Benjamin Mason Meier and Averi Chakrabarti
Health and Human Rights 18/1
Published June 2016
Abstract
The Kingdom of Bhutan is seeking to progressively realize the human right to health without addressing the cross-cutting human rights principles essential to a rights-based approach to health. Through a landscape analysis of the Bhutanese health system, documentary review of Bhutanese reporting to the UN human rights system, and semi-structured interviews with health policymakers in the Kingdom of Bhutan, this study examines the normative foundations of Bhutan’s focus on “a more meaningful purpose for development than just mere material satisfaction.” Under this development paradigm of Gross National Happiness, the Bhutanese health system meets select normative foundations of the right to health, seeking to guarantee the availability, accessibility, acceptability, and quality of health care and underlying determinants of health. However, where Bhutan continues to restrict the rights of minority populations—failing to address the ways in which human rights are indivisible, interdependent, and interrelated—additional reforms will be necessary to realize the right to health. Given the continuing prevalence of minority rights violations in the region, this study raises research questions for comparative studies in other rights-denying national contexts and advocacy approaches to advance principles of non-discrimination, participation, and accountability through health policy
Introduction
The Kingdom of Bhutan straddles two worlds: reforming health policy to ensure domestic happiness while denying human rights to minority populations. Although the Bhutanese government has reformed its national health system in accordance with select norms of the human right to health, the continuing denial of universal equality stands as an impediment to a rights-based health system, with this failure to ensure cross-cutting principles of non-discrimination, participation, and accountability undercutting government efforts to realize the right to health. Advancing understanding of cultural relativism debates at the intersection of health and human rights, it is necessary to account for those states that seek to meet public health goals while denying the larger interrelated set of health-related human rights. Given international efforts to address health rights in rights-denying states, it is vital that human rights advocates recognize culturally specific limitations to realizing the right to health through national health policy.
All policies in the Kingdom of Bhutan seek to enhance Gross National Happiness (GNH). Based upon principles of Mahayana Buddhism, GNH focuses on the advancement of social harmony, preservation of national identity, and sustainability of natural environments. By emphasizing non-economic measures in development policy, looking beyond Gross Domestic Product, the Bhutanese GNH system surveys citizens to assess their holistic well-being. With Bhutanese citizens consistently found to be among the happiest in the world, the Bhutanese government has sought to enlarge the global development agenda to incorporate notions of happiness. Yet, while Bhutan has sought to export its GNH Index to other nations, advancing GNH to widespread acclaim in the United Nations (UN), it is only beginning to interact with the UN human rights system and to confront criticism of its minority rights practices.
Where few have studied the ways in which Bhutanese GNH policy comports with international human rights law, this article investigates the policies through which human rights norms and principles have been implemented in the transformation of Bhutan’s national health system. The opening section reviews the political history of the Kingdom of Bhutan, introducing the governance reforms that have accompanied its recent democratic transition and the policy goals of Bhutan’s GNH approach to development. Central to GNH, the next section outlines the rapidly changing Bhutanese health system and analyzes the ways in which this evolving system seeks to progressively realize several normative foundations of the human right to health. However, highlighting the government’s continuing neglect of principles of non-discrimination, participation, and accountability in the health system, the article then examines the contradictions through which the Kingdom of Bhutan relies on a narrow vision of the right to health without engaging human rights principles that might challenge state authority, focusing on select norms of the right to health to the exclusion of minority rights. The article concludes that rights-based health advocacy in rights-denying states will require that public health advocates understand this tension in realization of the right to health, recommending additional cross-national research to understand how national policymakers engage the right to health selectively while avoiding cross-cutting principles of human rights.
The Kingdom of Bhutan and the goal of Gross National Happiness
Nestled high in the Himalayas between India and China, the Kingdom of Bhutan’s roots can be traced to the 17th century, when Shabdrung Ngawang Namgyal, a Buddhist military leader from Tibet, secured control over most of the Druk Yul (Land of the Thunder Dragon) and developed Bhutan’s dual religious/secular system of government. 1 With Buddhism having long predominated in the region, introduced in the 8th century by the Indian monk Padmasambhava (Guru Rimpoche in Bhutan), Buddhist monks continued to hold theocratic authority over the new Bhutanese state.2 Through the formalization of secular government, Penlops (regional fiefs) existed until 1907, when one Penlop was selected to be king over the entire state, marking the beginning of Bhutan’s hereditary monarchical system of governance, now extended across five generations of kings.3 Despite the formal establishment of democratic rule through the 2008 Constitution, Buddhism remains the “spiritual heritage” of this new constitutional monarchy, with the Druk Gyalpo (Dragon King) and Je Khenpo (leader of Central Monk Body) sharing authority over all matters of religion and state.4
In this small kingdom, there is substantial ethnic diversity: the Ngalong peoples (of Tibetan origin) are concentrated in the western and northern districts; Sharchops (originally from northern Burma and northeast India) are concentrated in eastern districts; and Lhotshampas (of Nepali origin) are concentrated in the southern foothills.5 The Ngalongs have long been politically dominant, reflected in the state’s:
-
religious makeup: Buddhists make up about 80% of the population, with the Ngalong practice of Tibetan-style Mahayana Buddhism permeating all aspects of Bhutanese life, even though Hindu and Christian populations make up the majority of the south.6
-
linguistic makeup: Dzongkha, the Ngalong language, is the official language of the country, although many other Tibeto-Burman languages predominate in the central and eastern parts of the country and Nepali is spoken in the south.7
This dominance of Ngalong/Buddhist/Dzongkha populations has often persisted to the detriment of ethnic, religious, and linguistic minorities.
Following a century of absolute monarchy in Bhutan, extended across five generations of kings, King Jigme Singye Wangchuk stepped down from the throne in 2006, declared the country to be a democracy, and handed over the reins of government to his son, Jigme Khesar Namgyel Wangchuk. The young Wangchuk, the fifth Dragon King, oversaw the nation’s first legislative elections in 2008, marking Bhutan’s transition to a constitutional monarchy.8 Where Bhutan has traditionally delegated authority to the local level, the country is now administratively divided into 20 dzongkhags (districts) and 205 gewogs (blocks), with district-level development committees administering local projects and articulating local needs.9 This decentralized governance structure has provided a basis to address Bhutan’s policy focus on GNH, presenting “a new paradigm based on human happiness and the wellbeing of all life forms as the ultimate goal, purpose and context of development.”10
GNH was envisioned in Bhutan as a method of encouraging holistic development, redefining development as the advancement of political, economic, social, and cultural goals. The enshrinement of happiness as a policy goal can be traced back to Bhutan’s 1729 legal code, which stated that “if the Government cannot create happiness (dekid) for its people, there is no purpose for the Government to exist.”11 With the third king declaring his principal intention to make the Bhutanese people “prosperous and happy,” he focused on happiness in commemorating Bhutan’s 1971 admission as a UN member state.12 Soon after his accession to the throne in 1972, the fourth king declared that he would reform Bhutanese policy “to achieve economic self-reliance, prosperity and happiness.”13 Coining the term ‘Gross National Happiness’ (and proclaiming it morally superior to Gross National Product), he formalized happiness as a national policy goal and a means to transform the Kingdom.
