Aquiles Ignacio Arrieta-Gómez
Abstract
Colombia has made significant progress in the recognition and protection of the right to health. Using litigation—a structural element of the democratic Colombian design—many people have had to fight in order to enjoy effective access to health care. Such litigation has proven a pacific and democratic way to protect a constitutional principle: health as a fundamental and justiciable right. In 2008, in the wake of thousands of individual rulings on the right to health, Colombia’s Constitutional Court issued a structural decision, T-760 of 2008, ordering government entities to identify flaws that made the country’s health system outdated and inequitable and to take correctional measures. In the years following this decision, Congress and the executive branch have increasingly included a rights-oriented perspective in public policies. The Colombian case reveals judicial intervention as a legitimate way to extend pressure on the government to act according to constitutional boundaries. Although there is still a long road ahead, public institutions responsible for health care are now on a constitutionally acceptable track.
After many political and judicial debates in light of the 1991 Constitution, Colombia passed a statutory law in 2015 (Law 1751) recognizing the constitutional right to health.[1] This law was the result of a long battle between those who consider health a fundamental right that is enforceable by the courts and those who claim that health is a social right that should instead be addressed through public policies set by the legislative and executive branches. This battle has taken place in one of the oldest uninterrupted constitutional jurisdictions.[2] This law was also the result of thousands of judicial decisions on the right to health issued over the span of more than two decades, especially Decision T-760 of 2008 in which the Colombian Constitutional Court ordered a restructuring of the health system. The purpose of this paper is to outline this constitutional process of change in Colombia and explore the role of judges in promoting the effective enjoyment of the right to health, mainly through structural orders.
First, it is worth highlighting the research to date on the impacts of judicial remedies. The literature on the justiciability of social rights has focused mainly on the implementation and impacts of structural judgments.[3] Debate over these impacts is relevant because in social rights cases, it is important to determine not just whether a right is being violated but also what to do to address the violation. It is a complex task to recognize both a good judicial order and a suitable process of enforcement. Some scholars have commented that judicial opinions, besides having a direct impact through the adopted remedies, can also have indirect and even symbolic impacts.[4]
There has been much academic debate about the impact of Decision T-760 of 2008, but we do not yet have adequate tools to settle this dispute. For example, César Rodríguez-Garavito has argued that along with Mark Tushnet’s two criteria—the strength or weakness of judicial measures in terms of the scope of the orders and the degree of obligation—the type of compliance with the measures chosen by the court must also be taken into account.[5] It could also be argued that the number of interests involved in and affected by a judicial decision, whether directly or indirectly, is a critical measure of a decision’s impact. For instance, the protection of the rights of persons in a situation of displacement involves a particular part of society, the people close to them (family, friends, and so forth), and the authorities and organizations that deal with displacement. In contrast, the protection of the fundamental right to access health services affects all people in a given country, as well as all health providers and other stakeholders in the sector. In the first case (displacement), it is easier to enforce a court’s orders, while in the second (health services), it is much more complex. The number of actors involved in the case and their relative power affects compliance with the court’s judgment.
In this sense, the degree of resistance to the fulfillment of judicial orders varies between a scenario in which broad public and private interests (both national and international) are at stake and one in which the work and autonomy of smaller sectors of the local bureaucracy are at issue. This difference in contexts affects the measures that a court must order and the intensity with which it must demand compliance. It also affects the degree of the counter-majoritarian objection and the level of self-restraint that is expected of the judge. This last criterion of analysis is crucial to determining the real impact and advantages of structural rulings such as T-760 of 2008 in Colombia. As will be shown, the Uribe administration (2002–2010) tried to overrule the structural orders of that ruling, declaring a state of economic and social emergency and using exceptional executive powers to change the legal framework. Later, under the Santos administration (2010–2018), the minister of health and social protection, Alejandro Gaviria, has had to deal with the pharmaceutical industry to comply with orders to ensure access to medicines that people require.
The first part of this paper presents the history and context of the right to health in Colombia and the structural remedies adopted by the Constitutional Court in response to thousands of individual judicial orders. The second part presents some achievements and setbacks after the structural judicial intervention (T-760 de 2008). The final section draws some conclusions.
The foundations of the right to health in Colombia and individual lawsuits as a tool for access
After more than 200 years, it is clear that the separation of public powers is not enough warranty against abuses. Nor is the detailed enumeration of the faculties of those who hold authority. What is missing is to attribute power to the citizens and create mechanisms for them to exercise it directly, peacefully … : transfer power to the regular citizen so that when he or she has been treated arbitrarily, that person has an alternative to aggression, incendiary protest or submissive and alienating resignation … That a single mother may ask the judge to order a school to promptly admit her son and cease discrimination against him. That medical care could not be denied to a poor person whose life is in danger, and a judge could order a hospital to provide immediate assistance to him … In short, let arbitrariness cease.
President César Gaviria, National Constituent Assembly, February 5, 1991
As mentioned above, the acceptance of health as a fundamental right in a 2015 statutory law enacted by Congress was the end of a long road of legal battles. The principal tool for realizing health as a fundamental constitutional right in Colombia has been individual litigation in the form of the tutela (writ of protection). Since the 1992 creation of the Constitutional Court, tutelas have been used by thousands of people to make claims regarding specific medical needs and to secure access to relevant health services. Through the tutela, individuals (or their relatives, friends, or lawyers) judicially claim their right to health in connection with their rights to life and dignity. Although the justiciability of the right to health was under debate by scholars and political leaders in the early 1990s, this kind of litigation was expected and common. Citizen litigation had become a structural part of the Colombian democratic design: to judicially claim a constitutional right is as political and democratic an action as going to the polls or forming a political party.[6] Citizens were making use of their new constitutional powers.
