum evaluation trainings
In 2016, five clinics held two trainings, three clinics held one training, and the remaining clinics held no trainings. In 2017, three clinics held two trainings, six clinics held one training, seven clinics held no trainings, and three clinics did not respond. Complete training data were obtained by both surveys for seven clinics; these clinics trained 76 clinicians and 186 students in 2016, and 377 clinicians and 337 students in 2017, reflecting a growth by 396% and 81% in the numbers of clinicians and students trained, respectively. On average, clinics trained 43.0 ± 16.6 more clinicians and 21.6 ± 7.2 students in 2017 than in 2016 (Figures 3a and 3b). To date, 12 clinics have together hosted 66 trainings that were attended by more than 1,400 clinicians and by more than 1,700 students in total. Moreover, nearly 400 clinicians and more than 1,000 students were reported to be actively involved in the clinics at the end of 2018.
Figure 3
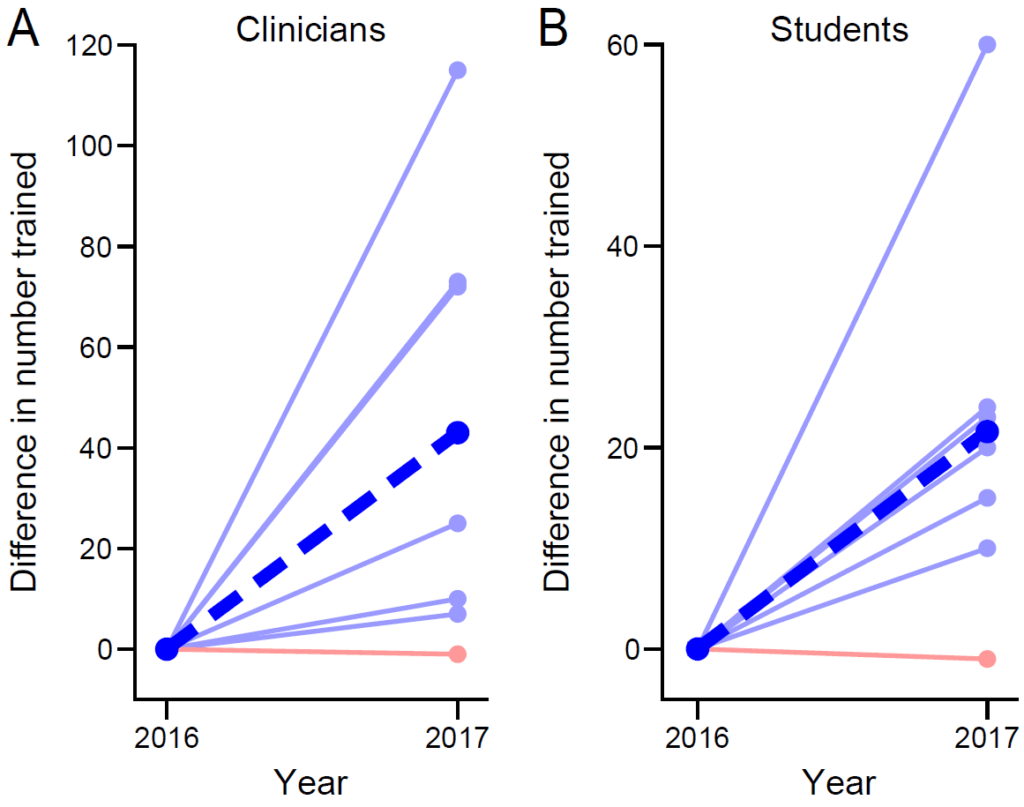
Differences in the numbers of clinicians (a) and students (b) trained between 2016 and 2017. Data is shown for only the seven clinics from which complete training data were obtained for both surveys. Light blue lines indicate an increase in the number of trainees, whereas light red lines indicate a decrease. The thick, blue, and dashed line represents the average difference across clinics.
Additional services offered by clinics
In 2018, a third of the clinics provided services in addition to forensic evaluations. Six clinics refer clients to local organizations that provide clients with pro bono or low-cost legal, medical, or psychological services. Other services included on-site social work and counseling for survivors of intimate-partner violence and sexual assault; a travel fund to help clients attend appointments; and financial assistance with clothing, food, and infant care necessities.