To reorient the nation toward GNH—making happiness the official goal of all policies—the Bhutanese government has sought to realize equitable and sustainable socio-economic development, environmental conservation, cultural preservation, and good governance.14 This national commitment to GNH has been woven throughout the 2008 Bhutanese Constitution, which codified that: “The State shall strive to promote conditions that will enable the pursuit of Gross National Happiness.”15 Surveying its citizens to assess happiness, the government of Bhutan now distributes GNH surveys to “representative samples” to assess nine domains: psychological well-being, health, education, culture, time use, good governance, community vitality, ecological diversity and resilience, and living standards.16 The GNH survey asks multidimensional questions on each of the domains, providing respondents an opportunity to rank their satisfaction on a scale from deeply unsatisfied to incredibly satisfied.17 Based upon these rankings, individuals can be classified as unhappy, narrowly happy, extensively happy, and deeply happy; by examining aggregate happiness levels in the national GNH Index, the government can reallocate resources to increase the proportion of happy people and decrease the “insufficiencies of the not-yet-happy people.”18
Seeking to export this paradigm of happiness through global development discourse, Bhutan has repeatedly extolled its GNH Index throughout the world, with the UN General Assembly supporting a 2011 resolution on “Happiness: Towards a Holistic Approach to Development.”19 These efforts to promote GNH have provided the Bhutanese government with an oversized voice in the UN agenda, allowing this small state to host a 2012 High-Level Meeting on “Happiness and Wellbeing: Defining a New Economic Paradigm.”20 The GNH model continues to resonate in UN development debates, with the Kingdom of Bhutan held up as a model for translating happiness into policy under the Sustainable Development Goals.21 As a reflection of Bhutan’s global efforts to advance happiness in development, the UN General Assembly has declared March 20th to be International Happiness Day.22
Health and human rights in the Kingdom of Bhutan
Described repeatedly as “the last Shangri-La,” a paradise on earth, the Bhutanese monarchy has endeavored to create a society according to Buddhist principles, seeking happiness through its national health system. The government has long seen the need for a national health system as a means to GNH, with the 2008 Constitution making explicit that the government “shall provide free access to basic public health services in both modern and traditional medicines” and, drawing on the Universal Declaration of Human Rights, shall “endeavor to provide security in the event of sickness and disability or lack of adequate means of livelihood for reasons beyond one’s control.”23 Although the Kingdom of Bhutan has not ratified many of the international treaties that codify a right to health, health is recognized as one of the nine domains of GNH, and the government has argued that it is implementing the right to health through GNH policy reforms.24
Yet even as the Kingdom of Bhutan seeks to secure happiness through health policy, it has done so at the expense of minority populations. Where many states have been seen to violate individual rights in the pursuit of economic development, the Kingdom of Bhutan has employed similarly violative means to achieve its unique focus on development through national happiness.25 This focus on GNH, however, creates distinct human rights challenges, with the government simultaneously
-
seeking to uphold the economic and social rights of the nation to facilitate the spiritual, emotional, and cultural well-being of society, while
-
continuing to restrict the rights of minority populations to maintain a uniform national identity for this pursuit of happiness.
The Bhutanese government thus presents a paradox in human rights realization, developing policies to fulfill the right to health through the health system’s GNH focus while undermining this rights-based effort through violations of cross-cutting human rights principles for non-discrimination and equality, participation, and accountability.
Bhutan’s rights-based health system
As Bhutan’s 2008 Constitution mandates universal access to health as part of the government’s commitment to GNH, the first National Health Policy, launched in 2011 by the Ministry of Health, authorized the government to: “Build a healthy and happy nation through a dynamic professional health system, attainment of highest standard of health by the people within the broader framework of overall national development in the spirit of social justice, and equity.”26 The Policy thereby frames the health system in accordance with select normative obligations of the human right to health, seeking to make health progressively available, accessible, acceptable, and of sufficient quality.27
Bhutan Ministry of Health and WHO Country Office in Bhutan photo: Benjamin Mason Meier
The Bhutanese health system
The Bhutanese Ministry of Health was established with the objective of bringing “GNH closer to a reality” through the realization of health.28 Pursuing a holistic health system, the Ministry has explicitly advocated this approach as a reflection of the WHO definition of health: “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”29 The health system seeks to realize this focus on “complete health” through both health care and determinants of health.
In meeting the Kingdom’s constitutional obligation to provide “free access to basic public health services in both modern and traditional medicines” to its largely rural population, Village Health Workers (VHWs), Basic Health Units (BHUs) and Outreach Clinics (ORCs) often provide the principal level of primary health care.30 Although the VHWs are not paid government employees, they serve as a valuable “complimentary [sic] force to support the activities of the health system.”31 The BHUs are the official source of primary health care, providing basic medical care, maternal and child care services, and prevention interventions.32 These BHUs run ORCs, through which health personnel travel to geographically isolated villages.33 Cases that cannot be resolved by these primary care facilities are referred to the formal hospital system, comprised of the district hospitals (located in each of the country’s 20 districts), the regional referral hospitals in Mongar (east Bhutan) and Gelephu (south Bhutan), and the Jigme Dorji Wangchuk National Referral Hospital in Thimphu.