At the end of 1993, through Law 100, Congress created the foundations of an “integral social security system” based on the principles of efficiency, universality, solidarity, integrality, unity, and participation (art. 2). Law 100, among other things, created a new health system for the country; this system was a mixed one, governed by the state, that included the participation of both public and private health care providers. The system was divided into two regimes: a contributory regime that provided full coverage to those who made financial contributions directly to the system, and a subsidized regime that provided partial coverage to those who did not contribute directly because of their low income. The contributory regime had access to all of the services included in the country’s benefits plan, while the subsidized had access to only some of them. This differentiation was temporary in order to allow the system to become financially viable (art. 162 of Law 100). For the contributory regime, the Constitutional Court held that health care providers were constitutionally obliged to guarantee access to required medical services and had the right to collect the cost of the services that were not covered by the benefits plan (then known as the Plan Obligatorio de Salud and today entitled the Plan de Beneficios en Salud). The order in these cases was “to take measures” within 48 hours to authorize the required medical service. For the subsidized regime, it held that health care providers were constitutionally obliged to inform, guide, and accompany patients in securing the required medical service through the public network and local authorities.[7] In 2000, the government extended the court’s protection, requiring institutions of the subsidized regime to deliver directly to patients any necessary medicines that fell outside the benefits plan (as in the contributory regime) and to collect reimbursement from the state (through local authorities) if necessary.[8] In 2001, the Constitutional Court decided to grant the same protection to children regardless of which regime they were enrolled in.[9]
The first years of the 21st century were bittersweet. On one hand, the court finally unified the rules for cases concerning health services not covered. People and institutions had certainty regarding what the outcome of their claim would be and which tutela judicial order would be enforced.[10] But at the same time, different actors from the health system (some insurers, some providers, and even some patients) started to take advantage of the executive and administrative regulations and its loopholes.[11] The regulation allowed insurers, through their scientific technical committees, to approve and provide required medicines that fell outside the benefits plan, but they were not allowed to do the same with other medical services. According to the regulation, surgeries, laboratory tests, and other medical services could not be approved, despite the clear constitutional obligation. In other words, the system promoted litigation as a way to access required services. In fact, the tutela was seen in those days as a “prerequisite” to accessing the health system. For the “good” insurers, this situation was evidence of the system’s dysfunction. For the “bad” ones, it was a business opportunity. All this was clearly reported by the national ombudsman, who showed that, in most cases, the denied health services were included in the benefits plan (56.4% in general; 89% in the case of surgeries).[12] In other words, health tutela claims—a way to access not-included services—had become a way to access even the included ones.
By the turn of the century, after substantial jurisprudence from the Constitutional Court regarding the right to health, both as connected to the right to life and subsequently as an autonomously enforceable right, the court was receiving an increasing number of health-related tutelas. In fact, the right to health went from being an exceptional case of justiciability in 1992 to being the most claimed right by tutela.[13] Different analyses identified various causes, including regulatory problems (vacuums, contradictions, and perverse incentives); poor supervision; and a lack of control and the absence of political will to structurally address the situation. For example, the benefits plan became obsolete (it had not been reviewed since its inception) and had a lot of gray areas (namely, doubts about which benefits should be included). It was becoming clear that the routine use of individual claims via tutela were leading to structural problems (including an obsolete vade mecum, regulatory gaps, inefficient and inadequate management of resources, and a lack of vigilance). The Constitutional Court understood the magnitude of this problem, which required structural solutions rather than specific orders for individual claims.