Challenges faced by nascent and established clinics
Challenges were shared by 13 respondents in 2017 and by 12 respondents in 2018. Most challenges were recurrently reported and were related to institutional difficulties, to recruitment or retention of clinicians, or to changes in national policies. Institutional obstacles included: gaining support from the medical school’s administration, finding physical spaces for evaluations, and answering questions about liability. Concerns around ensuring the continuity of services and around maintaining the organization’s knowledge across student-leadership transitions were also listed. Two clinics reported barriers to developing an apparatus that addresses clients’ ongoing medical and social needs. One of these clinics was unsure of how to implement such a framework without affecting the perceived objectivity of the forensic affidavits and evaluations.
Difficulties related to having enough volunteer clinicians were reported most commonly: six clinics (43% of respondents) in 2017 and six (40% of respondents) in 2018 cited such challenges. Specifically, some clinics had trouble attracting clinicians to training opportunities, recruiting clinicians to become active evaluators, or retaining trained clinicians. A shortage of mental health professionals to perform psychological evaluations was noted by two clinics in 2017 and by two different clinics in 2018. In 2017, one clinic reported having difficulty placing urgent evaluation requests—those needing to be completed within a short timeframe—with clinicians, an issue that arose for three clinics in 2018.
Two-thirds of clinics responded affirmatively to the question: “Have recent legislative changes affected the way in which your clinic operates?” Six clinics (40%) noted differences in how domestic violence or gang violence cases were handled by the organization or by legal partners. Four clinics (27%) connected rising caseloads to policy changes, with three of these clinics noting an increase in the number of urgent requests for evaluations. Two clinics saw diminished numbers of evaluation requests, and one of these clinics specifically reported having far fewer referrals for clients who were subjected to domestic violence.
Discussion
Forensic evaluation statistics
This study reports caseloads, training statistics, active involvement, and challenges for student-run asylum clinics. The growth experienced by the WCCHR augurs the trends seen for organizations across the nation. Eleven clinics performed 227 forensic evaluations in 2016 and 315 evaluations in 2017, reflecting a growth in capacity by 38.8%. By comparison, PHR conducted 520 evaluations in 2016 and 670 evaluations in 2017, representing growth by 28.8%.13 Considering that PHR is one of the largest providers of evaluations in the nation, these figures suggest that student-run clinics will soon manage the majority of requests for forensic medical evaluations. This prediction is further supported by the close agreement seen between the WCCHR’s average annual growth rate (40%) and the growth rate averaged over 11 clinics in various stages of development (38.8%). The WCCHR’s experiences are likely typical, and student-run asylum clinics in urban centers can expect to follow a similar trajectory. Greater capacities to accommodate evaluation requests are urgently needed as the number of asylum claims filed in the US continues to rise each year: in 2017, the US Citizenship and Immigration Services (USCIS) reported 139,801 affirmative asylum applications, surpassing the 2016 number by 21%.14
Greater numbers of all evaluation types—physical, psychological, gynecological, and those conducted in detention facilities—were performed in 2017 than in 2016. That the number of psychological evaluations grew by only 6.6% might reflect the challenge of recruiting mental health professionals that was cited by several clinics. Various studies place the rates of post-traumatic stress disorder in asylum seekers at different percentages ranging from 20% to 80%.15 The psychological harm that has befallen asylum seekers may impair their ability to recall facts or to coherently recall their experiences. Mental health professionals and physicians who routinely perform psychological assessments provide diagnostic information to support applicants’ claims of psychological harm, thereby enhancing a claimant’s credibility.16 The expertise of mental health professionals is needed with even greater urgency following the implementation of Executive Order 13767 in 2017 and the higher standard for “credible fear” of persecution therein established.17 Under this order, asylum applicants—the legitimacy of their claim notwithstanding—whose trauma has altered their “demeanor, candor, or responsiveness” may now be perceived as less credible.18
The doubling in the number of evaluations performed in detention centers by student-run clinics might be driven by the current administration’s 2017 policies of detaining undocumented immigrants and of increasing the capacity of detention facilities to 48,000 detainees per day.19 The administration’s implementation of ‘expedited deportation’ policies in 2017 has also contributed to the backlog of pending immigration court cases.20 Many asylum seekers now face prolonged detentions that span months or even years owing to longer waiting periods between an applicant prevailing in a credible-fear interview and subsequently appearing in immigration court.21 Obtaining access to detention centers to conduct evaluations remains critical for ensuring a fair adjudication process for asylum seekers.
