Volume 23/2, December 2021, pp. 49-61 | PDF
Leah Utyasheva and Lovleen Bhullar
Abstract
Pesticide exposure and poisoning among children can lead to devastating long-lasting health effects that impact their human rights, with communities in low- and middle-income countries experiencing the negative impacts of pesticides more profoundly than those in high-income countries. While United Nations agencies recommend banning highly hazardous pesticides responsible for serious pesticide poisonings, childhood pesticide poisoning is rarely discussed, especially from a human rights perspective. In India, a country with a large population of children and widespread pesticide use, no law or policy addresses pesticide poisoning among children. This lack of prioritization leads to gaps in poisoning surveillance and lack of government action to prevent poisoning, causing violations of children’s rights. The proposed pesticides ban can reduce pesticide poisoning among children in India, but to fully protect children’s rights, the government needs to establish comprehensive pesticide poisoning surveillance and ensure the mainstreaming of pesticide poisoning prevention into law and policy based on a human rights framework.
Introduction
If we take children’s rights to life and health seriously, the prevention of pesticide exposure and poisoning needs to become a global priority. Highly hazardous pesticides (HHPs)—pesticides that are acknowledged to present particularly high levels of acute or chronic hazards to health or the environment according to internationally accepted classification systems—are a global concern.[1] Organophosphates and carbamates and other HHPs belonging to class I and class II of the World Health Organization’s (WHO) classification of pesticides by hazard are the most common causes of pesticide poisoning.[2] The Food and Agriculture Organization (FAO) and WHO have repeatedly emphasized the need to reduce reliance on, the use of, and harms from HHPs, and the FAO has recognized children as one of the vulnerable groups for pesticide exposure.[3]
Children are affected by acute pesticide poisoning and chronic effects of exposure through ingestion, inhalation, and dermal contact.[4] They are more vulnerable than adults to the uptake and adverse effects of pesticides due to developmental, dietary, and physiological factors.[5] Pesticide poisoning in children may occur because of accidental exposure during play, occupational exposure during pesticide handling and agricultural work, and intentional self-harm (suicide or suicide attempt).[6] The environmental media of pesticide exposure and poisoning among children include air, water, and soil.[7] Pesticide exposure and poisoning is also experienced by plants and animals, leading to adverse impacts on plant and animal health.[8]
Pesticide exposure during pregnancy may impair the growth of the fetus and the healthy development of the child.[9] Chronic exposure and acute poisoning are associated with childhood cancers, neurodevelopmental issues, respiratory health issues, and low birth weight.[10] The United Nations Special Rapporteur on toxics and human rights has noted that “there is a ‘silent pandemic’ of disability and disease among children, associated with exposure to toxics and pollution during childhood, many of which do not manifest themselves for years or decades.”[11]
This paper uses a human rights lens to address this neglected issue of HHP exposure and poisoning in children, both globally and in India specifically. India is one of the world’s top producers, exporters, and users of pesticides.[12] It also has the largest child population in the world, with nearly 548 million children under the age of 18, representing almost 40% of its total population.[13] Moreover, 73% of all children live in rural areas, meaning that they face a high risk of exposure to pesticides in everyday life and sometimes use pesticides themselves. We assert that HHP exposure and poisoning puts children in a situation of vulnerability and represents a threat that requires special measures of protection.[14] Unfortunately, pesticide exposure and poisoning among children is reported in many other countries as well, making this paper’s findings relevant to other jurisdictions.[15]
The paper consists of four parts. Beginning with the context of pesticide exposure and poisoning among children globally and in India, the first part underlines the lack of data on the negative consequences of HHPs on children, and the need to eliminate HHPs from everyday use. The second part addresses the international human rights framework, and the third part analyzes how international obligations are reflected in India’s national legislation and policies. We conclude by highlighting the need to identify and ban HHPs and to include pesticide poisoning prevention in laws and policies in India and globally. While acknowledging the role of the pesticide industry in mitigating the harmful effects of HHP use, this paper concentrates on the state as the primary duty-bearer.
