Vol 25/1, 2023, pp. 105-117 PDF
Luis Martin Ortega, Michael J. Westerhaus, Amy Finnegan, Aarti Bhatt, Alex Olirus Owilli, Brian Turigye, and Youri Encelotti Louis
Abstract
Global health equity is at a historically tenuous nexus complicated by economic inequality, climate change, mass migration, racialized violence, and global pandemics. Social medicine, collective health, and structural competency are interdisciplinary fields with their own histories and fragmentary implementation in health equity movements situated both locally and globally. In this paper, we review these three fields’ historical backgrounds, theoretical underpinnings, and contemporary contributions to global health equity. We believe that intentional dialogue between these fields could promote a generative discourse rooted in a shared understanding of their historical antecedents and theoretical frameworks. We also propose pedagogical tools grounded within our own critical and transformative pedagogies that offer the prospect of bringing these traditions into greater dialogue for the purpose of actualizing the human right to health.
Introduction
Health workers concerned about the human right to health have reason to be wary as they observe the world around them. Despite a pandemic-triggered global economy slowdown, human consumption continues to generate dangerous levels of greenhouse gasses, pushing carbon dioxide levels to their highest in three million years.1 During the first two years of the COVID-19 pandemic, profit-driven economic systems crowned a new billionaire every 30 hours while pushing one million people toward extreme poverty every 33 hours. Forty of these new billionaires are pharmaceutical executives.2 Colonial imprints, white supremacy, and racial capitalism contours and textures both public and private care systems in ways that create patterns of advantage for white-identified and wealthy individuals and disadvantage for (largely poorer) black- and brown-identified individuals in their encounters with COVID-19.3 The consequences of these upstream forces are health inequities experienced as biological pathology. By upstream, we refer to the social, political, and economic contexts that structure society and are “manufacturers of illness,” such as profit-making institutions.4 Generative mechanisms in society that positively influence well-being are also examples of upstream social forces, such as equitable transportation, healthy rivers and wetlands, and community practices imbued with an ethos of care.
The recalcitrant persistence of health inequities experienced across both local and global contexts has intensified interest in frameworks that claim to diagnose the root causes of these inequities accurately. Prominent among these interdisciplinary fields are social medicine, collective health, and structural competency, all of which also offer a complementary set of prescriptions to remedy inequitable outcomes.5 Some argue that the intensified interest at this moment is simply a cyclical rediscovery of historically well-described relationships between oppressive social conditions that structure risk for illness.6 Others believe that the intensified interest and energy, pressured by the emergency context of climate catastrophe, ongoing racial injustice, and a global pandemic, signal something different. They hold the hope that disruptive and generative social change will move the global community toward actual fulfillment of article 25 of the Universal Declaration of Human Rights, which states that “everyone has the right to a standard of living adequate for the health and well-being of himself and of his family.”7
Social medicine, collective health, and structural competency share core commonalities in their assertion that health is a human right generated not in the biological domain but in the upstream determination of health. This is often akin to the contemporary reference within human rights literature to civil, political, social, cultural, and economic rights. All three of these fields focus on the (re)production of health and systems of care, as well as the political economies that aid or obstruct the realization of public health as a social good. They are each interdisciplinary fields linked with social change projects with broad agendas encompassing the social response to societal ills. All three grew out of academic contexts, and their adherents publish on and organize thematic conferences focused on health justice.
Despite their shared ideological interest in health justice and remedying health inequities, practitioners and scholars in the fields of social medicine, collective health, and structural competency engage in minimal dialogue. Possible reasons for the lack of dialogue include their origins in different geographic, linguistic, and historical contexts, territorialism, academic advancement linked to the generation of novel concepts and language, and the belief that new conceptualizations expanding beyond existing theories and actions are required to eliminate health inequities. Whatever the reason, the lack of exchange and engagement diminishes the possibilities of relationship-building, theoretical expansion, imaginative problem-solving, and the collective building of power needed for social change toward health justice. In short, we believe that the lack of dialogue isolates and minimizes the potential for all three to substantively contribute to the movement seeking to ensure health as a human right for all.
In this paper, our goal is to ignite intentional dialogue among these three fields by (1) juxtaposing their definitions, geographic and historical journeys, and key frameworks and themes, (2) proposing that transformative pedagogy offers one strategy to foster dialogue, and (3) providing concrete examples of what such pedagogy might look like. We illustrate these points by drawing on our collective experience as a transnational group of social medicine educators and practitioners.