Of the clients whose cases were adjudicated, asylum or another form of legal protection was received by 95% of clients seen by the WCCHR and by 97.4% of clients seen by all of the student-run clinics, numbers that closely agree. These grant rates accord with those reported elsewhere, suggesting that evaluations performed through student-run asylum clinics are non-inferior to those performed by independent clinicians.22 Obtaining outcomes data is limited, however, by several factors. The long delays in immigration proceedings hinder a clinic’s ability to track results: individuals with open immigration cases—including asylum seekers—have already been awaiting a decision for 727 days on average.23 Moreover, those denied asylum may appeal and subsequently prevail in their asylum case. Other limitations to accurately measuring asylum outcomes include non-response bias and missing data. Because asylum grant rates vary widely across states, the rates found in this study may not be attainable by every organization.
Training statistics
Between 2016 and 2017, the numbers of clinicians trained by the WCCHR and by seven student-run asylum clinics increased nearly fourfold and fivefold, respectively. The number of students trained also increased over this time period. Asylum evaluation trainings are typically held in September, October, and early spring. The trainings hosted by student-run clinics in 2016 therefore occurred before the 2016 presidential election, whereas the 2017 trainings followed the presidential inauguration. The WCCHR held a training in February 2017 that was—at the time—the largest in the organization’s history. The rhetoric surrounding the 2016 election appears to have spurred student-run asylum clinics to broaden their recruitment strategies and to have galvanized clinicians into leveraging their training to assist asylum seekers.24
More than 1,400 clinicians and 1,800 students have attended one of 66 trainings hosted by student-run organizations. Asylum clinics retain only a fraction of trainees, however: nearly 400 clinicians and approximately 1,000 students were actively involved in performing forensic evaluations by the end of 2018. Moreover, the need for more trained clinicians to meet the demand for forensic evaluations was the most commonly faced challenge reported by clinics. Clinicians with expertise evaluating minors are increasingly needed: unaccompanied children account for half of the affirmative-asylum applicants from Central America, and this proportion is expected to grow.25 Expanding opportunities for health care professionals to attend trainings remains integral to the continued growth of clinics nationwide.
Current political context and asylum law
Settled law that offers asylum to certain groups, particularly those claiming persecution due to domestic and gang violence, has been rolled back and challenged by the US Department of Justice. The Board of Immigration Appeals in 2014 held that “married women in Guatemala who are unable to leave their relationship” are a particular social group for purposes of obtaining asylum and withholding of removal.26 On June 11, 2018, Former Attorney General Jeff Sessions issued a decision, Matter of A-B-, that advised immigration officials to summarily deny credible-fear hearings for domestic violence or gang-related claims. Although the attorney general acknowledged the severity of the harms suffered, he questioned whether these survivors are recognized within their society as a particular social group.27 The proportion of asylum seekers granted protection from the Northern Triangle countries of Central America rose from 14% in 2010 to 27% in 2016, reflecting immigration officials’ recognition of the dangerous conditions—including powerful gangs and rampant gender-based violence—pervading the region. Owing to concerted efforts by the Trump Administration to limit asylum eligibility, this upward trend reversed course: grant rates for asylum applicants from Central America declined by 40% between 2017 and 2018.28 Consistent with these changes, several respondents (40%) noted differences in how domestic violence and gang violence cases were managed by the organization or by attorneys.
Starting on January 29, 2018, USCIS changed the way asylum claims were adjudicated by prioritizing the most recently filed affirmative asylum applications when scheduling interviews.29 This compressed timeline can increase stress for applicants as they attempt to gather documents quickly, and it also likely accounts for the increase in urgent evaluation requests reported by three clinics.