HHP exposure and poisoning as a human rights and equality issue
The vast majority of pesticide poisonings and deaths occur in low- and middle-income countries (LMICs) where pesticides are widely used in rural areas by small-holder farmers.[16] Since HHPs may be cheaper and are more easily available than the new generation of less toxic pesticides, LMICs use more HHPs than high-income countries, which have banned the domestic use of many HHPs but still manufacture and export them to other countries.[17] For example, in 2015, 59% of all pesticide sales in India were of HHPs, in contrast with 11% in the UK.[18]
HHP poisoning is a common hazard for many in LMICs, where people may lack information about the adverse effects of pesticide use and where poisoning treatment services may be scarce, difficult to access, and under-resourced.[19] Children belonging to low-income communities are particularly vulnerable to HHP poisoning and face multiple levels of impact and disadvantage due to their developing bodies, residence in rural areas with higher risk of exposure, and work with pesticides.[20]
The inverse relationship between exposure to pesticides and enjoyment of rights, particularly the rights of children, is recognized at the international level. The United Nations Special Rapporteur on the right to food has noted that
hazardous pesticides impose substantial costs on governments and have catastrophic impacts on the environment, human health and society as a whole, implicating a number of human rights and putting certain groups at elevated risk of rights abuses… Among those at grave risk of becoming victims of HHPs are agricultural workers, children, and low income and minority communities, especially in developing countries.[21]
The Committee on the Rights of the Child has expressed concern over the use of pesticides in state parties and their impact on children.[22] It has recommended that states prohibit the importation and use of any pesticides or chemicals whose use has been banned or restricted in exporting countries.[23]
HHP poisoning among children
Global systematic data on harms associated with pesticide poisoning in children are limited. Poisoning is reported as injuries, with accidental poisoning reported separately from intentional self-harm. According to WHO’s injury estimates from 2004 (the most recent year for which data are available), 345,814 people died worldwide that year because of accidental poisoning, with 13% of such poisonings occurring among people under 20.[24] Intentional pesticide poisoning, responsible for at least 20% of all suicide deaths in LMICs, was a common cause of death in older children.[25] WHO notes that there is substantial under-recording and under-reporting of childhood poisoning incidents.[26]
In India, data on pesticide poisoning among children are fragmented. Several agencies are responsible for data collection, but coordination on surveillance and data analysis is lacking.[27] In 2017, “injury, poisoning and certain other externalities” made up the third leading cause of deaths for children aged 5–14 (10.1% of all deaths) and was the leading cause of death for children aged 15–24 (20.5% of all deaths).[28] Similar to global data, India’s data are not disaggregated by cause of poisoning generally or among children specifically. Wolfgang Boedeker et al. place non-intentional pesticide poisoning in India in the range of 145 million people between 2006 and 2018, but specific data related to children are unavailable.[29]
Hospital studies find that HHP poisoning is the second to third most common cause of childhood poisoning, with cases of pesticide poisoning increasing over time.[30] Accidental poisoning is more common among younger children, while deliberate self-harm is more common among adolescents.[31] According to a 2013 study, children under the age of one had the highest rates of fatal accidental poisoning, with mortality decreasing with age until 14 years, after which it increased again due to self-harm.[32]
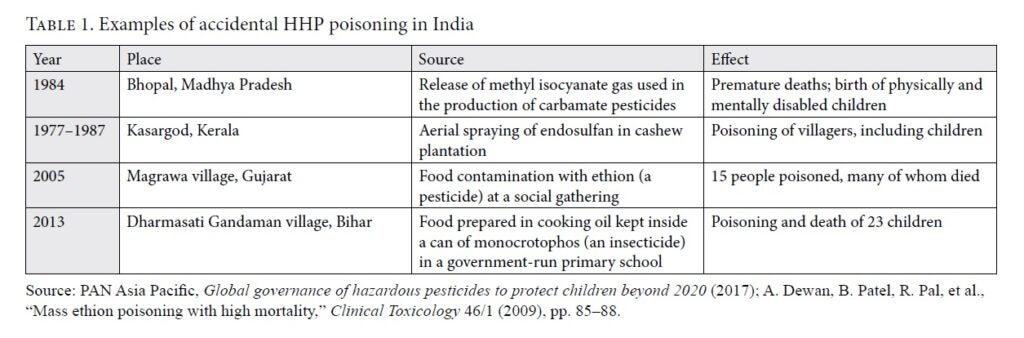
At least 10.1 million children participate in the workforce in India, of whom about 70% are involved in agriculture and related sectors, where they face higher risks of pesticide exposure and poisoning.[33] Several accidental pesticide poisoning cases also highlight the serious effect of wide pesticide use on children and the need for prevention (see Table 1).[34]
Elimination of HHPs: The most effective way to save health and the environment
The most effective way to prevent exposure and poisoning is the elimination of hazards.[35] Figure 1 depicts the hierarchy of hazard controls.