Contemporary summaries of social medicine, collective health, and structural competency
We first turn to an examination of the three fields—social medicine, collective health, and structural competency—that highlights the history, central tenets, and theoretical influences of each.
Social medicine
Social medicine is an interdisciplinary field that is over a century old. In the early to mid-19th century, European countries faced many social challenges, including increasingly low wages for the working class, poor working conditions, and a lack of housing and sanitation facilities. These population outcomes alarmed a group of reformist French physicians and hygienists to investigate the relationships between health problems and social conditions.8 They quickly realized the pervasive influence of social factors on health and disease. German pioneers of the field promoted health care reform after the revolution in March 1848. They proposed three basic principles regarding the academic and practical aspects of social medicine: (1) the health of the population is a matter of direct social concern; (2) social and economic conditions have an important effect on health, disease, and the practice of medicine, and these relations must be subjected to scientific investigation; and (3) steps must be taken to promote health and to combat disease, and the measures involved in such action must be social as well as medical.9
Social medicine was introduced to Latin America and the United States in the 20th century (though it has historically had limited uptake in the latter setting owing in significant part to a persistent political aversion to “socialist” forces in the medical industrial complex).10 This marked a “golden age” of social medicine during troubled times throughout the Latin American region, where local institutions of authority were coopted by transnational interests at the expense the common people. Leaders thus emerged from Chile, Brazil, Cuba, Ecuador, and Argentina to advance theories on the social roots of illness and action-oriented initiatives.11 This field has also taken inspiration from intersecting fields of liberation theology, empowerment practices in popular education, political revolutions in Cuba and Nicaragua, and a repressed peaceful transition to a socialist paradigm in Chile. Social medicine contrasts with public health “in its definitions of populations and social institutions, its dialectic vision of ‘health-illness’, and its stance on causal inference,” offering analyses that go beyond identifying relatively static mono- or multi-factorial accounts of decontextualized risk factors for health-illness and offering “a more complex approach to causality, in which social and historical conditions receive more explicit emphasis.”12 Social medicine traditions have advanced shared ideals of democracy, egalitarianism, and capacity- and community-building—all ideals grounded within a tradition of praxis (reflection and action upon the world in order to transform it).13 A strength identified within social medicine is the emphasis on the linkage of theory and practice, as leaders have emphasized theory that “both informs and takes inspiration from efforts toward social change.”14
More recently, at the Social Medicine Consortium conference in 2016 in Minneapolis, United States, a global group of educators and practitioners defined social medicine through consensus as a practice that integrates (1) understanding and applying the social determinants of health, social epidemiology, and social science approaches to patient care; (2) an advocacy and equity agenda that treats health as a human right; (3) an approach that is both interdisciplinary and multisectoral across the health system; (4) a deep understanding of local and global contexts which ensures that the local context informs and leads the global movement; and (5) voice and vote of patient, families, and communities.15 Some scholars at the intersection of Latin American social medicine and collective health have proposed a more active language focus on the social determination of health as a focus on the dynamic nature of how health-illness is (re)produced.16
Collective health
Collective health emerged in Brazil in the 1970s as an interdisciplinary field focused mainly on epidemiology, social sciences in health, and health policy, planning, and management. While largely centered in Brazil at its inception, collective health has grown in importance throughout Latin America, with particularly strong threads emerging in Argentina, Uruguay, and Ecuador in the 1990s. The field was born out of the medical education reform project of preventive medicine and the broader, recursive historical movement of social medicine. It has been connected to grassroots struggles for democracy and health reform movements. Collective health views health and disease as a social process and “investigates the production and distribution of diseases in society as processes of social production and reproduction.” It attempts to understand the forms with which society identifies its health needs and problems, looks for an explanation, and then organizes itself to face them.17