Student-run asylum clinics: Challenges and benefits
Respondents indicated that many of the greatest challenges were encountered in establishing a clinic. Particular difficulties at the outset included: addressing risk management, receiving institutional support, transitioning student leaders, recruiting clinicians, and acquiring funding. To help anticipate and preemptively address these challenges, members of the PHR National Student Advisory Board compiled the collective wisdom of several clinics into a guide that delineates the critical steps in founding and operating a student-run clinic.30 The board’s Asylum and Refugee Committee stands ready to offer additional advice, share resources, and connect organizations beset by obstacles to clinics that have overcome similar challenges. The successes of the clinics showcased in this study demonstrate that the barriers to starting a clinic are surmountable, a fact that may allow students to garner support from their institutions as they endeavor to open new clinics.
A student-run asylum clinic’s value extends beyond providing forensic medical evaluations and hosting asylum evaluation trainings.31 Through referral networks, clinics connect clients to local organizations that provide low-cost or pro bono medical and social services. By pooling resources and by serving as an organizational hub, an asylum clinic can surpass the number of evaluations performed by independent clinicians and can accommodate tighter deadlines. Moreover, a clinic manages the details of scheduling evaluations. Thus relieved of these logistical burdens, clinicians can focus their time on performing evaluations. Clinics across the nation ascribe to a common set of policies and procedures that were developed with oversight from PHR to ensure the uniform application of acceptable standards of practice. Notably, the affidavit of a first-time evaluator must receive feedback from an experienced evaluator before the document is submitted to a client’s attorney. Education is central to the mission of the student-run asylum clinic. By participating in evaluations and in affidavit writing, students interact with highly vulnerable populations, develop cross-cultural competence, learn how to recognize and document signs of torture, practice trauma-informed interviewing, and become acquainted with ways that clinicians can leverage their training to help those in need outside of providing medical care. Students involved in the clinic’s operation also gain leadership experience. Conversely, volunteer clinicians are afforded the opportunity to train and mentor students who are passionate about human rights. A clinic can enhance the entire community’s awareness of human rights issues through lecture series and can rapidly mobilize many voices through advocacy initiatives. Several organizations have also engaged in broader conversations by developing robust research programs, as is evidenced by the diverse topics presented at the annual PHR National Student Conference.32
Conclusion
In August 2019, the backlog of immigration cases in the US soared to more than 1,000,000, a figure that underscores the immense need for forensic evaluations of asylum seekers.33 Our study demonstrates a rapid expansion in the collective capacity of student-run asylum clinics to provide evaluations. More than 1,500 evaluations have been conducted by 18 student-run asylum clinics nationwide, a testament to the hard work of the students and clinicians who make these organizations possible. This encouraging trend reveals a growing interest among health care professionals in offering services to asylum seekers and predicts that student-run asylum clinics will soon provide a significant proportion of urgently needed evaluations. With the help of the PHR National Student Advisory Board, the number of asylum clinics continues to grow annually, and each clinic becomes better equipped to accept more evaluation requests.
Acknowledgments
We gratefully acknowledge Kelsey Young, Ryan Lion, and Nicole Aguirre for assisting with data collection, and the Weill Cornell Center for Human Rights for sharing detailed data sets. A.R.M. is supported by National Institutes of Health Grants F30DC015697 and T32GM07739.
Madison B. Sharp* is an MD candidate at the Yale School of Medicine, New Haven, CT, USA and Co-Chair of the Physicians for Human Rights National Student Advisory Board.
Andrew R. Milewski*, PhD, is an MD-PhD candidate at the Weill Cornell/Rockefeller/Sloan-Kettering Tri-Institutional MD-PhD Program, New York, NY, USA; Co-Chair Emeritus of the Physicians for Human Rights National Student Advisory Board; and Co-Executive Director Emeritus of the Weill Cornell Center for Human Rights.
Claire Lamneck, MPH, is an MD candidate at the University of Arizona College of Medicine, Tucson, AZ, USA, and a member of the Refugee and Asylum Committee of the Physicians for Human Rights National Student Advisory Board.
Katherine McKenzie, MD, FACP, is Assistant Professor of Medicine in the Department of General Internal Medicine, Yale School of Medicine, New Haven, CT, USA, and Director of the Yale Center for Asylum Medicine.