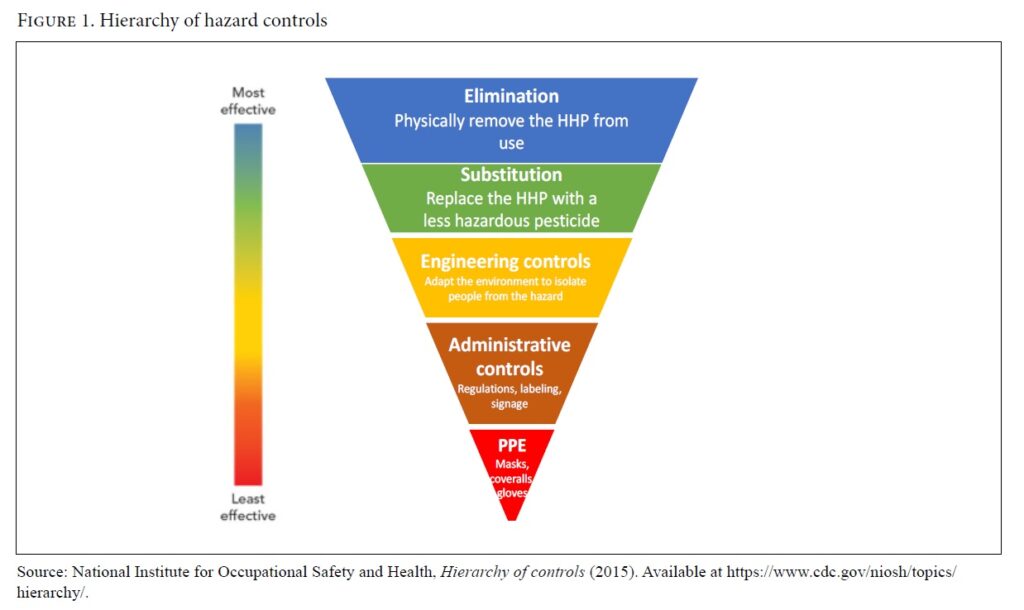
The elimination and substitution of hazards, such as through a ban on HHPs, is the most effective way to prevent pesticide exposure and poisoning. Other risk mitigation measures include (in order of effectiveness) engineering controls, administrative controls, and the use of personal protective equipment (PPE). Studies show that engineering and administrative control measures (label instructions and the safer storage of HHPs) and PPE use have not proven effective in LMICs.[36] Farmers may not be able to read or understand label instructions; PPE may be expensive, unavailable, or not feasible to use in hot climates; and the safer storage of HHPs is not effective for poisoning prevention.[37]
International regulations on pesticide management have a limited role in HHP exposure and poisoning prevention because of their information-sharing- and consensus-based approaches.[38] In contrast, national bans on HHPs have been effective in preventing pesticide poisoning and deaths.[39] HHP bans have led to significant reductions in deaths from intentional and unintentional poisoning in Sri Lanka, South Korea, and Bangladesh.[40] For example, Sri Lanka’s pesticide suicide prevention policy—which combines pesticide legislation, a suicide prevention strategy, and a high-level task force—has led to a notable decrease in poisoning and deaths.[41] The bans are accompanied by a data-driven approach that contributes to improvements in poisoning surveillance—an important component of a comprehensive response.[42]
More generally, HHP bans illustrate the application of the precautionary principle in the face of scientific uncertainty about the adverse impacts of HHPs.[43] In addition, national pesticide legislation should encourage the minimization of HHP use through stricter rules for risk assessment during pesticide registration (also applying the precautionary principle), the elimination of financial and other incentives, and the prohibition of export of domestically banned pesticides and import limitations.