A strength identified within collective health has been the proposal to organize in both horizontal and vertical directions. The horizontal organization of collective health refers to a social movement oriented toward the professional health-allied community, as well as lay people across society advocating for health as a human right. Vertical organization refers to the intentional development of subject-matter experts in the field such that specialized knowledge can be brought to bear on more complex problems.18 Thus, collective health has strength in its inherent value of “democratizing” the arena of health as an expanded human right to all stakeholders. It commits to a collective praxis of the social determination of health in a way that is inclusive to experts and common citizenry alike, in horizontal and vertical levels. This is in contrast to social medicine, which has been described as having a “key aim … to work against vertical approaches that have historically dominated global health interventions.”19
Structural competency
Structural competency is also a relatively new curricular framework for training health professionals (with predominant historical roots in the United States) to recognize and respond to disease and its unequal distribution, which comes about as the outcome of harmful social structures such as policies, institutions, and systems. Structural competency explicitly engages with the root causes and the “structural violence” naturalized and (re)produced within the status quo. Structural competency was initially developed as a framework to reform medical education paradigms in ostensibly domestic Global North settings with no apparent specific focus on global health.20 However, it is increasingly being put forth as one response to “decolonize” global health and meaningfully engage with structural drivers of global health inequity.21
Structural competency offers strengths in its proposed framework of sub-competencies for global health education (a relatively recent development with structural competency, as its gaze was historically focused on local medical education endeavors) developed by scholars from the Global North and Global South who have developed and taught curricula related to global health, social medicine, and structural inequality. These sub-competencies include being able to
(1) describe the role of social structures in producing and maintaining health inequities globally, (2) identify the ways that structural inequalities are naturalized within the field of global health, (3) discuss the impact of structure on the practice of global health, (4) recognize structural interventions for addressing global health inequities, and (5) apply the concept of structural humility in the context of global health.22
One key strength within structural competency is that practitioners have demonstrated a remarkable ability to build cross-institutional and -organizational relationships via their development and delivery of structural competency training to diverse audiences of health care professionals.23 We highlight the inclusion of sub-competency 5 of structural humility—“a self-reflective approach to addressing the structural determinants of health that requires partnering with individuals and communities to inform understandings of structural violence and to explore how best to respond to it.”24 We feel that it relates closely to our pedagogical localization of the “personal” within our 3Ps educational model described in further detail below. Despite scholars proposing concrete sub-competencies within this field, there remain identified needs to “further refine and operationalize the competencies proposed here into curricula, to develop relevant pedagogy, and to evaluate its effects on trainee knowledge, skills, and real-world impact.”25
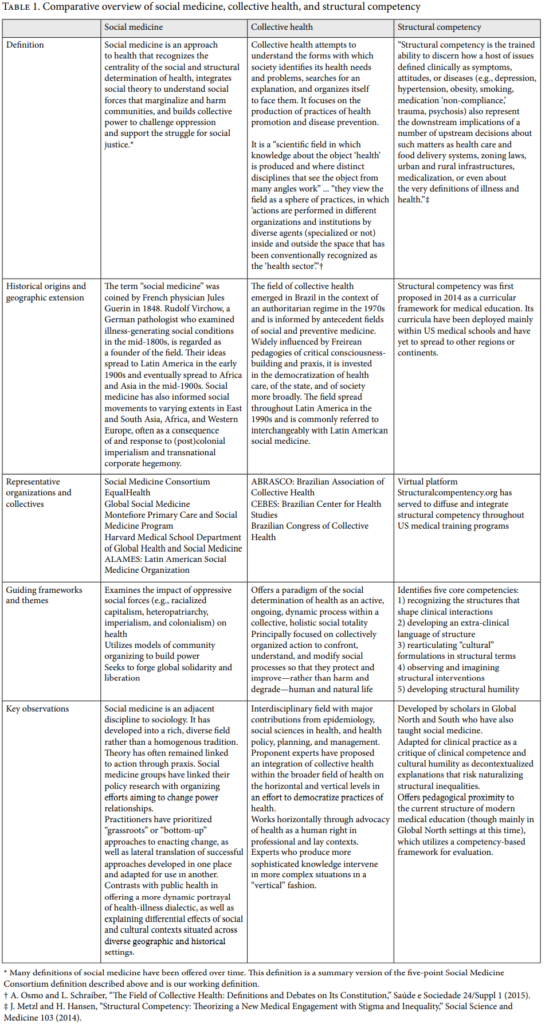
Table 1 summarizes each of the three fields. This work is not a comprehensive review of the fields but rather an examination of how they have contributed to the broader social movement of health and human rights. Significant overlap and interconnection exists between these fields.
In summary, social medicine, collective health, and structural competency are interrelated, interdisciplinary, evolving fields that have recursively grappled with health inequities in their unique histories against increasingly globalized oppressive phenomena impacting historically marginalized and dispossessed communities. There lies an opportunity within global health equity as a social change project to develop a common language and integrated framework for analysis within these fields toward more concrete and collaborative curricular design and evaluation oriented toward transformative learner outcomes linked with social change. Collective health has proposed a “democratized” arena of horizontal and vertical levels of knowledge and practice such that health can be more broadly conceptualized as an expanded human right and such that change can be facilitated by more specialized agents according to the complexity of situations. Structural competency has proposed structural humility such that structural interventions might be more readily adapted and accepted to diverse localized contexts according to social, cultural, and political differences. Social medicine has proposed a linkage between theory and practice (praxis) such that theory both informs and takes inspiration from collective social change efforts.