Thus, judicial rulings on the right to health began to seek structural solutions in addition to individual protections for the specific cases at hand, which would correct violations and, as a result, extend the right to health to more people. One such opinion was T-344 of 2002, which created a rule for resolving conflicts between treating physicians and health insurers with regard to health services being requested.[14] It was a judicial position that referred to constitutional rights in general, regardless of whether they are social, economic, or cultural, or whether they are procedural or freedom rights. In addition, the court’s jurisprudence established that every fundamental right, despite its nature, has facets that imply the decisive action of the state through the use of critical public resources. This position of the court was set in a case on the protection of a disabled person seeking mobility access to public spaces. This ruling, T-595 of 2002, established that when the protection and effective guarantee of a fundamental right depends on public policies, the minimum constitutional conditions of such a policy can be judicially claimed.[15] Eventually, Colombian constitutional case law evolved to protect the right to health in many instances, finally recognizing health as a fundamental right justiciable by itself.[16]
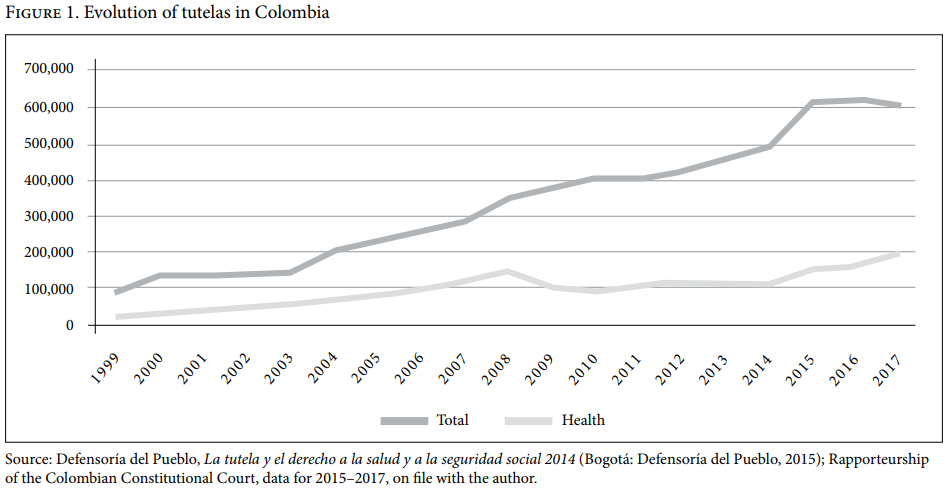
Subsequent legislative advances paved the way for the court’s structural judicial decisions. At the beginning of the 21st century, national, regional, and international debates were taking place on social rights.[17] Colombia’s Congress remained silent for many years, but its implicit support for the Constitutional Court was evident through its rejection of bills that tried to overrule constitutional jurisprudence or that tried to limit the tutela. In 2005, however, Congress began to engage and passed a law to improve the care of people suffering from “ruinous or catastrophic” diseases, especially HIV/AIDS (Law 972 of 2005). Two years later, it passed a law amending the health system’s regulatory framework, which had been established in 1993, and expressly supporting the jurisprudence of the Constitutional Court and the use of the tutela to enforce the right to health (Law 1122 of 2007). However, despite the harmonious view shared by the judiciary and Congress, the right to health continued to be violated in a number of scenarios. By 2008, evidence of problems in the health care system was overwhelming. Indeed, by that point, the Ombudsman’s Office had, for three years running, been asking the Constitutional Court to declare the health system to be in an “unconstitutional state of affairs.” Those years (2005–2008) were a turning point, representing the period when the largest number of tutelas were filed and when the proportion of health claims as a percentage of all tutelas reached its peak. In addition to complaints and ambiguities, the benefits plan remained unequal and had not been updated for ten years.
Decision T-760 of 2008
The Constitutional Court addressed these issues in Decision T-760 of 2008. This ruling resolved 22 different claims that captured some of the most critical problems of the health system. With this decision, the court reiterated its previous opinions and issued a set of structural orders to fix the basic problems of the health system, in addition to taking measures to protect the right to health in the specific cases analyzed. Most of the orders were general ones that were created not by the court but by experts and public agencies that participated in the judicial process.
In T-760, which was considered by some authors a landmark judgment, the court concluded that the existence of flaws in the regulation of the health system represented a violation of the state’s constitutional obligations to respect, protect, and guarantee the right to health.[18]
First, the court identified various general problems in the contributory regime. To begin with, there was a high level of uncertainty regarding the health services that were included in and excluded from the current benefits plan. The plan had become obsolete. Furthermore, the majority of judicial decisions protecting access to health services for citizens were aimed at guaranteeing access to services expressly included. Lastly, there was no administrative procedure that allowed patients to access health services (as opposed to medications) not included in the plan, such as surgeries and other medical interventions, to effectively enjoy their right to health.
Second, the court recognized a structure tending toward inequity within the health system. It considered it unacceptable that the government had not designed a program to effectively overcome inequalities between the subsidized and contributory regimes, as part of its constitutional duty to move progressively toward the expansion of insured services (the fundamental right to health is guaranteed to everyone on an equal basis).
Third, the court considered the sustainability of the health system. Among the 22 cases, the court selected two tutelas filed by health care providers against the Ministry of Health and regulatory agencies alleging inadequate and delayed flows of financial resources into the system. These two cases were unusual. Normally, tutelas are used by patients who sue health care providers or insurers, but in these cases, the insurers sued the regulators, using the power of the tutela as a guarantor of the right to health of their clients. The problem identified by the court was the excessive red tape required in order for health care providers to receive reimbursements.
Fourth, the court identified a lack of available information when it came to citizens’ choice of health care providers. The need to remedy information asymmetry in the health care market was obvious. Patients needed adequate information to choose a provider that would be best for them. In this regard, the court ordered health care providers to make relevant information available to users before they joined the providers’ schemes.
Finally, the court made a structural ruling to assure that the objective of universalizing the coverage of Colombia’s health system was achieved. It ordered the Ministry of Social Protection to adopt the necessary measures to achieve the goal of sustainable universal health coverage by 2010.
Although some of the orders were specific, most called for changes at the structural and policy levels. The court further emphasized that all the measures should be undertaken in a transparent and participatory manner and should be based on best evidence. In fact, T-760 recognized the duty of judges to support and respect the decision of when to limit the scope of the right to health, provided that such a decision was made on reasonable, public, transparent, and scientific grounds, including the possibility of an appeal based on better arguments.
But in those cases in which it is legitimate to impose limits and deny requested services, does it mean that the person denied treatment should feel that the system has turned its back on him or her? The court emphasized the need for procedures and processes that treated people with dignity, even when denying them care. This means that the system must acknowledge the seriousness of the situation faced by a particular patient and must assume a duty to inform, guide, and accompany that person through his or her health journey, in addition to providing services and compensatory guarantees. In other words, in a social sate under the rule of law, it is possible to say “no”—but it should be a compassionate “no,” not one that eviscerates the dignity of the other.