International law on pesticide exposure and poisoning among children
Human rights are universal and indivisible, and while HHP exposure and poisoning have a particularly ruinous impact on children’s rights to life and health, a whole range of rights is affected. We will address other rights through the prism of the rights to life and health.
The right to life
Article 3 of the Universal Declaration of Human Rights, article 6 of the International Covenant on Civil and Political Rights (ICCPR), and article 6 of the Convention on the Rights of the Child (CRC) guarantee the right to life.[44] The ICCPR stipulates that every child shall have the right to special measures of protection as required by their status as a minor.[45] General Comment 36, which helps states implement the ICCPR’s provision on the right to life, requires states to adopt appropriate measures to protect life from all reasonably foreseeable threats and to take special positive measures of protection toward persons in situations of vulnerability or whose lives have been placed at risk because of specific threats.[46]
A child’s right to life is violated when easy access to HHPs puts their life in danger due to accidental or intentional pesticide poisoning. States’ obligation to protect children’s right to life includes creating an environment that ensures, to the maximum extent possible, the survival and healthy development of the child. States need to identify risks that underlie life, survival, growth, and development of the child, and design and implement evidence-informed interventions to protect the right to life.[47]
The right to health
The right to health derives from article 25 of the Universal Declaration of Human Rights, article 24 of the CRC, and article 12 of the International Covenant on Economic, Social and Cultural Rights.[48] Children’s right to health is an inclusive right extending to timely and appropriate prevention and health promotion, a right to grow and develop to one’s full potential, and a right to live in conditions that enable them to attain the highest standard of health.[49] It includes the underlying determinants of health, such as access to safe and potable water; an adequate supply of safe food, nutrition, and housing; healthy occupational and environmental conditions; and access to health-related education and information.[50] Children are entitled to the prevention of diseases and accidents as one aspect of health services.[51] HHP exposure and poisoning represent states’ failure to prevent injury and disease and to discharge their obligation to protect children’s right to health.[52] The realization of mothers’ right to health and their protection from pesticides, as underlined by the Committee on the Elimination of Discrimination against Women (the expert body that monitors the implementation of the Convention on the Elimination of all Forms of Discrimination against Women), is also crucial for the protection of children’s right to health.[53]
The availability of information about risks associated with HHPs is important for the protection of the right to health.[54] Most small-holder farmers and their families in LMICs possess little information about toxicity, correct application, and hazards associated with pesticide use. The right to health is threatened when health-related information about pesticide harms is unavailable, inaccessible, or hard to understand.[55]
Healthy occupational conditions are one of the underlying determinants of health. Occupational exposure to pesticides infringes on children’s right to health, which requires that children “be protected from performing any work that is likely to be hazardous … or to be harmful to [their] health or physical, mental, spiritual, moral or social development.”[56] The International Labour Organization does not allow children under 18 to be employed in hazardous work, including pesticide use.[57] In 2020, the Food and Agriculture Organization adopted the Framework on Ending Child Labour in Agriculture, calling for a renewed commitment to ending child labor and children’s exposure to pesticides.[58]
Three of the four overarching principles identified by the Committee on the Rights of the Child as fundamental principles guiding the implementation of the CRC are directly applicable here. The best interest of the child (article 3(1)), the inherent right to life (article 6), and the right to nondiscrimination (article 2) suggest the development of a rights-based approach to secure the holistic physical, psychological, moral, and spiritual integrity of the child, to promote their human dignity, and to ensure to the maximum extent possible their survival and development. The best interest of the child in attaining the right to health requires the prevention of HHP exposure and poisoning, as adverse health effects are often irreversible and may not manifest themselves for years.[59] These principles need to guide all laws and policies in order for states to fully realize children’s rights.[60]
The rights of the child and India’s domestic legal and policy framework
India’s domestic legal and policy framework recognizes children’s rights to life and health and the corresponding duties of the state. However, this framework does not consider the link between pesticide exposure and poisoning, on the one hand, and children’s rights, on the other.