* Madison B. Sharp and Andrew R. Milewski are joint first authors
Please address correspondence to Katherine McKenzie. Email: katherine.mckenzie@yale.edu.
Competing interests: Dr. McKenzie is a long-term volunteer for Physicians for Human Rights and HealthRight International. She was paid less than $300 for each of two PHR trainings conducted in 2015 and 2016. When she provides asylum detention evaluations for American Friends Service Committee, her travel expenses are compensated. She was paid less than $500 in travel expenses to present grand rounds at Stony Brook University.
Copyright © 2019 Sharp, Milewski, Lamneck, and McKenzie. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- United Nations High Commissioner for Refugees, Asylum trends 2014: Levels and trends in industrialized countries (Geneva: UNHCR, 2015).
- United Nations High Commissioner for Refugees (2015, see note 1); United Nations High Commissioner for Refugees, Global trends: Forced displacement in 2017 (Geneva: UNHCR, 2018).
- United Nations High Commissioner for Refugees (2018, see note 2).
- Ibid.; TRAC Immigration, Immigration court backlog tool: Pending cases and length of wait by nationality, state, court, and hearing location. Available at https://trac.syr.edu/phptools/immigration/court_backlog/.
- Department of Homeland Security, Granted asylum affirmatively or defensively: Fiscal years 1990 to 2017 (Washington, DC: DHS, 2019); S. L. Lustig, S. Kureshi, K. L. Delucchi, et al., “Asylum grant rates following medical evaluations of maltreatment among political asylum applicants in the United States,” Journal of Immigrant and Minority Health 10/1 (2008), pp. 7-15; TRAC Immigration, Asylum decisions and denials jump in 2018. Available at https://trac.syr.edu/immigration/reports/539/; TRAC Immigration, Relief granted by immigration judges as of May 2019. Available at https://trac.syr.edu/phptools/immigration/court_backlog/apprep_relief.php.
- United Nations High Commissioner for Refugees, Istanbul Protocol: Manual on the effective investigation and documentation of torture and other cruel, inhuman or degrading treatment or punishment (Geneva: UNHCR, 2004).
- E. Scruggs, T. C. Guetterman, A. C. Meyer AC, et al., “ ‘An absolutely necessary piece’: A qualitative study of legal perspectives on medical affidavits in the asylum process,” Journal of Forensic and Legal Medicine 1/44 (2016), pp. 72-78; H. Ferdowsian, K. McKenzie, and A. Zeidan, “Asylum medicine: Standard and best practices,” Health and Human Rights Journal 21/1 (2019), pp. 215.
- E. Emery, C. Stellar, K. Dubin, et al., “Student leadership in the creation and operation of an asylum clinic,” Health and Human Rights Journal (2015). Available at https://www.hhrjournal.org/2015/11/student-leadership-in-the-creation-and-operation-of-an-asylum-clinic/; K. Chelidze, N. Sirotin, M. Fabiszak, et al., “Documenting torture sequelae: the Weill Cornell model for forensic evaluation, capacity building, and medical education,” in B. N. Lawrence and G. Ruffer (eds), Adjudicating refugee and asylum status: The role of witness, expertise, and testimony (New York: Cambridge University Press, 2015), pp. 166–179; N. Praschan, R. Mishori, and N. Stukel, “A student-run asylum clinic to promote human rights education and the assessment and care of asylum seekers,” Journal of Student-Run Clinics 2/2 (2016); S. G. Carbrey, B. Cesar, A. Chava, et al., “The value of medical students in support of asylum seekers in the United States,” Families, Systems, and Health: The Journal of Collaborative Family Healthcare 36/2 (2018), pp. 230–232.
- Ferdowsian et al. (see note 7).
- Lustig et al. (see note 5).
- TRAC Immigration (see note 4); TRAC Immigration, Asylum decisions by custody, representation, nationality, location, month and year, outcome and more. Available at https://trac.syr.edu/phptools/immigration/asylum/.
- Ibid.
- Physicians for Human Rights, Securing justice: Physicians for Human Rights annual report 2016 (New York: PHR, 2017). Available at https://phr.org/wp-content/uploads/2018/09/ phr-2016-annual-report.pdf; Physicians for Human Rights, Through evidence, change is possible; Physicians for Human Rights annual report 2017 (New York: PHR, 2018). Available at https://s3.amazonaws.com/PHR_Reports/PHR_2017_Annual_Report.pdf.