In response to T-760, the executive branch tried to reduce the scope of protection of the right to health recognized by the court. For example, it declared a state of emergency and enacted a set of executive decrees to “fix” the health system in its own restricted way, leaving aside the rights-based approach of constitutional jurisprudence and the political debate in Congress. These decrees were met with vigorous protest by unions, churches, health professionals, and others. The Constitutional Court later declared the decrees unconstitutional, forcing the administration to go to Congress to find democratic solutions to the structural problems of the country’s health system.[19]
Progress and setbacks
The impact of constitutional jurisprudence on the protection of the right to health in Colombia is becoming evident. Thousands of people now live with dignity because a tutela has granted them access to a medication or medical service; indeed, many of these people would have died without such a judicial intervention.[20] Without individual rulings, it would not have been possible to achieve the current levels of protection and fulfillment of the right to health. But there were also a lot of critics of these case-by-case interventions in health policy, arguing that they lacked a broader perspective.[21] Thus, the structural remedies turn of the Colombian constitutional jurisprudence has embraced a new way to deal with the progressive realization of a fundamental right. T-760 enabled an analysis of health system controversies as part of a broader political system. It moved beyond the facts of individual cases to promote solutions that would overcome larger issues, such as the opportunity costs that regulatory policies allowed for several years without effective controls (for example, not providing timely health services to people with high-cost diseases, such as HIV/AIDS, to prevent them from getting worse). The court sought to go beyond protecting access to necessary medicines (which had made up the majority of tutela rulings at that time) to ensure the effective enjoyment of a higher standard of health for all Colombians.
Nonetheless, the situation remains far from perfect. The health system still has many problems. In a ranking based on an index of health outcomes conducted by the Colombian Association of Clinics and Hospitals, Colombia ranked 48th out of 99 countries, with a score of 80.6 out of 100.[22] Political debate on the right to health continues. There are even radical critical voices that have been arguing for a long time that the actual problem of Colombia’s health care system is the liberal market-based model.[23]
But despite these problems and debates, Colombia faces a new legal scenario: the 2015 statutory health law—which defines the constitutional right to health as fundamental, autonomous, irrevocable, individual, and collective—has become the new common ground to settle disputes.[24] Health insurers and providers, as well as the three branches of power, have accepted these new rules. Decision T-760 of 2008 and the Statutory Health Act (Law 1751 of 2015 have become what Bruce Ackerman would call, respectively, a judicial “super-precedent” and a landmark statute that alter constitutional law without formally touching it.[25] This is an example of a “living constitution.”
There are two main observations to make. First, the health orders given by the Constitutional Court have favorably affected public policy. Second, the court’s T-760 ruling, on its own, could not have achieved these results—government and civil society support were also necessary.
Specifically, T-760 had at least three positive impacts: it helped establish the constitutional roots of the right to health and its justiciability (a living reform of the Constitution); it guaranteed better access to necessary health services; and it ensured that public health policies are rights oriented, including through the promotion of reasonable limits and public participation in decision making.
The following discussion explores some of the progress achieved in the health system in the wake of T-760.
Access to services
Various government actions have been taken to remove barriers to access to health services. To improve access to medicines, one of the principal actions was a change in the pricing policy implemented from 2003 until 2013.[26] Changes in policy began to be discussed after the sentence, but it took a few years to implement them. Before 2013, medicines were priced using value-based pricing. This resulted in numerous high-cost medicines being paid for by the national budget. By 2013, two new types of regulations were adopted to price medicines. The first is a “supervised market freedom” regime, which covers all medicines that are marketed in Colombia and included in a registry. The second regulation is a “direct control regime,” by which the National Commission for the Pricing of Medicines and Medical Devices establishes a maximum sales price for essential medicines, using the international reference pricing method.[27] According to the Ministry of Health, international reference pricing resulted in savings of approximately US$1.5 billion between January 2014 and September 2017.[28] Controlling the high costs of medicines (some of the highest prices in Latin America) removes one of the greatest barriers to access. The policy changes and their impacts have been debated in both academic journals and national newspapers.[29] Oscar Andia, a member of the Colombian Medical Federation and director of the Colombian Observatory of Medicines, has described the deregulation policies of 10 years ago as “good for business but not for patients,” and has argued that the current pricing policy improves the sustainability of the system and removes barriers to access.[30] Another newspaper editorial strongly supported the government policy, describing it as necessary and reasonable.[31]
The number of tutelas addressing access to health care decreased after decision T-760 of 2008. Although health claims continue to represent a significant proportion of all tutela claims, they decreased from 37.56% of all claims in 2006 to 23.74% in 2014. There is evidence of new growth (26.57% in 2016 and 32.54% in 2017), prompting the court to declare that the administrative measures taken to avoid the use of tutela are not enough.[32] But there are signs that it is a “new wave” of health litigation related to new issues; the nature of the claims has changed.[33] Except for the case of specific health insurers with significant problems (such as Medimás), fewer claims regarding entitlement to services are being raised, and more are being made to overcome other barriers, such as transportation challenges, long waiting times to see specialists, and access to complementary services such as home care.[34] There is also evidence of significant differences in health protection levels among regions.[35] But there are still a large number of individual claims that have not been studied. As the Ministry of Health informed the court, the tutela is not used in 97% of the services provided by the system.[36]
Rights-oriented policies
Throughout the 1990s and early 2000s, the right to health was not “equal” to other rights. Other considerations were prioritized (such as investor confidence), even in cases where there were severe impacts on people’s health. Some government decisions during those years (such as the pricing policy) that were unreasonable even from an economic perspective posed significant barriers to access, especially for patients of the subsidized regime who suffered from costly illnesses, such as cancer. This scenario can be attributed to a power imbalance between patients and providers, with patients on the losing end. In the public debate, cost overruns due to inefficiency, corruption, and loopholes allowing providers to benefit financially from the health system were overshadowed by the costs of health services needed by patients as ordered by tutelas, despite the fact that the former were clearly higher.[37]
The result is that there was greater concern over the negative effects of jurisprudence on health than over fixing the structural problems of the system, which, among other perverse effects, were propelling the health litigation.