The right to life
Children are among the holders of the fundamental right to life entrenched in article 21 of the Constitution of India. The Supreme Court has expanded the scope of this right to life beyond “protection of limb or faculty” to include “the right to live with human dignity and all that goes along with it, namely, the bare necessaries of life.”[61] A person’s right to life is “secured only when he is assured of all facilities to develop himself and is freed from restrictions which inhibit his growth.”[62] The right embraces “quality of life,” which is described as “all those aspects of life which go to make a man’s life meaningful, complete and worth living.”[63] The Supreme Court cited article 21 of the Constitution when passing an order to ban the use, sale, production, and export of endosulfan (a DDT-like organochloride insecticide), applying the precautionary principle.[64]
As discussed above, pesticide exposure and poisoning may result in the loss of life or in long-term health and developmental impacts. A child who is affected by exposure or poisoning may exist physically but be unable to enjoy the right to live with dignity or enjoy quality of life. In other words, their constitutional right to life is violated, and it is the duty of the state to prevent pesticide exposure and poisoning, such as through the introduction and implementation of appropriate measures.
The right to health
While India’s Constitution does not explicitly guarantee a right to health, the Supreme Court has read this right into the constitutional right to life and defined it as the “right to live in a clean, hygienic and safe environment.”[65] The Constitution also includes Directive Principles of State Policy, which, though non-enforceable, are “fundamental in the governance of the country” and shall be applied by the state in making laws. Two of these principles address children’s health: article 47 establishes a state duty to improve public health, while article 39(e)–(f) notes that the state shall direct its policy toward ensuring that the tender age of children is not abused and that children are given opportunities and facilities to develop in a healthy manner. HHP exposure and poisoning undermine the realization of children’s constitutional right to health and represent the state’s failure to discharge its constitutional duties.
Health falls within the purview of state governments.[66] Gujarat is one of the few states that has enacted a health law with an explicitly rights-based approach.[67] The law’s preamble recognizes the importance of fundamental human rights and of improving the quality of life of all citizens. Chapter V explicitly incorporates the rights to health and dignity, which could ensure protection from pesticide exposure and poisoning. In the state of Goa, the Children’s Act of 2003 explicitly recognizes children’s rights and sets out the duty of the state government to ensure that children are given opportunities and facilities to develop in a healthy manner and in conditions of freedom and dignity.[68] The CRC’s provisions on the rights of the child are directly enforceable subject to certain exceptions, and state governments are permitted to specify higher standards for children. These provisions represent opportunities to protect children from pesticide exposure and poisoning.