Transformative pedagogy and building critical consciousness
Given the cross-disciplinary commitment to social change shared by social medicine, collective health, and structural competency, educating practitioners across all three traditions requires pedagogy that catalyzes learner transformation. Jack Mezirow and Edward Taylor define transformative learning as “learning that transforms problematic frames of reference to make them more inclusive, discriminating, reflective, open, and emotionally able to change.” They contend that transformative learning requires a combination of individual experience, critical reflection, dialogue, holistic orientation, awareness of context, and authentic relationships. Ultimately, transformative learning, “require[s] that the learner make an informed and reflective decision to act or not.”26 In other words, success in transformative learning is based not on cognitive measures but rather on learner action or inaction in the world. The central evaluative question following a transformative learning experience then becomes not what knowledge has been gained but rather: Are the learners now acting and engaging differently with themselves and the world around them?
Transformative learning experiences create the conditions for the emergence of critical consciousness. Drawing on the work of Paulo Freire, we understand critical consciousness to involve problematizing the reality of the world in its causal and circumstantial correlations; awakening to the totality of the world and one’s place in it; recognizing the self as an active subject in the world working with other subjects to transform the world; and expanding one’s sense of possibility and imagination through a gritty relationship with the world. Freire posited that critical consciousness arises through an iterative process of de-coding in which “the consciousness … rebuilds its power of reflection in the ‘entering into’ of present understanding which progresses towards a new understanding.”27 Critical consciousness, though, is not just a heightened state of awareness about the sources of the world’s ills. Rather, it is the coupling of that heightened state of awareness with an awakened sense of one’s agency to transform those ills.
Transformative learning that cultivates critical consciousness requires deconstructing traditional “banking” models of education that treat learners as passive receptacles for information dumping and conceptualize the body and mind as separate agents.28 Traditional human rights and global health education models often align with Western banking models of education that exist “as an arena of domestication, where abstract knowledge and its constructions are decontextualized, disembodied, and objectified.”29 Domesticating educational processes intensify both social contextual and bodily estrangement, which can “cause false dichotomies that alienate students from their material world—the only true realm from which liberatory education can be forged.”30
If we genuinely seek human rights education with liberatory potential, critical attention and labor must be put toward human rights education that counters domesticating forces. Education rooted in dialogue is central for accomplishing this. As noted by Denis Goulet in his introduction to Freire’s Education: The Practice of Freedom, “The mark of a successful educator is not skill in persuasion—which is but an insidious form of propaganda—but the ability to dialogue with educatees in a mode of reciprocity.”31 In our experience, dialogue must, however, expand beyond its traditional conceptualization as two cognitive beings engaged in an exchange of information. Generating critical consciousness requires us to envision dialogue as a dynamic process that involves the circulation of information, sensation, and emotion between minds, bodies, hearts, and place/land. We must welcome the invitation toward a revolutionary praxis of the body in which we recognize how the body plays a significant role in making sense of the material conditions and social relations of power that shape human and non-human life and land.
A model of social medicine education
EqualHealth has centered transformative pedagogy since its origins. As a collective of health workers and educators from both Global North and Global South contexts, a handful of us first came together in 2010 in Northern Uganda, dissatisfied with traditional educational content and the missed opportunities for relationality among peers in our global health endeavors. For more than 10 years, we, the authors, have taught social medicine in three different institutional and sociopolitical contexts—Sub-Saharan Africa, particularly Uganda and Rwanda; Haiti; and the United States. Over this time spent implementing and reforming the social medicine courses, the learners’ reach stretches across four continents of Africa, Asia, North America, and Europe. It is, in fact, the transnational nature of our relationships and work that brought us into encounter with these three fields, whose roots and histories lie in diverse geographic contexts. Today, EqualHealth is a nonprofit organization that centers building critical consciousness and collective action globally in pursuit of health equity, with intentional anchors in Uganda and Haiti. We, the authors of this paper, from Uganda, Haiti and the United States, among other colleagues, have taken up leadership roles within EqualHealth. Our programs include social medicine courses in Uganda, Haiti, and the United States, as well as the Campaign Against Racism, a global action-focused collective with 21 member-based chapters from nine countries seeking to dismantle racialized capitalism in health care.