State bodies appear to be addressing the significant problems of corruption and inefficiency in the health sector rather than trying to limit individual protection of the right to health by, for instance, pushing legislative amendments to stop this kind of claim. Currently, there is a bill from the Office of the Comptroller General and the Office of the Inspector General seeking to criminalize behavior that stands in the way of access to health care. In addition to saving lives, as some scholars have observed, this is also a victory for defending the critical role of the Constitution in shaping policies.[38] It has become clear that public policy is integral to the protection of fundamental rights (including the right to health). Further, the Constitution must be the basis of public policy in order to ensure that it is designed to be reasonable and accountable.
In addition to the battle for price controls on medicines, President Santos’s minister of health, for example, entered into important debates around the control of sugary drinks, which are considered a major contributor to obesity and weight-related diseases. Although Congress has not yet allowed a sugar tax, this battle is clear evidence of new winds.[39] The government is keeping the right to health central in new policies, even when it runs against the interests of powerful industries. Policies that began by addressing the right to access necessary health services have now moved toward ensuring better health through disease prevention and reducing the probability of needing health care. The difficulties that have been encountered in the attempt to tax sugary drinks have demonstrated that “taking rights seriously” is not easy. The health minister, in keeping with Lawrence Lessig, argues that a healthy democracy is necessary before a fundamental problem of society, such as a weak health system, can be fixed.[40] Finally, good financial management is crucial because the financial sustainability of the health system remains at risk.
Reasonable and deliberated limits
Colombian constitutional jurisprudence has always acknowledged the existence of reasonable limits to the right to health, which must be established through a participatory, transparent, and scientific process. This process is now happening (Resolutions 5267 of 2017 and 687 of 2018). Within the legal framework, the Ministry of Health is undertaking a public and open process to decide what services to exclude from the benefits plan. Determining limits in this way enables the health system to say “no” to requests for including certain health care services, but in a fair manner that respects human dignity. The Constitutional Court has tried to improve the deliberative process.[41] The process of enforcing complex and structural orders, by itself, could deepen democracy. Despite the challenges in enforcing the structural orders of T-760, the court has opened spaces for deliberation and public reflection. It has allowed, for example, the public scrutiny of cost overruns in the design of the current system and close inspection of the scarcity of resources as a justification for restrictions.[42]
Evidence of progress recognized
The social rights advances made in Colombia have been recognized by scholars and institutions beyond the field of health. For example, the Organisation for Economic Co-operation and Development acknowledges the challenges that the system still faces (improving quality, efficiency, and sustainability) but also recognizes the achievements.[43]
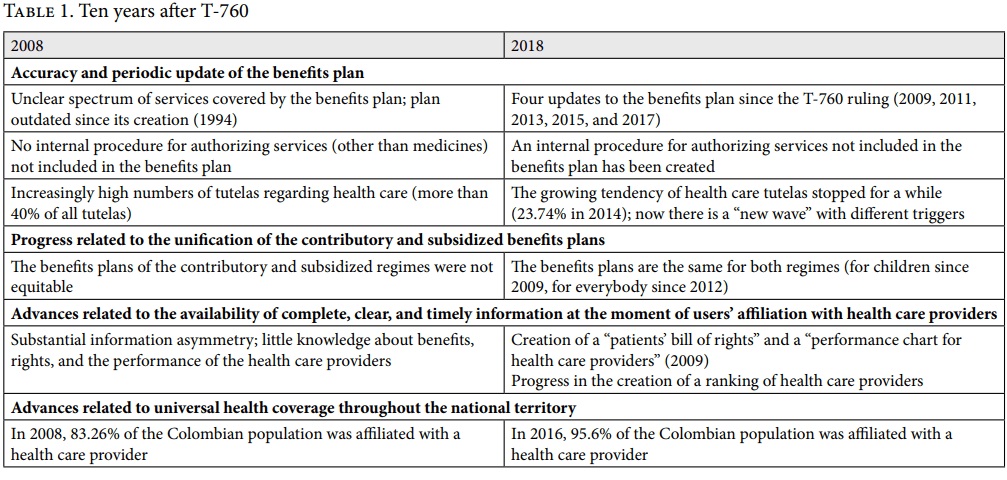
Since 2008, there have been important advances in the accuracy and periodic updating of the benefits plan. A participatory process to update the plan was undertaken every two years from 2009 to 2017.[44] Another concern was the lack of internal procedures allowing health care providers to directly authorize the provision of services (as distinct from medicines) not included in the benefits plan. As an initial measure, the Ministry of Health and Social Protection issued Resolution 3099 of August 19, 2008, expanding the competencies of health care providers’ technical scientific committees to authorize medical services not included in the benefits plan. Later, the 2015 statutory health law removed additional restrictions.