Beyond health care, the new Bhutanese Constitution also seeks to “ensure a safe and healthy environment,” and the Ministry of Health has employed this authority to achieve significant public health advancements through disease prevention and health promotion programs.34 Public health interventions have led to the virtual disappearance of endemic goiter and leprosy, reduced the prevalence of vector-born diseases, achieved near-universal childhood immunization, and stemmed the flow of water-borne illness.35 To halt tobacco-related diseases, Bhutan became the first nation in the world to ban cigarette smoking and prohibit the production and sale of tobacco.36 Given this primary health care approach—providing community-based health care and addressing underlying determinants of health—WHO has repeatedly praised the Kingdom of Bhutan for the impact of its health system on the public’s health.37
The Ministry of Health plays a crucial leadership role in “nurturing” these health care and public health programs, working with foreign donors and international organization to support needed international assistance and cooperation in health initiatives.38 WHO has applauded the Bhutanese government for being “proactive in managing donor assistance within a well-defined framework, avoiding duplication and overlaps, with each donor or development partner active in preferred areas of assistance.”39
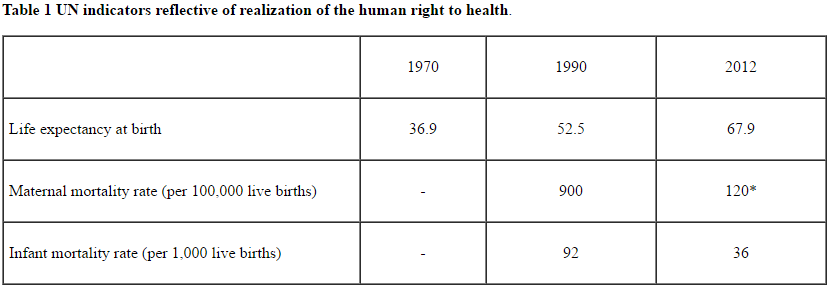
Based upon Bhutanese government programs and foreign health assistance, health indicators in Bhutan have improved steadily, as seen in Table One.
*Data pertains to 2013
The Kingdom of Bhutan fares better on many health indicators than its counterparts in the WHO South-East Asia Region, with considerably lower rates of maternal mortality (120 per 100,000 live births, compared to 190 for the region), HIV (142 per 100,000 people, compared to 185 for the region) and malaria (20 per 100,000 people, compared to 1,462 for the region).40 Even as the nation undergoes a larger “demographic transition”—with longstanding problems of undernutrition compounded by new problems of overconsumption—the government has begun to focus on non-communicable diseases, encouraging healthy diets and physical activity.41 With the first national GNH surveys finding the greatest expressions of citizen happiness in the health domain, these health system reforms speak to the government’s efforts to implement certain norms of the right to health.
Mainstreaming the right to health
The right to health, codified seminally in Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR) and clarified expansively in General Comment 14 of the UN Committee on Economic, Social and Cultural Rights (CESCR), is progressively realized through the Bhutanese health system’s structures, processes, and outcomes.42 Establishing the legal structure of its health system under the 2008 Constitution, the Kingdom of Bhutan has set out a range of laws to realize the right to health. Building from government processes to implement primary health care, Bhutan’s National Health Plan has laid out “detailed provisions clarifying what society can expect by way of health-related services and facilities.”43 Heralding its improving public health outcomes, Bhutan has made enormous strides in reducing the risk of prevalent diseases, with major implications for the country’s public health. In accordance with select normative foundations of the human right to health, these implementation efforts for health care, disease prevention, and health promotion highlight Bhutan’s rights-based practices to guarantee health availability, accessibility, acceptability, and quality (AAAQ):
-
Availability: The right to health looks to whether there is a sufficient quantity of health facilities, goods, and services, and Bhutan has made progressive efforts to enhance health availability by increasing the number of health care personnel, developing its health education system, and ensuring essential medicines.44 Where Bhutan has long faced a significant shortfall of health care workers, with approximately half the amount that WHO guidelines recommend, it has seen a dramatic scaling up in the past decade: from 50 doctors and 335 nurses in 2002 to 244 doctors and 957 nurses in 2014.45 Bhutan’s National Mental Health Program seeks to assure the availability of mental health care through the general health care system, with additional resources through 63 psychiatric facilities, one mental health inpatient ward, two psychiatrists, and three psychiatric nurses.46 To further increase the availability of health services, Bhutan is expanding its health education system, with the Royal Institute of Health Sciences (RIHS) developing its first bachelor’s degree program in Public Health in 2010 and in Nursing and Midwifery in 2012.47
Although Bhutanese students previously studied abroad to receive advanced medical training, the Bhutanese government has worked with India to establish a new medical school, the University of Medical Sciences of Bhutan, which is developing programs in medicine, traditional medicine, nursing, and public health.48 While Bhutan continues to have a lower proportion of health personnel than other countries in the region, it spends (with support from foreign donors) far more per capita than its regional counterparts on health goods and services, with WHO estimating that essential medicines are now available to more than 90% of the population.49
-
Accessibility: The Bhutanese health system seeks to expand accessibility to health through a continuum of free services, with the tiers of the Bhutanese health system—the VHWs, BHUs, and hospitals—meeting international human rights standards to “have a mix of primary (community-based), secondary (district-based), and tertiary (specialized) facilities and services.”50 Facilitating geographic accessibility in a country of scattered rural settlements and rugged mountainous roads, the primary health care system is “reasonably equitably distributed” and, in accordance with the National Health Policy, can be accessed by 90% of citizens within a three-hour walk (with the remaining 10% reached by ORCs).51 The VHW program exists principally to improve health education (information accessibility) in villages, with national trainings for VHWs to disseminate information on sanitation practices, family planning, and “the importance of cleanliness, immunization and a healthy diet.”52 To ensure the continuing affordability (economic accessibility) and “long-term sustenance” of these health services, the government in 1997 established the Bhutan Health Trust Fund—with centralized government purchasing and matching foreign contributions—to finance vaccines and essential medications.53 Although there remains a continuing shortage of specialists and supplies in the district hospitals, patients can be referred to distant facilities for tertiary care, with the Bhutanese government assuming all expenses for transporting patients and escorts, if necessary, outside of the country.54
-
Acceptability: Where the right to health seeks acceptability to cultural standards in public health systems, the Bhutanese health system has been designed in line with the Buddhist traditions practiced by the majority of citizens.55 Combining elements from traditional medicine and modern medicine in all hospitals, it is common for patients to be referred between traditional and modern medical units. The traditional medical care practitioners—both Drungtshos (traditional doctors) and sMenpas (traditional compounders)—have been formally integrated into the national health system and receive required training at the Institute of Traditional Medicine Services.56 In cases where modern medicine has challenged cultural beliefs—for example, cancer is “an almost taboo topic in the country” and often goes unreported because it is thought to be a consequence of improper actions in this or a previous life—modern medical practitioners have worked with traditional healers to raise awareness, increase diagnoses, and expand treatment options.57 Beyond cultural acceptability, the health system also considers acceptability to affected communities, as seen where the government’s HIV programs have sought to be “responsive to the needs of the vulnerable and marginalized groups, especially people living with HIV/AIDS, Men who have sex with Men, Commercial Sex Workers and Trans-genders.”58
-
Quality: A health system realizing the right to health must secure “a level of quality consistent with medical and scientific standards.”59 Although past international reviews have found that many of the health facilities in Bhutan are “of questionable quality,” lacking even necessary equipment, these external reviews have taken note of recent upgrades and concluded, based on Bhutan’s level of development, that the “[q]uality of care in general is reasonable.”60 Similarly, while the poor training of health workers is likely to affect the quality of health services, the training programs discussed above are likely to improve both the quantity and quality of trained workers in the years to come. In creating regulatory institutions for the maintenance of health system quality, the Bhutan Medical and Health Council Act of 2002 regulates medical and health personnel, and the Bhutan Medicines Act of 2003 oversees the quality of medications.61 To guide health personnel in assuring the quality of medications, Bhutan has codified a National Drug Policy to bring about more “rational prescribing” of modern medicines and created a Pharmaceutical and Research Unit to standardize the research and development of traditional medicines.62
Fulfilling many of the central norms of the right to health, the Kingdom of Bhutan views GNH as a basis for the right to health, and, in turn, looks to the right to health as necessary for GNH.