- N. Mossaad, Annual flow report refugees and asylees: 2017 (Washington, DC: Department of Homeland Security, March 2019).
- K. Lee, “Seeking sanctuary,” Monitor on Psychology 48/7 (2017), pp. 38. Available at https://www.apa.org/monitor/2017/07-08/sanctuary.
- K. C. McKenzie, J. Bauer, and P.P. Reynolds, “Asylum seekers in a time of record forced global displacement: The role of physicians,” Journal of General Internal Medicine 34/1 (2019), pp. 137–143; K. Baker, K. Freeman, G. Warner, and D. M. Weissman, Expert witnesses in U.S. asylum cases: A handbook (Chapel Hill: University of North Carolina at Chapel Hill, School of Law, 2018); S. M. Meffert, K. Musalo, D. E. McNiel. and R. L. Binder, “The role of mental health professionals in political asylum processing,” The Journal of the American Academy of Psychiatry and the Law 38/4 (2010), pp. 479–489.
- US Citizen and Immigration Services, Credible fear FAQ. Available at https://www.uscis.gov/faq-page/credible-fear-faq#t12831n40220.
- Baker et al. (see note 14); US Citizen and Immigration Services, Credible fear FAQ (see note 17).
- Human Rights First, Tilted justice: Backlogs grow while fairness shrinks in U.S. immigration courts (Washington, DC, and New York: Human Rights First, 2017). Available at https://www.humanrightsfirst.org/sites/default/files/hrf-tilted-justice-final%5B1%5D.pdf.
- Preston and A. R. Calderon, “Trump tried to deport people faster. Immigration courts slowed down instead,” The Marshall Project (July 2019). Available at https://www.themarshallproject.org/2019/07/16/trump-tried-to-deport-people-faster-immigration-courts-slowed-down-instead.
- Human Rights First (2017, see note 19).
- Emery et al. (see note 8); Lustig et al. (see note 5); R. Asgary, P. Saenger, L. Jophlin, and D. C. Burnett, “Domestic global health: A curriculum teaching medical students to evaluate refugee asylum seekers and torture survivors,” Teaching and Learning in Medicine 25/4 (2013), pp. 348–357.
- TRAC Immigration (Immigration court backlog tool, see note 4).
- G. Reich, “Hitting a wall? The Trump Administration meets immigration federalism,” Publius: The Journal of Federalism 48/3 (2018) pp. 372–395.
- Human Rights First (2017, see note 19).
- U. S. Department of Justice, Matter of A-R-C-G- et al., Respondents (August 26, 2014). Available at https://www.justice.gov/sites/default/files/eoir/legacy/2014/08/26/3811.pdf.
- U. S. Department of Justice, Matter of A-B-, Respondent (June 11, 2018). Available at https://www.justice.gov/eoir/page/file/1070866/download.
- Human Rights First, Central Americans were increasingly winning before President Trump took office (January 2019). Available at https://www.humanrightsfirst.org/resource/central-americans-were-increasingly-winning-asylum-president-trump-took-office.
- U. S. Citizenship and Immigration Services, Affirmative asylum interview scheduling (January 2018). Available at https://www.uscis.gov/affirmative-asylum-scheduling.
- Physicians for Human Rights National Student Program, The asylum clinic guide. Available at https://www.phrstudents.com/how-to-efficiently-run-an-asylum-pr.
- Emery et al. (see note 8), Chelidze et al. (see note 8), Praschan et al. (see note 8), Carbrey et al. (see note 8).
- Physicians for Human Rights National Student Program, 2017 national conference poster archive. Available at https://www.phrstudents.com/2017-national-conference-posters; Physicians for Human Rights National Student Program, 2018 national conference poster archive. Available at https://www.phrstudents.com/2018-national-conference-posters.
- TRAC Immigration (Immigration court backlog tool, see note 4).