Our social medicine courses are the central mechanism for our transformative pedagogy work. These courses seek to engage students in the praxis of health equity, the social and structural determination of health, the principles and practice of global health in local settings, and leading change. They are topically organized to foster an examination of oppressive social forces and liberating practices. Oppressive social forces (e.g., heteropatriarchy, racism, racialized capitalism, settler colonialism, and imperialism) are historicized and politicized to debunk the standard perception that they are naturally occurring, essentialized phenomena of the world.
Our original courses consisted of three- to four- week immersion programs in Uganda and Haiti, with learners from the Global North and the Global South living and studying together for the immersive period. In recent years, due to the global COVID-19 pandemic and heightened concern over the climate impact of global travel, we have adapted our curricular structure and content to offer three simultaneous social medicine courses in the United States, Uganda, and Haiti. Within these courses, we create space for intentional transnational dialogue across the parallel cohorts, seeking to foster conditions to build solidarity and mutual understanding of the differential effects of globalized social forces. Across all three sites, we explore what creating conditions for healing, health, and safety means in our lived communities through exposure to community organizing, mutual aid and community-based care, embodied healing practices, the arts, and storytelling. This content provides rich opportunities to develop the organizing, relational, and creative skills that are foundational for advancing health equity in partnership with communities. Detailed descriptions of the course content have been published elsewhere.32
EqualHealth grounds its learning model in the 3Ps—praxis, personal, and partnership—as a means of fostering transformative outcomes for learners, teachers, and practitioners alike. We aim to destabilize traditional hierarchies of power found in global health communities by invoking practices of mutuality and reciprocity, where all participants can engage one another as peers. This learning model aims to build critical consciousness, described above. In practice, place-based and embodied learning has inspired students to identify, analyze, and strategize to resist repressive policies, albeit functioning within an authoritarian system.33
The notion of praxis is inspired by Freire, in which pedagogues are co-creating the conditions for a constant interplay between reflection and action (alongside learners and other stakeholders).34 Educators are present not to deposit knowledge into students’ minds but rather to co-create knowledge alongside participants. Everyone involved in education, then, is a learner, and learning activities are not just listening to expert speakers, watching films, or reading texts; learning also includes both meaningful dialogue and opportunities to act in the world. The courses intentionally center connections with local community members as well as those from outside the traditional health disciplines to birth creativity, inspire imagination, build relationships, and foster connections essential to engaging social forces that determine health.
Attention to the personal is based on the notion that critical self-awareness enhances our abilities to examine and act upon harmful social structures. It is a foundational component of a “revolutionary praxis of the body,” as it explicitly invites learners to utilize their senses and their personal subjective experiences of oppression and advantage to reflect upon the (re)production of social forces.35 Rather than merely reflecting on words in a text or theories that explicate the interlocking systems of oppression, we invite learners to share their lived experiences and center them in their analysis and in relationship-building with others in the learning space. The course thus integrates critical reflection upon personal and collective experiences operating within interlocking systems of oppression, such as racism, classism, ableism, and heteropatriarchy. Of note, pedagogy, even when critical, can and does reproduce harm if extreme care is not taken to attend to “power-over” dynamics that unfold in classrooms composed of learners from the Global South and Global North.36 As facilitators, attentiveness to the unintentional reproduction of patterns of harm is critical for creating safe learning spaces that potentiate the emergence of new forms of relationship based on mutuality, care, dialogue, and trust.
Finally, the value of partnership is foundational. Our understanding is that authentic partnerships across differences must be thoughtfully co-created and nourished in order to advance equity and approximate social justice. Too often, classrooms and educational processes replicate power dynamics already apparent in society, as those advantaged with social privilege and power “outside of the classroom walls” are given more opportunity to amplify their ideas and theories and make consequential decisions—praxis—than those from marginalized communities. In the context of global human rights education, a significant dichotomy is often amplified between those from the Global North and those from the Global South; and between those perceived as donors versus those perceived as recipients of assistance. Thus, our pedagogical approach is one that continually seeks opportunities for learners to build authentic relationships with one another—relationships that may, with time, evolve into generative partnerships. In the transnational reflection space, learners are invited to share what they witness locally, and then dialogue with a cadre of global learners about differences and similarities across the geographic spaces.
Discussion: A vision for dialogue through transformative pedagogy
While many potential spheres exist to spark interdisciplinary conversation between social medicine, collective health, and structural competency, we, given our position as educators grounded in critical pedagogy, envision one possible path through transformative pedagogy. As discussed above, transformative pedagogy creates a dynamic space that allows for ideas to intersect in a generative manner. When doing so with care, we believe that learners, faculty, and ideas all emerge changed and in deeper relationship. We believe that the same could occur for these three disciplines by intentionally bringing them into a space together and around the proverbial table for conversation.