Engaging human rights in the Kingdom of Bhutan
Yet restrictions of human rights in the Kingdom of Bhutan stem from its same GNH-based efforts to chart a distinctive course for health and development, with the government viewing minority “inundation” as a threat to the survival of the state and viewing restrictive citizenship policies as necessary safeguards for the Bhutanese GNH system.63 Similar to the repressive efforts of other rights-denying states that have sought to forge a national identity through the exclusion of minority populations, the Kingdom of Bhutan first established its “one nation, one people” policy in the 1990s as a means to frame the Bhutanese identity to realize its unique development objectives, justifying that:
The emergence of Bhutan as a nation state has been dependent upon the articulation of a distinct Bhutanese identity, founded upon our Buddhist beliefs and values, and the promotion of a common language. These have been defining elements in our history and they have made it possible to unify the country and to achieve national homogeneity and cohesion among various linguistic and ethnic groups. This identity, manifest in the concept of ‘one nation, one people’, has engendered in us the will to survive as a nation state as well as the strength to defend it in the face of threats and dangers.64
Rather than facilitating the multicultural national identity that had existed previously, this policy shift led to the persecution of non-Buddhist peoples, the mass exodus of minority populations, and the creation of large Bhutanese refugee populations outside of the Kingdom.65 Up to 100,000 Nepali-speaking Hindus (Lhotshampas) were expelled from the country throughout the 1990s—through violent repression, forcible eviction, or formal pressure—making their way to refugee camps in Nepal and thereafter excluded from Bhutanese citizenship and land ownership.66 Decried as a form of “ethnic cleansing,” with emptied southern agricultural lands subsequently given to landless northern Bhutanese citizens, such violations of minority rights brought international condemnation on the Bhutanese government.67
Responding to this condemnation, Bhutan initially sought to close itself off from the international human rights system, arguing that it had never ratified either of the UN’s human rights covenants: the International Covenant on Civil and Political Rights (ICCPR) and the ICESCR.68 By denying civil and political rights, the Bhutanese government sought to insulate itself from the ICCPR’s protection of minority rights.69 Yet, with these seminal ICCPR protections evolving to become the corpus of minority rights under international law, Bhutan continued to be criticized for violating the universal rights of the Lhotshampa minority.70
Based upon the General Assembly’s elaboration of minority rights in the 1992 Declaration on the Rights of Persons Belonging to National or Ethnic, Religious and Linguistic Minorities, the UN repeatedly questioned Bhutan’s denial of rights through the exclusion of citizenship, first in the Commission on Human Rights and then in the Human Rights Council.71 The Bhutanese government has come to ratify the Convention on the Elimination of All Forms of Discrimination against Women (CEDAW) and the Convention on the Rights of the Child (CRC), reporting on women’s and children’s rights to international treaty monitoring bodies; however, where the government continues to neglect the minority rights components of these adopted treaties, it has faced continuing international criticism—for example, from the Committee on the Rights of the Child for denying minority children the right to take part in Lhotshampa culture, practice the Hindu religion, or use the Nepali language.72
In spite of the promise of negotiations for the return of Lhotshampa refugees, very few refugees have been naturalized as Bhutanese citizens or permitted to return to their homes in Bhutan.73 Rather than engage these land tenure claims, Bhutanese government reports regularly exclude any mention of minority populations, linguistic differences, or cultural diversity.74 When the Kingdom of Bhutan has been pressed on the human rights of these excluded populations, the government has viewed these issues through the lens of terrorism and criminality, arguing that “the problem of the people in the refugee camps in eastern Nepal is not a typical refugee situation, but one of highly complex nature, with its genesis in illegal immigration.”75 With neither minority suffrage, independent media, nor civil society, the Kingdom of Bhutan continues to face international scrutiny for its violative policies.76
Despite this ongoing denial of minority rights, the Bhutanese government has begun to engage human rights as part of the Kingdom’s transition to democracy. Proceeding toward democracy without crisis, struggle, or revolution, this unique democratic transition over the past decade was driven and guided by the monarchy, which yielded considerable power to elites in the legislative and judicial branches while solidifying the majority Buddhist/Drukpa/Dzonkha identity.77 Even as the Constitution has been criticized for its neglect of religious, linguistic, and ethnic diversity—and specifically for the continuing exclusion of Lhotshampa refugees, reserving constitutional rights only to “citizens”—it has opened a space for human rights discourse, with Bhutan now acknowledging that “without the enjoyment of all human rights, Gross National Happiness, to which it is also deeply committed, cannot be achieved.”78
This democratic transition has led the government to express a renewed commitment to the international human rights system, with the drafters of the Bhutanese Constitution noting that they were “particularly influenced by South Africa’s [constitution] . . . because of its strong protection of human rights.”79 Engaging with the international human rights system in the aftermath of this democratic transition, however, has necessitated a purposeful effort to examine rights in isolation, looking to collective development rather than individual freedoms and noting that “respect for human rights such that rights to education, health and livelihoods complement abstract rights of equality before law.”80 Through this prioritization of collective happiness (of the majority citizens) over individual freedoms (of minority populations), the government has argued that GNH “lays the framework for the protection, promotion and integration of human rights into the fabric of Bhutanese society.”81
Participating in the UN’s Universal Periodic Review (UPR) process for the first time in 2009, the Bhutanese government focused on the strides it was taking to implement rights as part of the Kingdom’s nascent transition to democracy. While largely addressing women’s and children’s rights, framed by its treaty commitments to CEDAW and the CRC, the Kingdom of Bhutan reported on the progressive realization of health rights to these groups through the national primary health care system.82 Only when pressed during its UPR presentation did the Bhutanese delegation agree “that equal importance must be accorded to civil and political rights, and economic, social and cultural rights.”83 The interrelated rights of minority populations were raised repeatedly in the UPR process—in the state report and the country dialogue, leading to several concrete Working Group conclusions to address these cross-cutting human rights concerns—yet few steps were taken to resolve this issue prior to Bhutan’s second review in 2014.84
When Bhutan again presented information to the Human Rights Council, its second UPR report (a) linked GNH to the promotion of economic and social rights, (b) included a separate section on the “Right to Health,” and (c) noted tentative steps through which the transition to democracy had facilitated greater realization of civil and political rights.85 Repeatedly noting its deepening commitment to all human rights, the government concluded in both UPR reporting cycles that it will continue to consider the ratification of human rights instruments once it has developed the institutions and capacity necessary to meet these human rights obligations.