Appendix
Figure S1. Asylum decisions and backlogs by state

(a) Map showing the statewide rate at which immigration courts granted applicants asylum or another form of legal protection in 2018. This data, taken from TRAC, contains both affirmative and defensive applications decided by immigration courts, but excludes applications decided by USCIS. Darker shades of blue correspond to higher rates along a linear scale as indicated by the color bar. Rates range from 5.5% to 65.6%, the median rate is 21.1%, the national rate across all decisions is 34.7%, and averaging the statewide rates yields 27.8%.
(b) Map showing the backlog of pending cases in the immigration courts by state as of October 2019. Darker shades of red correspond to larger backlogs along a logarithmic scale as indicated by the color bar. In both panels, tan indicates states without immigration courts and striped states are home to student-run asylum clinics that are marked by red (a) or blue (b) dots. Data for both panels were taken from the sources listed in reference 11 of the main text.
Student-Run Asylum Clinic Impact Survey
- My organization consents to allowing the PHR Student Advisory Board to pool the information we provide through this survey to create and disseminate a report that evaluates the impact of student-run asylum clinics:
- My organization consents
- My organization does not consent
- Your Organization’s Information
- Name of your organization:
- Contact email for your organization:
- In what year was your organization founded?
- What are your organization’s primary sources of forensic evaluation requests?
- Clinic Caseload
- How many forensic evaluations did your organization perform in 2017?
- Of those, how many were physical evaluations?
- How many were psychological evaluations?
- How many were gynecological evaluations?
- How many were performed in detention facilities (including detention centers, jails, etc.)?
- Did your clinic perform any other type of forensic evaluation in 2017? If so, what types and how many?
- Examples include, but are not limited to, dental evaluations, radiographic imaging for forensic purposes, medical record reviews, evaluating whether medical treatments in other countries would be effective for certain conditions (i.e. HIV).
-
- How many clients did your organization evaluate in 2017?
- Some clients may receive multiple evaluations; we therefore also want to know how many individual clients your organization has seen.
-
- How many forensic evaluations has your organization performed since it was founded?
- Of those, how many were physical evaluations?
- How many were psychological evaluations?
- How many were gynecological evaluations?
- How many were performed in detention facilities (including detention centers, jails, etc.)?
- Has your clinic performed any other type of forensic evaluation? If so, what types and how many?
- Examples include, but are not limited to, dental evaluations, radiographic imaging for forensic purposes, medical record reviews, evaluating whether medical treatments in other countries would be effective for certain conditions (i.e. HIV).
-
- How many clients has your organization evaluated since it was founded?
- Some clients may receive multiple evaluations; we therefore also want to know how many individual clients your organization has seen.
-
- How does the volume of forensic evaluation requests received by your organization compare with its capacity to perform evaluations?
- The number of forensic evaluation requests we receive exceeds our organization’s capacity.
- The number of forensic evaluation requests we receive is commensurate with our organization’s capacity.
- Our organization’s capacity for forensic evaluations exceeds the number of requests we receive.
- Client Outcomes
- Of the clients whose cases have been adjudicated, how many have been granted asylum or another form of legal protection?
- Of the clients whose cases have been adjudicated, how many were denied asylum or other forms of legal protection?
- Asylum Evaluation Trainings
- How many asylum evaluation trainings did your organization hold in 2017?
- How many clinicians did your organization train in 2017 to perform forensic evaluations?
- How many students did your organization train in 2017 to participate in forensic evaluations?
- How many total asylum evaluation trainings has your organization held?
- How many total clinicians has your organization trained to perform forensic evaluations?
- How many total students has your organization trained to participate in forensic evaluations?
- Current Involvement
- How many clinicians are currently involved in performing forensic evaluations with your organization?
- How many students are currently involved in performing forensic evaluations with your organization?
- Does your clinic provide services in addition to forensic evaluation?
- Yes
- If yes, please give a short description:
- No
- Challenges
- Has your clinic faced any challenges during the past year? If so, was your organization able to address those challenges? Would you like to discuss any of these challenges with other student-run asylum clinics?
- Would your organization be interested in participating in another summit for student-run asylum clinics like the event hosted by Cornell in May of 2017?
- Yes
- No
-
- Have recent legislation changes affected the way in which your clinic operates?
- Yes
- If yes, in what ways?
- No
- Questions
- Do you have any questions for the PHR Student Advisory Board’s Asylum Committee at this time?