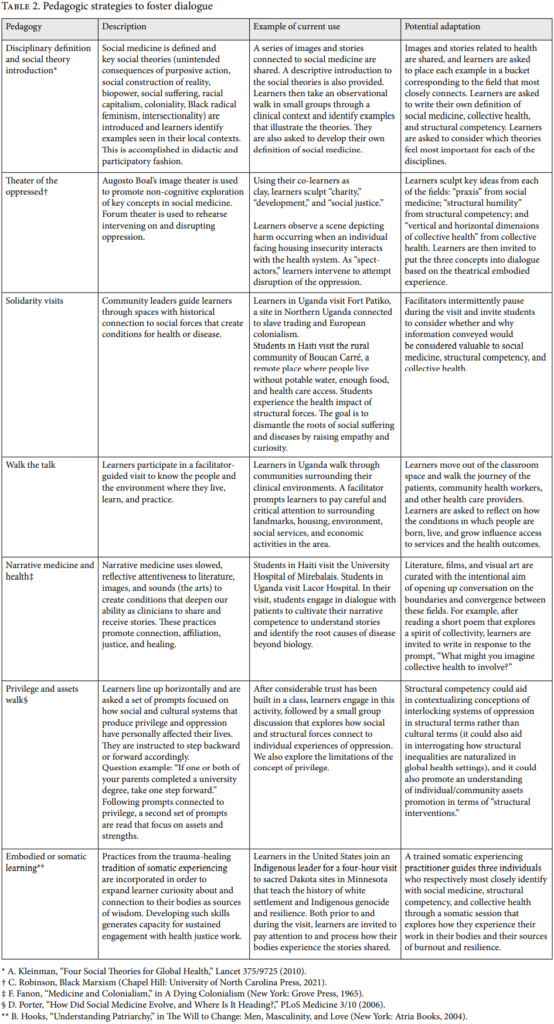
Fostering such dialogue will require deliberate adaptation of pedagogical tools currently used in our learning environments. Based on our humbling past experiences, we urge educators to deliberately anticipate and continually monitor for unintentional harm that arises among learning communities with diverse identities. This is especially true when adapting or trialing new pedagogies, such as those suggested below. In Table 2, we identify key pedagogies currently used in EqualHealth’s curricula and potential adaptations that aim to foster interdisciplinary dialogue.
Social medicine, collective health, and structural competency are interrelated, interdisciplinary, and evolving fields that have recursively grappled with health inequities in their unique histories against increasingly globalized oppressive phenomena impacting historically marginalized and dispossessed communities. There lies an opportunity within global health equity as a social change project to develop a common language and integrated framework for analysis within our fields toward more concrete and collaborative learner outcomes in order to better realize the human right to health. Particularly, we highlight a complementary strength from each of these fields. Among other fields of study dedicated to advancing the agenda of health and human rights, social medicine, collective health, and structural competency are uniquely positioned to provide foundational frameworks, content, and methods of global health equity analysis and action. Social medicine’s praxis—theory and action—both informs and takes inspiration from collective social change efforts. Collective health has proposed a “democratized” practice arena composed of horizontal and vertical levels of knowledge and practice contextualized within an active process of social determination. Structural competency has proposed structural humility such that structural interventions can be adapted to diverse contexts across various ecological levels, from micro to macro scales.
As critical and transformative pedagogy-oriented educators and advocates, we identify these three strengths as logical extensions to an equitable human rights education—one that focuses on a social change framework prioritizing personal empowerment, fostering and enhancing leadership, and development of alliances and coalitions.37 Experts in human rights education have proposed that programming take on an interactive pedagogical approach and have proposed idealized typologies for such programming.38
The three identified strengths from social medicine, collective health, and structural competency together have the potential to spur us to advance the agenda of health and human rights in a more cohesive framework that centers reflexivity, inclusivity, and relational solidarity across diverse historical and geographic contexts. If we are to advance a model of praxis geared toward social justice in global health, then an equity-oriented education and advocacy approach that is rooted in structural humility serves that end. More recently, Felisa Tibbitts has proposed a revised model of human rights education that points to the importance of integrating a reflective and critical stance.39 This model emphasizes attention to one’s own value system, power structures in the immediate and more distant environments, and the human rights framework. In line with Tibbitts, we contend that creating standards and values that uphold health and human rights requires a genuine and honest dialogue that engages, challenges, and questions the learners’ worldviews. Tibbitts identifies critical pedagogy as a philosophical “mother” to human rights education that can help “reflect upon, critique, and improve our efforts” in navigating tensions within human rights education as an endeavor mired by controversializing claims such as honoring indigeneity, examining conceptions of universality, and working with hierarchical structures of bureaucracy across private and public spheres. We propose that the lens of transformative pedagogies might be one such productive forum from which to promote further dialogue and offer suggestions. Our educational model rooted within social medicine and within our own principles of the 3Ps—praxis, personal, and partnership—has enabled us to recognize and understand the commonalities across and strengths of each of the three fields: social medicine, collective health, and structural competency. Our proposal for dialogue is not synonymous with a call to collapse or subsume these diverse fields into a standardized or universal framework, but rather to promote generative discussion at the intersection of their unique historical settings and their shared vision of promoting global health equity through interdisciplinary collaboration.