The paradox of human rights realization in rights-denying states
The Kingdom of Bhutan’s GNH-driven health system has met certain international obligations to progressively realize the right to health—receiving scant criticism on health issues in advocate reports and few recommendations on its health system in either UPR reporting cycle—yet Bhutanese health policy has nevertheless failed to meet cross-cutting human rights principles that underlie the right to health, including:
-
Equality and non-discrimination: With principles of non-discrimination ubiquitous across the international human rights system, Bhutan has made explicit its commitment to realize health without discrimination, but this commitment has fallen short with regard to minority populations. The government prioritizes women and children as “vulnerable groups” in national policy, in accordance with CEDAW and the CRC; however, data indicate that health inequality in Bhutan flows mostly along geographic lines, with large and persistent regional disparities in access to food security, potable water, and health care.86 Although the government has attributed geographic inaccessibility to “the rugged and difficult terrain” and “remoteness, sparse population and lack of reliable communication facilities,” these regional disparities are strikingly similar to the distribution of ethnic/religious/linguistic minorities, indicative of de facto (if not de jure) discrimination.87 Policies are needed to address the specific barriers to health care and underlying determinants of health for minority populations, particularly the Nepali-speaking Lhotshampas in southern Bhutan, who remain marginalized in policy and vulnerable in practice.88 Where the government has not released disaggregated health data based on ethnicity, religion, or language, it will be necessary for the government to understand these inequities through disaggregated indicators, developing a tailored response that prioritizes these minority groups in health policy.
-
Participation: Where a rights-based health system must develop “institutional arrangements for the active and informed participation” of “all relevant stakeholders,” Bhutan has long facilitated participation through a decentralized system of governance, extended through the Constitution’s authorization that:
Power and authority shall be decentralized and devolved to elected Local Governments to facilitate the direct participation of the people in the development and management of their own social, economic and environmental well-being.89
Although this constitutional decentralization was specifically justified as a means of facilitating participation through district administration of the health system, such decentralization efforts have given rise to problems in the supervision and monitoring of health programs.90 In facilitating meaningful local participation beyond the GNH Survey, VHWs can provide a crucial link between communities and the health system, with trusted VHWs who are “living permanently in the community,” and it will be crucial that VHWs come from the minority communities they serve.91 Ensuring minority voices in the health system, it will be additionally necessary to expand government authorization of minority civil society organizations in health. Replicating the success of organizations like Lhaksam, which represents HIV-positive populations and works with the Ministry of Health to reduce stigma, such mechanisms for civil society participation in the health system can assure acceptability in realization of the right to health.92
-
Accountability: In facilitating accountability as a cross-cutting human rights principle and key component of the right to health, Bhutan provides neither individual complaint mechanisms nor independent judicial authorities.93 In the absence of formalized adversarial means of enforcing rights against the state, the Bhutanese government relies on its GNH Index to assess the realization of happiness. Yet in assessing happiness, the GNH Surveys (on which almost 90% report themselves to be happy) have been criticized as highly subjective, reflecting habituation to persistent deprivations and imposing standards that may not reflect wellbeing.94 Further, although the GNH Index groups individual responses by sub-groups—disaggregating populations by age, district, gender, and occupation—this data disaggregation does not account for ethnic/religious/linguistic minority groups, obscuring any basis for discrimination claims.95 While the Ministry of Health has begun to administer National Health Surveys (NHS) to complement the GNH surveys, the Ministry remains limited in its ability to compile and analyze information on the quality and effectiveness of the health sector.96 To provide additional monitoring and evaluation mechanisms, the Ministry of Health has created the Bhutan Health Management and Information System (BHMIS) to assess information forwarded by each district health office, and it will be necessary to evaluate information on minority groups under new versions of the District Health Information System (Druk HMIS).97
While Bhutan has taken steps to progressively realize select norms of the right to health through its GNH approach to development, these efforts to assure happiness through the health system continue to violate the rights of minorities, impacting underlying determinants of health and undermining cross-cutting human rights principles. This paradox raises an imperative to assess cross-cutting human rights principles as interconnected obligations under the right to health, recognizing the ways in which human rights are indivisible, interdependent, and interrelated.
Without the unalloyed principles laid out by human rights, there can be no moral progress under international law, yet such failures should not blunt health policy reforms in the direction of greater humaneness and respect for the inherent dignity of the individual. Although scholars have noted a resistance to human rights in Southeast Asia, with some relativist authors arguing that “Asian” values are fundamentally different from “universal” human rights, it becomes clear in this case that Bhutanese values in the health system overlap substantially with select norms of availability, accessibility, acceptability, and quality under the right to health.98 Establishing a middle ground between universality and relativism, the Bhutanese government is not denying the existence of norms that protect health but rather constraining the norms included in its interpretation of the right to health, implementing certain norms of the right to health in isolation while denying cross-cutting principles necessary to a rights-based approach to health. These issues must be addressed as Bhutan continues to work with the international human rights system, analyzing the opportunities and limitations for human rights mainstreaming in the Bhutanese health system.