The right to health and the prohibition of child labor
Article 23 of the Constitution prohibits forced labor. The system of forced and partly forced labor was abolished in 1976 and is today a punishable offense.[69] However, adults and children continue to be forced to work on farms where pesticide use might lead to exposure and poisoning.[70] Article 24 of the Constitution prohibits the employment of children in hazardous work. According to the Child and Adolescent Labour (Prohibition and Regulation) Act, the employment of children under 14 in any occupation or process, and of adolescents aged 14–18 in specified hazardous processes, is prohibited.[71] These hazardous processes include insecticides, fungicides, and herbicides, among others.[72] By referring to the potential of hazardous processes to cause material impairment to workers’ health, the law implicitly acknowledges the right to health of workers who are children. At the same time, the law permits a child to help their family in a family enterprise subject to certain conditions.[73] Children may work on farms where pesticides are used, thus risking pesticide exposure and poisoning. The continuance of child labor after the enactment of relevant laws and the absence of measures to prevent HHP exposure and poisoning of children represent the state’s failure to discharge its duties corresponding to children’s right to health. The elimination of child labor is a complex issue that impacts the entire range of children’s rights and requires comprehensive approaches that are beyond the scope of this paper.
Children’s rights and pesticide use in panchayat laws
The main use of pesticides in India is in agriculture. The extensive network of panchayats—self-governing institutions for rural areas—could play a role in the protection of children from pesticides exposure and poisoning.[74] A 2005 World Bank report recognizes the need to enhance the regulatory role of gram panchayats for the controlled use of pesticides.[75] In Kerala, a license is required for the use of any place in the panchayat area for purposes that are likely to be offensive or dangerous to human life or health, including storing, preparing, packing, and selling pesticides.[76] There is implicit recognition of the adverse impacts of pesticides on the rights to life and health. In Andhra Pradesh and Telangana, the panchayat secretary (a non-elected representative appointed by the state government to oversee panchayat activities) is required to assist in giving information to concerned officials about black-market sales of pesticides.[77] Elimination of the black market is necessary for the successful enforcement of pesticide management rules, which in turn enhances protection of the abovementioned rights.
National policies and children’s rights
Children’s rights form the exclusive focus of many national policies.[78] The National Policy for Children of 2013 explicitly affirms the government’s commitment to a rights-based approach.[79] In addition, the National Youth Policy of 2014 recognizes health as a priority and highlights the need for a targeted approach to emotional and mental health issues. Since there is a clear link between the incidence of intentional pesticide poisoning among youth and their emotional and mental health issues, implementation of this policy could include measures directed at the prevention of intentional poisoning. Further, children are the beneficiaries of several other policies, including the National Health Policy of 2017, the National Population Policy of 2000, and the National Education Policy of 2020. These policies could provide the overarching framework for the incorporation and realization of children’s rights and the integration of pesticide exposure and poisoning prevention in regulatory instruments.
Prevention of HHP exposure and poisoning among children: The way forward
India is currently discussing a new pesticide management law to replace the Insecticides Act of 1968. The Union Cabinet approved the Pesticide Management Bill in February 2020, and it was introduced in the Rajya Sabha (the upper house) the following month.[80] The bill includes several features to decrease HHP use and exposure, including requirements for pesticide labels, the promotion of organic pesticides, and prescription requirements for the sale of class I pesticides. States have the power to organize and carry out poisoning surveillance.[81]
The objective of the bill is “to regulate pesticides … to ensure availability of safe and effective pesticides and to strive to minimize risk to human beings, animals, living organisms other than pests, and the environment.” However, the use of terms such as “to strive to” creates a hierarchy among objectives. The bill follows the traditional command-and-control approach—for example, by subjecting the registration of pesticides to the fulfillment of certain formal criteria instead of mitigating and eliminating negative health effects by decreasing pesticide use and introducing bans on HHPs. Further, it does not ban HHPs that are harmful to health, nor does it prohibit the registration of pesticides banned in other countries.[82]
The bill follows in the steps of India’s ban on 12 pesticides in 2018 and the proposal to ban 27 other pesticides in 2020.[83] Some stakeholders opposed these bans on the ground that they may decrease agricultural productivity, endanger food security, increase farmers’ production costs, and adversely impact the profitability of the pesticide industry.[84] The bill, together with the proposed pesticide ban, if adopted, can form a part of the country’s response to HHP exposure and poisoning among children. However, to be effective, these solutions must be accompanied by the introduction of HHP poisoning prevention measures in laws and policies on children, women, health, agriculture, and labor.