Furthermore, inequities between the contributory and subsidized regimes were removed in 2009, when the same benefits were guaranteed to children regardless of which regime they belonged to.[45] Then, in 2012, the benefits plans were unified through a decision (Agreement 032) of the Regulatory Body in Health. The court has declared a high level of compliance with the judicial order to unify the benefits plan of both regimes.[46] Advances have also been made regarding the availability of complete, clear, and timely information for users at the moment of selecting a health care provider. In 2009, the Ministry of Health and Social Protection issued Resolution 1817 to establish guidelines and operational processes for health care providers. This resolution outlines a patients’ bill of rights and a performance chart for health care providers. The Constitutional Court has also proposed that health care providers be ranked according to their level of performance to help people decide which provider to use.[47] But there is still a lot to do in this area; the court has declared a medium level of compliance with this order.[48]
Finally, advances have been made with regard to universal coverage. According to the Ministry of Health and Social Protection, in 2008, 83.26% of the population was affiliated with a health care provider. By 2016, this had reached 95.6%. This progress has also reduced inequities resulting from wealth inequalities. Ministry of Health data reveal that in 2016, 92.6% of the population with a lower income and 91.1% of the population with the highest income were affiliated with the health system. This has occurred at the same time as the unification of benefit plans. Universal protection is being achieved under conditions of equality. Before T-760, the government intended to achieve universal health coverage but postpone the unification of the plans. However, the court prevented this, ordering it to do both at the same time. Currently, the inequity in accessing the system relates less to a person’s financial position and more to barriers such as geographical accessibility and the lack of available services in conflict-affected areas.
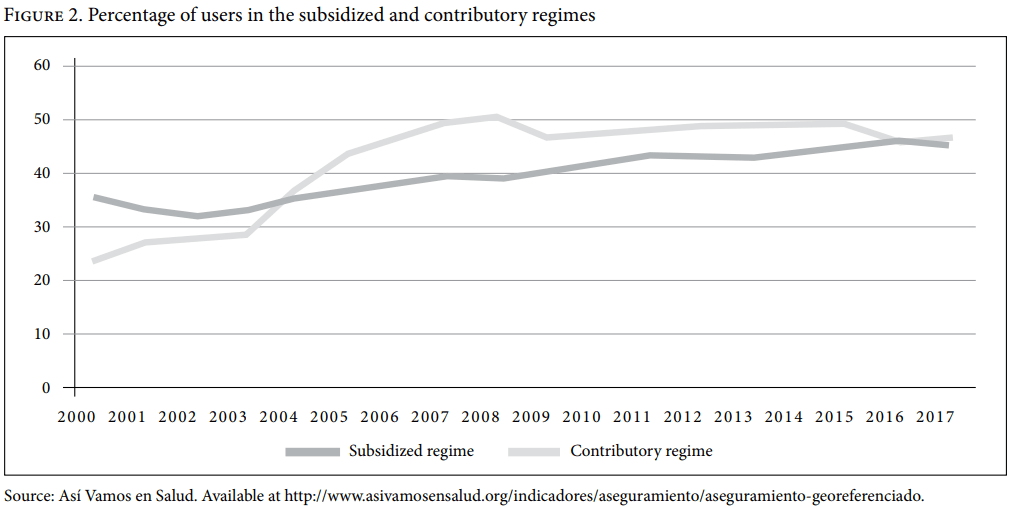
Some critics have suggested that the Constitutional Court’s order to offer the same benefit plan to those who contribute and those who do not contribute would encourage people not to contribute. But the court advised the government to take additional measures to avoid this perverse effect.[49] In practice, granting the same benefit plan to all people has not led to a decrease in affiliations to the contributory regime (see Figure 2).
As mentioned above, the situation is far from perfect. Some general indicators are mediocre, rather than good.[50] But if we compare today’s situation with that of 2008, the advances in health policies are evident.
Conclusion
The Colombian experience shows how the power of the people to litigate can help secure the protection of their right to health. Judicial intervention can bring justice and equity to a health system when judges listen to both sides of the debate on aspects of the fundamental right to health. On the one hand, this right must be respected as a prerequisite for democracy. Judges must ensure that authorities recognize and enforce its effective enjoyment. On the other hand, the fulfillment of this right should be based on technically supported rational arguments, as well as on ethical grounds, principles, and values. This requires transparent decision-making processes open to public scrutiny and democratic participation. In these situations, judicial intervention does not become the “rule of the judges” but is instead a legitimate way to exert pressure on the government to act according to the rule of law, and within constitutional boundaries.
It is essential that public policies aimed at protecting a fundamental right ensure a reasonable policy design, implementation, and evaluation. Colombia’s courts and judges will still face many challenges in dealing with structural and complex orders. But today, through the tutela, there is finally democratic access to constitutionally controlled public policies.[51] It is settled that the right to health is a fundamental constitutional and justiciable right.
Constitutional litigation is one of several democratic tools. Structural and complex remedies to guarantee the effective enjoyment of a fundamental right function when supported by, and carried out in collaboration with, other branches of power. Courts by themselves cannot assure, for example, total coherence between national agencies and local governments. The success of a structural remedy can be seen when the court is no longer needed.[52] When the policymaking process respects constitutional boundaries, judges should take a step aside—not when everything is perfect, but when policy makers take rights seriously and fully respect them.[53]
Acknowledgments
I am grateful to Martha Agudelo Córdoba for her collaboration as an assistant researcher and to Alicia Ely Yamin for her comments and support.