While acknowledging failures to implement a rights-based approach to health in Bhutan, this case study highlights the value of cross-cutting human rights principles in framing health system reforms. Bhutan has come to receive widespread approbation from human rights advocates for its failure to respect minority rights and implement human rights protections, and where the Bhutanese government has come to view the international human rights regime with intense suspicion, such suspicions may close off any formal advancement of the human right to health, with current health policy documents often neglecting even to mention human rights. The Bhutanese government’s continuing violations of minority rights—while egregious in failing to see the moral equality of all peoples—should not keep human rights advocates from working with policymakers in reforming the national health system to implement cross-cutting human rights principles pursuant to state obligations under human right to health.
Conclusion
Although the Kingdom of Bhutan has steadfastly sought to blunt the influence of global forces, seeking its own unique form of development under the GNH paradigm, it would be a mistake to assume that the international human right to health has no place in framing a rapidly evolving Bhutanese health system. Where the human rights system lacks a basis to prioritize human rights, it is necessary to study how different cultures navigate tradeoffs between rights-based norms and principles in seeking to realize the right to health. The human right to health is transforming the world, and the human rights community must understand the ways in which this international human right is implemented through national health systems, conceptualizing human rights implementation in states that deny the existence of individual freedoms while seeking to realize public health. As the Bhutanese government moves beyond GNH and integrates itself further in the international human rights system, scholars must clarify the importance of cross-cutting human rights principles to the human right to health—addressing universal threats to dignity, framing health system reforms, and assuring the highest attainable standard of health.
Benjamin Mason Meier is an Associate Professor of Global Health Policy at the University of North Carolina, Chapel Hill, NC, USA.
Averi Chakrabarti is a Doctoral Student in the Department of Public Policy at the University of North Carolina, Chapel Hill, NC, USA.
Please address correspondence to the authors c/o Benjamin Mason Meier, Department of Public Policy, 103 Abernethy Hall, University of North Carolina, Chapel Hill, NC 27599. Email: bmeier@unc.edu
References
- D.A. Andelman, “Bhutan, borders, and bliss,” World Policy Journal 27/1 (2010), pp. 103-111: p. 107; J. Rosen, “Bhutan: A Higher State of Being,” New York Times (October 30, 2014).
- S. Giri, The vital link: Monpas and their forests (Thimphu, Bhutan: The Centre for Bhutan Studies, 2004).
- G.W. Burns, “Gross National Happiness: A Gift from Bhutan to the World,” in R. Biswas-Diener (eds), Positive Psychology as Social Change (New York: Springer, 2011), pp. 73-87; M. Mancall, “Gross national happiness and development: An essay,” in K. Ura and K. Galay (eds), Gross National Happiness and Development (Thimphu, Bhutan: The Centre for Bhutan Studies, 2004), pp. 3-5.
- J. Temperman, State-Religion relationships and human rights law: Towards a right to religiously neutral governance (Leiden, The Netherlands: Martinus Nijhoff Publishers, 2010), p. 59; Kingdom of Bhutan, The Constitution of the Kingdom of Bhutan (Kingdom of Bhutan), pp. 2, 9-10. Available at http://www.wipo.int/wipolex/en/text.jsp?file_id=167939.
- D. Rizal, “The unknown refugee crisis: Expulsion of the ethnic Lhotsampa from Bhutan,” Asian Ethnicity 5/2 (2004), pp. 151-177.
- Ibid., p. 153.
- G. van Driem, “Language policy in Bhutan,” in M. Aris and M. Hutt (eds), Bhutan: Aspects of culture and development (Gartmore, UK: Kiscadale, 1994).
- S.O. Wolf, “Bhutan’s political transition – Between ethnic conflict and democracy,” Spotlight South Asia, SSA 2 (2012), pp. 6, 14.
- K. Ura, “Development and decentralisation in medieval and modern Bhutan,” in M. Aris and M. Hutt (eds), Bhutan: Aspects of culture and development (Gartmore, UK: Kiscadale, 1994), pp. 40-42; A, Thomson, Thematic paper on decentralization and local empowerment (Ministry of Foreign Affairs/Denmark and Gross Happiness Commission/Bhutan, 2010), p. 6.
- The new development paradigm, history. Available at http://www.newdevelopmentparadigm.bt/about-us/history/.
- K. Ura, S. Alkire, T. Zangmo, and K. Wangdi, A short guide to gross national happiness index (Thimphu, Bhutan: The Centre for Bhutan Studies, 2012), p. 6.
- S. Priesner, “Gross national happiness–Bhutan’s vision of development and its challenges,” in S. Kinga, K. Galay, P. Rapten and A. Pain (eds), Gross national happiness: A set of discussion papers (Thimphu, Bhutan: The Centre for Bhutan Studies, 1999), p. 28.
- S. Murugan, Gross national happiness through ICTs for development: A case study of the Jakar community multimedia center (Thimphu, Bhutan: The Centre for Bhutan Studies, 2007). pp. 172-187.
- Bhutan foundation, Bhutan believes in gross national happiness. Available at http://www.bhutanfound.org/?p=151.
- Kingdom of Bhutan, The Constitution of the Kingdom of Bhutan, p. 18.
- T. Tobgay, U. Dophu, C.E. Torres, and K. Na-Bangchang, “Health and gross national happiness: Review of current status in Bhutan,” Journal of Multidisciplinary Healthcare 4 (2011), pp. 731-736.
- Ura et al. (see note 9), pp. 1-3, 8.
- Ibid., pp. 1-2.
- Kingdom of Bhutan, Ministry of Foreign Affairs, National report submitted in accordance with paragraph 5 of the annex to Human Rights Council resolution 16/21 (Bhutan, Ministry of Foreign Affairs, 2014), p. 12.
- T.W. Ryback, “The U.N. happiness project,” The New York Times (March 28, 2012).
- R. Beaglehole, and R. Bonita. “Development with values: Lessons from Bhutan,” Lancet 385 (2015), p. 849.
- United Nations General Assembly, G.A. Res. 66/281 (2012). Available at http://www.un.org/en/ga/search/view_doc.asp?symbol=%20A/RES/66/281.
- Constitution (see note 15)
- Kingdom of Bhutan (see note 19) pp. 9-10.
- Stephen P. Marks, The human rights framework for development: Seven approaches (François-Xavier Bagnoud Ctr. for Health & Human Rights, Harvard Sch. of Pub. Health, Working Paper No. 18, 2003).