As illustrated above, the failure of regulatory instruments to protect children from HHP exposure and poisoning happens due to weak surveillance systems, a lack of government prioritization and coordination of response measures, and the government’s hesitation to ban HHPs. First, although childhood mortality and morbidity are discussed widely, data on the health effects of pesticides on children remain lacking.[85] A pesticide incidence surveillance system is necessary to convince decision-makers of the seriousness of the situation. Second, currently, the issue of pesticide exposure and poisoning among children in India sits at the periphery of concern for different central government ministries, such as the Ministry of Health and Family Welfare, Ministry of Women and Child Development, Ministry of Agriculture and Farmers’ Welfare, Ministry of Labour and Employment, and Ministry of Human Resources Development. A similar situation exists at the state level. This fragmentation must be replaced by a comprehensive and integrated approach, which would also promote the implementation of existing laws and policies that emanate from government agencies with different mandates.
Third, the belief that pesticide use is necessary for food security and agricultural productivity is a misconception. The Special Rapporteur on the right to food has underlined that “the assertion by the agrochemical industry that pesticides are necessary to achieve food security is not only inaccurate, but dangerously misleading.”[86] Replacing chemicals with biological plant protection products and promoting agricultural practices that stimulate soil fertility are more beneficial for sustainable food production than indiscriminate pesticide use.[87]
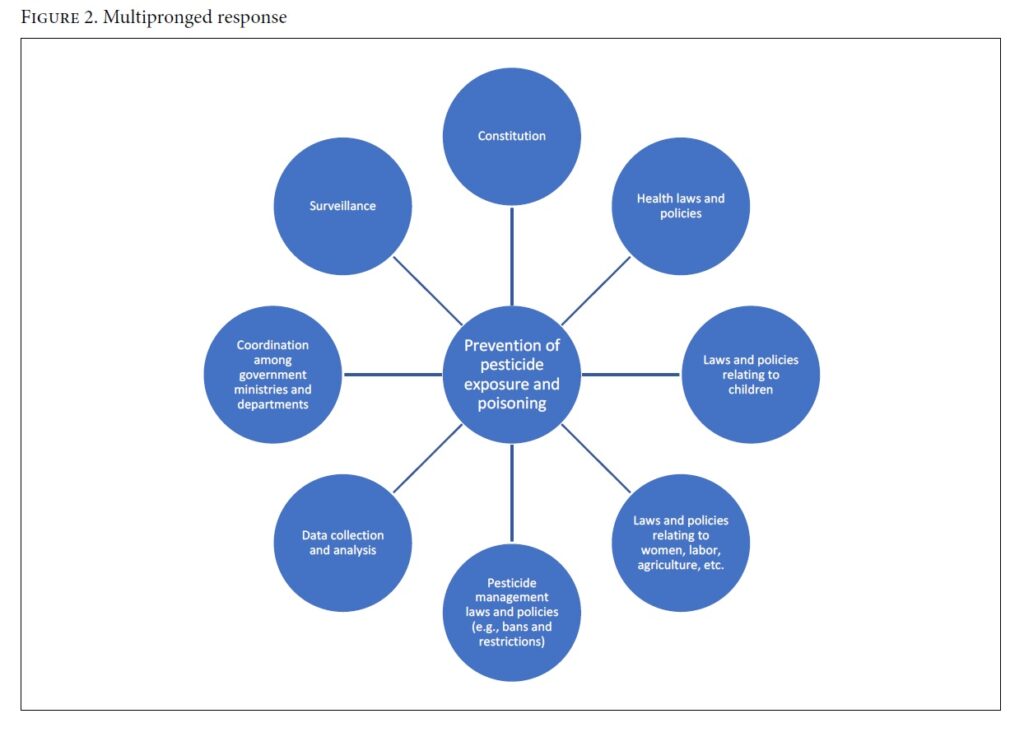
The wide availability and use of HHPs and their impact on children’s rights deserve urgent recognition and attention from international and national decision-makers. Our discussion of India’s legal and policy framework highlights the complexities and intricacies of developing responsive and child-centered laws and policies. Our review identifies elements of the domestic framework that could form a part of a multipronged response (Figure 2) to pesticide exposure and poisoning among children. Nationally in India and globally, HHP bans can save the lives and health of the present and future generations and positively impact animal health and the environment. As highlighted in this paper, policy coordination and prioritization, as well as information about best practices, are needed to formulate effective responses.