Limitations of this proposed dialogue as envisioned might include a relatively distanced interface with epistemologically different frameworks aligned with more “biotechnical” or “technocratic” formulations of global health structures, such as health systems strengthening, health systems administration and finance, global health security, and global health policy and research. Future directions of the proposed dialogue might interrogate how we can promote more coherent ethics across these different fields and local-global settings, as well as how we can design, translate, and evaluate social and structural interventions from educational settings to research and practice settings.
Conclusion
Calls from the field of global health to “decolonize” have been met with a suggestion to promote “dialogical reflexivity” with the aim of decentering Western epistemologies and further learning from Indigenous practices and worldviews of seeing the “whole person (physical, emotional, spiritual, and intellectual) in relationship with other individuals, communities, nations, and the world, guided by values of respect, reciprocity, relevance and responsibility” (note: this proposal for reflexivity diverges from its usual place within qualitative research and is brought closer to individual positionality).40 “Dialogical reflexivity,” similar in overarching principles to our model of the 3Ps, has been framed as comprising elements of “self-understanding, dialogue with peers, and insights-to-action.”41 We join with colleagues in calling for the building of a culture of dialogical reflexivity within the global health community. We thus offer our educational model of the 3Ps, as well as examples of collaborative transformative pedagogies, as a way of raising critical consciousness around oppressive forces. Promoting global health justice requires that we employ tools that aim to deconstruct forces that threaten human dignity with the goal of ensuring health as a human right for all.
Luis Martin Ortega, MD is a family physician at San Ysidro Health in San Ysidro, United States.
Michael J. Westerhaus, MD, MA is a primary care physician at the Center for International Health in Saint Paul, United States.
Amy Finnegan, PhD, MALD, is a professor of justice and peace studies at the University of Saint Thomas in Saint Paul, United States.
Aarti Bhatt, MD, is a medicine-pediatrics physician at the Community-University Health Care Center in Minneapolis, United States.
Alex Olirus Owilli, RN, BScN, MN, is a PhD candidate at the College of Nursing of the University of Saskatchewan in Saskatoon, Canada.
Brian Turigye, MBBS, MPH, is a medical officer at Divine Mercy Hospital in Mbarara, Uganda.
Youri Encelotti Louis, MD, is a generalist physician and care coordinator with Dialogue in Montreal, Quebec, Canada.
Please address correspondence to Luis Ortega. Email: orteg029@umn.edu.
Competing interests: None declared.
Copyright © 2023 Ortega, Westerhaus, Finnegan, Bhatt, Owilli, Turigye, and Louis. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- COVID-19 Hasn’t Slowed Global Warming: Earth’s Carbon Dioxide Levels Highest in Over 3 Million Years, NOAA Says,” USA Today (April 7, 2021), http://www.usatoday.com/story/news/nation/2021/04/07/global-warming-carbon-dioxide-levels-highest-3-m-years/7130141002/.
- Oxfam, “Pandemic Creates New Billionaire Every 30 Hours—Now a Million People Could Fall into Extreme Poverty at Same Rate in 2022” (May 2022), http://www.oxfam.org/en/press-releases/pandemic-creates-new-billionaire-every-30-hours-now-million-people-could-fall.
- T. Rogers, C. Rogers, E. VanSant-Webb, et al., “Racial Disparities in COVID-19 Mortality among Essential Workers in the United States,” World Medical and Health Policy 12/3 (2020).
- J. McKinlay, “A Case for Refocusing Upstream: The Political Economy of Illness,” Sociology of Health and Illness: Critical Perspectives (1994).