- Ministry of Health, National health policy (Thimphu: Ministry of Health, 2011). Available at http://www.gnhc.gov.bt/wp-content/uploads/2012/04/nationalHpolicy.pdf.
- Ibid.
- National Portal, Government of Bhutan, Ministries. Available at http://www.bhutan.gov.bt/government/ministries.php
- Centre for Bhutan Studies & GNH Research, Health. Available at http://www.grossnationalhappiness.com/9-domains/health/
- M.A. Gosai & L. Sulewski, “Urban attraction: Bhutanese internal rural–urban migration,” Asian Geographer 31:1 (2014), pp. 1-16.
- UNICEF, What works for children in South Asia: Community health workers (UNICEF: 2004), p. 10. Available at http://www.unicef.org/rosa/community.pdf.
- UN Capital Development Fund and Royal Government of Bhutan, Primary schools and Basic Health Units in Eastern Bhutan (United Nations Capital Development Fund and Royal Government of Bhutan , 2001). Available at http://erc.undp.org/evaluationadmin/manageevaluation/viewevaluationdetail.html?evalid=1446; S.D. Morris-Jones, “Tales of the unexpected: The Basic Health Unit in Bhutan,” British Medical Journal 291 (1985), p. 878.
- Human Resources Division, Ministry of Health, Human resources for health country profile Bhutan, (Ministry of Health: 2014). p. 13. Available at http://www.searo.who.int/entity/human_resources/data/Bhutan_HRH_Country_Profile.pdf
- Constitution (see note 15).
- Parliament of Bhutan, The water act of Bhutan 2011 (Thimphu, Bhutan: Parliament of Bhutan, 2011). Available at http://faolex.fao.org/docs/pdf/bhu106322.pdf; WHO Bhutan: Health profile. Available at http://www.who.int/gho/countries/btn.pdf?ua=1.
- Taiwo A. Oriola, Ethical and legal analyses of policy prohibiting tobacco smoking in enclosed public spaces, Journal of Law, Medicine and Ethics; 37(4): 828-840 (2009).
- WHO (see note 35).
- Ministry of Foreign Affairs of Denmark, Joint evaluation: Danish-Bhutanese country programme 2000-09. Synthesis Report (Oxford Policy Management, 2010), p. 50.
- WHO (see note 35).
- WHO (see note 35)
- D. Wangchuk, N.K. Virdi, R. Garg, S. Mendis, N. Nair, D. Wangchuk, and R. Kumar, “Package of Essential Noncommunicable Disease (PEN) Interventions in Primary Health-care Settings of Bhutan: A Performance Assessment Study,” WHO South-East Asia Journal of Public Health 3/2 (2014), pp. 154-160: p. 155.
- UN Committee on Economic, Social, and Cultural Rights, General Comment No. 14, The Substantive Issues Arising in the Implementation of the International Covenant on Economic, Social, and Cultural Rights, UN Doc. No. E/C.12/2000/4 (2000); P. Hunt and G. Backman, “Health Systems and the Right to the Highest Attainable Standard of Health,” Health and Human Rights 10 (2009). pp. 81-92.
- G. Backman, P. Hunt, R. Khosla, C. Jaramillo-Strouss, B.M. Fikre, C. Rumble, D. Pevalin, “Health Systems and the Right to Health: An Assessment of 194 Countries,” The Lancet 372/9655 (2008), p. 2050.
- General Comment 14 (see note 42) ¶12.
- Ministry of Health, Royal Government of Bhutan. Annual Health Bulletin 2015 (Thimphu: Ministry of Health 2015), p. 104. Available at http://www.health.gov.bt/wp-content/uploads/ftps/annual-health-bulletins/AHB_2015_FINAL_9Jul2015.pdf.
- R. Pelzang, “Mental Healthcare in Bhutan: Policy and Issues,” WHO South-east Asia Journal of Public Health 1/3 (2012), pp. 339-346.
- Human Resources Division, Ministry of Health (see note 45), p. 23.
- Khesar Gyalpo University of Medical Sciences in Bhutan. Available at http://www.umsb.edu.bt/index.php; Ministry of Foreign Affairs of Denmark (see note 38), p. 46; Human Resources Division, Ministry of Health (see note 45), p. 24.
- M. Stapleton, Bhutan Essential Drugs Programme: A Case History (World Health Organization: 2000), pp. xiii-xiv. Available at http://apps.who.int/medicinedocs/documents/s19041en/s19041en.pdf; WHO (see note 35).
- Backman et al. (see note 43) p. 2052.
- Ministry of Foreign Affairs of Denmark (see note 38), p. 44. M. Drexler, “The Road to Health and Well-being,” Harvard School of Public Health (Winter 2013). Available at https://www.hsph.harvard.edu/news/magazine/the-road-to-health-and-wellbeing/.
- UNICEF (see note 31), pp. 9-10.
- Bhutan Health Trust Fund, Ministry of Health, About BHTF. Available at http://www.bhtf.bt/about-us/about-bhtf/; Tobgay et al. (see note 16) p. 734.
- Kingdom of Bhutan, National Report Submitted in Accordance with Paragraph 15(A) of the Annex to Human Rights Council Resolution 5/1 (Report Submitted for the Universal Periodic Review) (Bhutan, 2009), p. 18 ; Tobgay et al. (see note 16), p. 732.
- Andelman (see note 1), p. 107; Backman et al. (see note 43), p. 2051.
- Ministry of Health, Royal Government of Bhutan, Annual Health Bulletin (Thimphu: Ministry of Health, Royal Government of Bhutan, 2014), p. 112. Available at http://www.health.gov.bt/wp-content/uploads/ppd-files/health-bulletins/bulletins/ahb2014/ahbContent2014.pdf.
- Drexler (see note 51); Timmins, “Bhutan Supports Dual Medicine,” Daily Press (June 18, 2001).
- Kingdom of Bhutan (see note 54), p. 10.
- B.M. Meier, L. Gable, J.E. Getgen, and L. London, Rights-Based Approaches to Public Health in E. Beracochea, C. Weinstein, and D. Evans (eds), Rights-Based Approaches to Public Health, (New York: Springer, 2010), p. 23; Backman et al. (see note 43) p. 2051.
- Ministry of Foreign Affairs of Denmark (see note 38) p. 44.
- Ibid., p. 45.