Aquiles Ignacio Arrieta-Gómez is a Colombian lawyer, philosopher, and professor who, since 1996, has assisted several justices in the Constitutional Court; he was a temporary justice at the court from September 2016 to May 2017.
Please address correspondence to Aquiles Arrieta-Gómez. Email: aquilesarrieta@gmail.com.
Competing interests: The author was part of the technical teams that supported justices of the Colombian Constitutional Court in authoring judicial opinions on the right to health, among them Decision T-760 of 2008.
Copyright © 2018 Arrieta-Gómez. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
[1]. Ley Estatutaria 1751 de 2015, Por medio de la cual se regula el derecho fundamental a la salud y se dictan otras disposiciones.
[2]. See, for example, E. Rodríguez Piñeres, “Relaciones entre los poderes judicial y legislativo,” in Por el reinado del derecho (Colombia: Imprenta de La Luz, 1927); M. J. Cepeda Espinosa, “La defensa judicial de la Constitución,” in F. Cepeda Ulloa (ed), Fortalezas de Colombia (Colombia: Ariel & BID, 2004); M. J. Cepeda Espinosa, “Judicial activism in a violent context: The origin, role, and impact of the Colombian Constitutional Court,” Washington University Global Studies Law Review 3/4 (2004); M. J. Cepeda Espinosa and D. Landau, Colombian constitutional law: Leading cases (New York: Oxford University Press).
[3]. See, for example, C. Rodríguez Garavito and D. Rodríguez Franco, Cortes y cambio social: Cómo la Corte Constitucional transformó el desplazamiento forzado en Colombia (Bogotá: Dejusticia, 2010); M. Langford, C. Rodríguez Garavito, and J. Rossi, Social rights judgments and the politics of compliance: Making it stick (Cambridge, MA: Cambridge University Press, 2017).
[4]. See, for example, Rodríguez Garavito and Rodríguez Franco (see note 3); Langford et al. (see note 3).
[5]. M. Tushnet, Weak courts, strong rights: Judicial review and social welfare rights in comparative constitutional law (Princeton, NJ: Princeton University Press, 2008); Langford et al. (see note 3).
[6]. See the Constitution of Colombia, art. 40; A. I. Vellvé Torras, J. J. Ruchti, and M. del C. Gress, Political Constitution of Colombia of 1991, as consolidated to Legislative Act No. 5 (July 18, 2011) (HeinOnline World Constitutions Illustrated Library, 2011).
[7]. See, for example, Decision T-261 of 1999;, Decision T-549 of 1999; Decision T-524 of 2001; Decision T-053 of 2002.
[8]. Ministry of Health, Resolución 3384 of 2000 (December 29), art. 4.
[9]. Cepeda Espinosa and Landau (see note 2); Decision T-972 of 2001.
[10]. A. Arrieta Gómez, “Comentarios a la creación de jurisprudencia constitucional, el caso del acceso a los servicios de salud,” Revista Tutela 45 (2003); O. Parra Vera, El derecho a la salud en la Constitución, la jurisprudencia y los instrumentos internacionales (Bogotá: Defensoría del Pueblo, 2003).
[11]. See, for example, Defensoría del Pueblo, La tutela y el derecho a la salud: Causas de la tutela en salud (Bogotá: National Printing, 2004); Defensoría del Pueblo, La tutela y el derecho a la salud, período 2003-2005 (Bogotá: National Printing, 2007); Defensoría del Pueblo, Evaluación de los servicios de salud que brindan las Empresas Promotoras de Salud (Bogotá: National Printing, 2005); see also M. E. Echeverri López, “La situación de salud en Colombia,” in S. Franco Agudelo (ed), La salud pública hoy (Bogotá: Universidad Nacional de Colombia, 2002); M. Vélez, Salud: Negocio e inequidad; Quince años de la Ley 100 en Colombia (Bogotá: Ediciones Aurora, 2008); M. Vélez, La salud en Colombia, pasado, presente y futuro de un sistema en crisis (Bogotá: Debate, 2016).
[12]. Defensoría del Pueblo (2007, see note 11).
[13]. Regarding the process of those years, besides the reports of the Defensoría del Pueblo, see E. Lamprea Montealegre, La Constitución de 1991 y la crisis de la salud (Bogotá: Universidad de Los Andes, 2011); C.Rodríguez Garavito, “La judicialización de la salud: síntomas, diagnóstico y prescripciones”, in Bernal and Gutiérrez (ed) La Salud en Colombia: logros retos y recomendaciones (Colombia: Universidad de Los Andes, 2012); E. Lamprea Montealegre, Derechos en la práctica:. Jueces, litigantes y operadores de políticas de salud en Colombia (1991-2014) (Bogotá: University of Los Andes, 2015).
[14]. Decision T-344 of 2002.
[15]. Decision T-595 of 2002.
[16]. See, for example, Decision T-227 of 2003.
[17]. R. Arango Rivadeneira, “Basic social rights, constitutional justice, and democracy,” Ratio Uris 16/2 (2003), pp. 141–154); V. Abramovich and C. Courtis, Los derechos sociales como derechos exigibles (Madrid: Trotta, 2002).
[18]. See, for example, G. Backman, P. Hunt, et al., “Health systems and the right to health: An assessment of 194 countries,” Lancet 372 (2008), pp. 2047–2085.