- H. Waitzkin, C. Iriart, A. Estrada, and S. Lamadrid, “Social Medicine Then and Now: Lessons from Latin America,” American Journal of Public Health 91/10 (2001); A. Osmo, L. Schraiber, “The Field of Collective Health: Definitions and Debates on Its Constitution,” Saúde e Sociedade 24/Suppl 1 (2015);N. Filho, J. Paim, “La crisis de la salud pública y el movimiento de la salud colectiva en Latinoamérica,” Cuadernos Médico Sociales 75 (1999); M. Harvey, J. Neff, K. R. Knight, et al., “Structural Competency and Global Health Education,” Global Public Health 17/3 (2022).
- H. Waitzkin, W. Alina Pérez, and M. Anderson, Social Medicine and the Coming Transformation (New York: Routledge, 2021).
- Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948), art. 25.
- D. Sun Han, S. Bae, D. Kim, and Y. Choi, “Origins and Evolution of Social Medicine and Contemporary Social Medicine in Korea,” Journal of Preventive Medicine and Public Health 50/3 (2017).
- Ibid., p. 142.
- J. Quadagno, One Nation, Uninsured: Why the U.S. Has No National Health Insurance (online edition: Oxford University Press, 2006).
- Waitzkin et al. (2001, see note 5), p. 1592.
- Ibid., pp. 1592, 1599
- P. Freire, Pedagogy of the Oppressed (New York: Continuum, 1970).
- Waitzkin et al. (2001, see note 5), p. 1598.
- A. Finnegan, M. Morse, M. Nadas, and M. Westerhaus, “Where We Fall Down: Tensions in Teaching Social Medicine and Global Health,” Annals of Global Health 83/2 (2017), p. 349.
- M. Harvey, C. Piñones-Rivera, and S. M. Holmes, “Thinking with and against the Social Determinants of Health: The Latin American Social Medicine (Collective Health) Critique from Jaime Breilh,” International Journal of Health Services 52/4 (2022); J. Breilh, Critical Epidemiology and the People’s Health (New York: Oxford University Press, 2021).
- J. Paim and N. de Almeida Filho, “Collective Health: A ‘New Public Health’ or Field Open to New Paradigms?,” Revista de Saúde Pública 32/4 (1998).
- A. Osmo and L. Schraiber, “The Field of Collective Health: Definitions and Debates on Its Constitution,” Saúde e Sociedade 24/Suppl 1 (2015).
- M. Pentecost, V. Adams, R. Baru, and C. Caduff, “Revitalising Global Social Medicine,” Lancet 398/10300 (2021).
- J. Metzl and H. Hansen, “Structural Competency: Theorizing a New Medical Engagement with Stigma and Inequality,” Social Science and Medicine 103 (2014).
- Harvey et al. (2022, see note 5), p. 342.
- Ibid., pp. 343–356.
- Ibid., p. 343.
- Ibid., p. 355.
- Ibid., p. 356.
- J. Mezirow and E. W. Taylor, Transformative Learning in Practice: Insights from Community, Workplace, and Higher Education (San Francisco: Jossey-Bass, 2009).
- P. Freire, Education, the Practice of Freedom (London: Writers and Readers Publishing Cooperative, 1976).
- Freire (1970, see note 13).
- A. Darder, “Freire and a Revolutionary Praxis of the Body,” Review of Education, Pedagogy, and Cultural Studies 40/5 (2018), p. 427.
- Ibid.
- Freire (1976, see note 27).
- A. Owilli, V. Voller, W. Martin, et al., “Beyond Witnesses: Moving Health Workers towards Analysis and Action on Social Determinants of Health,” World Medical and Health Policy 14/1 (2022); Finnegan et al. (see note 15); V. Voller, A. Owilli, A. Yang, et al., “Evaluating the Impact of a Social Medicine Course Delivered in a Local-Global Context: A 10-Year Multi-site Analysis,” World Medical and Health Policy 14/1 (2022).
- Owilli et al. (see note 31).
- Freire (1970, see note 13).
- P. Freire, Pedagogy of the City (New York: Continuum, 1993).
- Finnegan et al. (see note 15).
- F. Tibbitts, “Understanding What We Do: Emerging Models for Human Rights Education,” International Review of Education 48/3–4 (2002).
- Ibid.
- F. Tibbitts, “Revisiting ‘Emerging Models of Human Rights Education’,” International Journal of Human Rights Education 1/1 (2017).
- H. Liwanag and E. Rhule, “Dialogical Reflexivity towards Collective Action to Transform Global Health,” BMJ Global Health 6 (2021).
- L. Vieira da Silva, “Jules Guerin and Social Medicine in 1848,” Journal of Medical Biography 31/1 (2022).