- Department of Medical Supplies, Ministry of Health, Royal Government of Bhutan, National drug policy 2007 (Department of Medical Supplies, 2007). Available at http://www.searo.who.int/entity/medicines/nmp_bhu_2007_who_ok.pdf. M. Stapleton, Bhutan essential drugs programme: A case history (World Health Organization: 2000), pp. xiii-xiv. Available at http://apps.who.int/medicinedocs/documents/s19041en/s19041en.pdf; Tobgay et al (see note 16), p. 735.
- UN General Assembly, Report of the working group on the universal periodic review-Bhutan, A/HRC/13/11 (January 4, 2010), p. 4.
- Planning Commission, Royal Government of Bhutan, Bhutan 2020: A vision for peace, prosperity and happiness, Part I (1999), p. 18.
- M. Hutt, “Ethnic nationalism, refugees and Bhutan,” Journal of Refugee Studies 9/4 (1996), pp. 397-420.
- M. Hutt, Unbecoming citizens: culture, nationhood and the flight of refugees from Bhutan (New York: Oxford University Press, 2003); Amnesty International, Nationality, expulsion, statelessness and the right to return (2000); Bill Frelick, For Bhutan’s refugees, There’s no place like home, March 30, 2011. Available at
- http://www.hrw.org/news/2011/03/30/bhutan-s-refugees-there-s-no-place-home.
- Amnesty International, Bhutan: Forcible Exile (1994); F. de Varennes, “Constitutionalising discrimination in Bhutan: The emasculation of human rights in the land of the dragon,” Asia-Pac. J. on Hum. Rts. & L. 2 (2008), pp. 47-76.
- UN Office of the High Commissioner of Human Rights, Status of ratification interactive dashboard, Available at: http://indicators.ohchr.org/.
- UN General Assembly, International Covenant on Civil and Political Rights, 1966: art. 27.
- Amnesty International, Bhutan: Human rights violations against the Nepali-speaking population in the South (1992); Human Rights Watch, Last hope: The need for durable solutions for Bhutanese refugees in Nepal and India (2007).
- UN General Assembly, Declaration on the rights of persons belonging to national or ethnic, religious and linguistic minorities, A/RES/47/135, adopted on 18 December 1992; D. Weissbrodt, M. Gómez, and B. Thiele, “An analysis of the fifty-first session of the United Nations Sub-Commission on the Promotion and Protection of Human Rights,” Human Rights Quarterly 22/3 (2000), pp. 788-837; UN General Assembly (see note 69).
- Committee on the Rights of the Child. 2008. Forty-Ninth Session: Consideration of reports submitted by states parties under article 44 of the convention.
- U.S. Department of State, Country reports on human rights practices for 2011 (Washington: Bureau of Democracy, Human Rights, and Labor, 2012).
- R. Evans, “The perils of being a borderland people: on the Lhotshampas of Bhutan,” Contemporary South Asia 18/1 (2010), pp. 25-42.
- Kingdom of Bhutan (see note 54), p. 15.
- U.S. Department of State, (see note 73).
- M. Gallenkamp, “When agency triumphs over structure: Conceptualizing Bhutan’s unique transition to democracy,” in Heidelberg papers in South Asian and comparative politics 68 (2012); W. Bothe, “In the name of king, country, and people on the Westminster Model and Bhutan’s constitutional transition,” Democratization (2015).
- Kingdom of Bhutan (see note 54), p. 22 (emphasis added); L. Pellegrini and L. Tasciotti, “Bhutan: Between happiness and horror,” Capitalism Nature Socialism 25/3 (2014), pp. 103-109.
- E. Newburger, “Elevation,” Harvard Law Bulletin (2007), p. 28. Available at http://today.law.harvard.edu/feature/elevation/.
- Bhutan: Poverty reduction strategy paper, IMF Country Report No. 04/246, August 2004 (emphasis added).
- Kingdom of Bhutan (see note 54), p. 6.
- Ibid., pp. 6-9.
- UN General Assembly (see note 69), p. 4.
- Kingdom of Bhutan, Responses to recommendations (June 18, 2012). Available at http://www.upr-info.org/sites/default/files/document/bhutan/session_6_-_november_2009/recommendationstobhutan2009.pdf.
- Kingdom of Bhutan (see note 54), p. 9.
- Kingdom of Bhutan, (see note 54), p.16; U. Zangmo, M. de Onis and T. Dorji, “The nutritional status of children in Bhutan: Results from the 2008 national nutrition survey and trends over time,” BMC Pediatrics 12/151 (2012), pp. 1-7. Available at http://www.biomedcentral.com/1471-2431/12/151/; WHO (see note 35).
- Department of Planning, Ministry of Finance and National Statistical Bureau, Poverty and inequality in Bhutan (Department of Planning, Ministry of Finance and National Statistical Bureau, 2004), pp. 1-2. Available at http://www.nsb.gov.bt/publication/files/pub10ks2884sy.pdf.
- Committee on Economic, Social and Cultural Rights, General Comment No. 20, Non-discrimination in economic, social and cultural rights; 2009; S. Qiu, “Equality and the right to health: A preliminary assessment of China,” in B. Toebes et al. (eds), The right to health: A multi-country study of law, policy and practice (New York: Springer, 2014).
- Backman et al. (see note 43), p. 2051; Thomson (see note 9), p. 2; Constitution (see note 4).
- Ministry of Foreign Affairs of Denmark (see note 38), p. 46.
- UNICEF (see note 31), p. 9.
- Kingdom of Bhutan (see note 54), p. 10; H. Potts, Participation and the right to the highest attainable standard of health (2009).
- A.E. Yamin, “Beyond compassion: The central role of accountability in applying a human rights framework to health,” Health and Human Rights 10/2 (2008), pp. 1-20.
- A.A. Braun, “Gross national happiness in Bhutan: A living example of an alternative Approach to Progress,” Social Impact Research Experience Journal (2009), pp. 33-38; W. Bates, “Gross National Happiness,” Asian-Pacific Economic Literature (2009), p.12.
- Ura et al. (see note 11), p. 1.
- Ministry of Health, Annual Report of the Ministry of Health: 1st Year of the 11th Five Year Plan (2013-2014) (Ministry of Health: 2014), p. 1, 4.
- Ministry of Health (see note 96), p.10; Tobgay et al (see note 16), pp. 731-736.
- J. Donnelly, “Human rights and Asian values: A defense of ‘Western universalism,’” in The East Asian Challenge for Human Rights (Cambridge: Cambridge University Press, 1999); Human rights and Asian values: Contesting national identities and cultural representations in Asia (Michael Jacobsen & Ole Bruun eds., 2000).