[19]. Decision C-252 of 2010.
[20]. E. Lamprea Montealegre (2015, see note 13).
[21]. See, for example, A. Yamin, O. Parra, and C. Gianella, “Colombia: Judicial protection of the right to health; An elusive promise?,” in A. Yamin, S. Gloppen (eds), Litigating health rights: Can courts bring more justice to health? (Cambridge, MA: Harvard University Press, 2011).
[22]. J. C. Giraldo Valencia, “Rasgos distintivos de los sistemas de salud: Actualización 2017,” Hospitalaria 19/114 (2017).
[23]. See, for example, M. Hernández Alvarez, “El derecho a la salud en Colombia: Obstáculos estructurales para su realización,” in V. de Currea Lugo, M. Hernández, and N. Paredes (eds), La salud está grave (Bogotá: Plataforma Colombiana de Derechos Humanos, Democracia y Desarrollo, 2000); see also M. Hernández Alvarez, La salud fragmentada en Colombia, 1910–1946 (Bogotá: Universidad Nacional de Colombia, 2002); M. Hernández Alvarez, La fragmentación de la salud en Colombia y Argentina: Una comparación sociopolítica, 1880–1950 (Bogotá: Universidad Nacional de Colombia, 2004).
[24]. Law 1751 of 2015, Art. 2.
[25]. B. Ackerman, “The living constitution,” Harvard Law Review 120/7 (2007), pp. 1737–1812.
[26]. See, for example, Ministry of Health, Decreto 1782 of 2014; Ministry of Health, Circular 03 of 2017.
[27]. Ministry of Health, Circular 03 of 2013; see also Ministry of Health, Circular 01 of 2014.
[28]. Ministry of Health data, Análisis de mercado. Available at https://www.minsalud.gov.co/sites/rid/Lists/BibliotecaDigital/RIDE/VS/MET/Analisis-mercado-medicamento-control-directo-ahorros-sgsss.zip.
[29]. See, for example, T. Andia Rey, “Entre la legitimidad y el control: El arreglo institucional de los medicamentos en el sistema de salud colombiano,” in O. Bernal and C. Gutiérrez (eds), La salud en Colombia: Logros, retos y recomendaciones (Bogotá: University of Los Andes, 2012); F. A. Rossi Buenaventura, “El mercado de los medicamentos en Colombia: Entre la salud y los negocios,” in S. Franco Agudelo (ed), La salud pública hoy (Bogotá: Universidad Nacional de Colombia, 2002).
[30]. O. Andia, “Control de precios a medicamentos,” El Tiempo (January 7, 2018).
[31]. Editorial, El Espectador (January 4, 2018).
[32]. Auto 590 of 2016.
[33]. Defensoría del Pueblo, La tutela y el derecho a la salud 2012 (Bogotá: National Printing, 2013); see also Defensoría del Pueblo, La tutela y el derecho a la salud y a la seguridad social 2014 (Bogotá: National Printing, 2015).
[34]. Defensoría del Pueblo (2013, see note 33).
[35]. Así vamos en salud, Indicadores. Available at https://www.asivamosensalud.org/indicadores/consolidado-nacional.
[36]. Auto 590 of 2016. The court asked the Ministry of Health to clarify how it has obtained these figures.
[37]. Defensoría del Pueblo (2013, see note 33).
[38]. Lamprea Montealegre (2015, see note 13).
[39]. C. Orozco Tascón, “Esta semana hubo muchos lobistas en el Congreso,” El Espectador (November 27, 2016).
[40]. A. Gaviria Uribe, “Yo estuve en el debate sobre las bebidas azucaradas,” El Espectador (January 1, 2017).
[41]. R. Gargarella, “Dialogic justice in the enforcement of social rights: Some initial arguments,” in A. Yamin, S. Gloppen (eds), Litigating health rights: Can courts bring more justice to health? (Cambridge, MA: Harvard University Press, 2011).
[42]. See, for example, O. Parra-Vera and A. Yamin, “La implementación de la Sentencia T 760/08 en Colombia,” in L. Clérico, L. Ronconi, and M. Aldao (eds), Tratado de derecho a la salud (Buenos Aires: Abeledo Perrot, 2013); C. Gianella-Malca, O. Parra-Vera, A. Yamin, and M. Torres-Tovar, “¿Deliberación democrática o mercadeo social? Los dilemas de la definición pública en salud en el contexto del seguimiento de la sentencia T–760 de 2008,” Health and Human Rights Journal 11/1 (2009), Perspectives.
[43]. Organisation for Economic Co-operation and Development, Colombia still faces challenges to improve health care quality. Available at http://www.oecd.org/health/colombia-still-faces-challenges-to-improve-health-care-quality.htm.
[44]. See Auto 410 of 2016.
[45]. Auto 342 of 2009.
[46]. Auto 410 of 2016.
[47]. Auto 153 of 2014; Auto 230 of 2016.
[48]. Auto 591 of 2016.
[49]. Auto 411 of 2016.
[50]. Así vamos en salud. Available at http://www.asivamosensalud.org/indice-asi-vamos-en-salud.
[51]. See, for example, E. Lamprea Montealegre (2015, see note 13); Langford et al. (see note 3).
[52]. See, for example, Rodríguez Garavito and Rodríguez Franco (see note 3).
[53]. See, for example, Decision T-388 of 2013.