Conclusion
The universality and indivisibility of children’s rights are particularly relevant for pesticide poisoning prevention, as children’s rights to life and health provide the rationale for stricter pesticide regulation and, ultimately, the phasing out of HHPs. The principle of the best interest of the child points to the need to adopt a human rights-based and child-centered approach to the development and implementation of pesticide management laws and policies. Collaboration among the industry, international bodies, and national decision-makers on strengthening pesticide management is needed to promote a children’s rights-based approach. The human rights-based framework discussed in this paper could ensure the integration of the interests of children into relevant domestic laws and policies in different jurisdictions.
Acknowledgments
We would like to thank Professor Michael Eddleston of the University of Edinburgh and Professor Philippe Cullet of SOAS University of London for reviewing this paper.
Leah Utyasheva is a policy director at the Centre for Pesticide Suicide Prevention, University of Edinburgh, UK.
Lovleen Bhullar is a lecturer at Birmingham Law School, University of Birmingham, UK.
Please address correspondence to Leah Utyasheva. Email: lutyashe@ed.ac.uk.
Competing interests: None declared.
Copyright © 2021 Utyasheva and Bhullar. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
[1] Food and Agriculture Organization and World Health Organization, Guidelines on highly hazardous pesticides (2016); J. G. Thundiyil, J. Stober, N. Besbelli, et al., “Acute pesticide poisoning: A proposed classification tool,” Bulletin of the World Health Organization 86/3 (2008), pp. 205–209.
[2] J. Pretty, The pesticide detox: Towards a more sustainable agriculture (2005); European Union, The use of pesticides in developing countries and their impact on health and the right to food, EP/EXPO/DEVE/FWC/2019-01/LOT3/R/; PE653.622 (2001).
[3] Food and Agriculture Organization and World Health Organization, International code of conduct on pesticide management: Guidelines on highly hazardous pesticides (Rome: FAO, 2016); World Health Organization, Public health effects of chemicals: Knowns and unknowns (Geneva: WHO, 2016).
[4] Food and Agriculture Organization and World Health Organization, Detoxifying agriculture and health from highly hazardous pesticides: A call for action (Rome: FAO and WHO, 2019); World Health Organization, Exposure to Highly Hazardous Pesticides: A major public health concern, WHO/CED/PHE/EPE/19.4.6 (2019); UNICEF, Understanding the impacts of pesticides on children: A discussion paper (January 2018); J. R. Roberts, C. J. Karr, and Council on Environmental Health, “Pesticide exposure in children,” Pediatrics 130/6 (2012), pp. 1765–1788.
[5] UNEP Chemicals, Childhood pesticide poisoning: Information for advocacy and action (May 2004).
[6] M. Watts, Poisoning our future: Children and pesticides (Penang: Pesticide Action Network Asia and the Pacific, 2013).
[7] See, for example, Md. W. Aktar, D. Sengupta, and A. Chowdhury, “Impact of pesticides use in agriculture: Their benefits and hazards,” Interdisciplinary Toxicology 2/1 (2009), pp. 1–12.
[8] Ibid. See also P. C. Jepson, “Assessing environmental risks of pesticides,” in E. B. Radcliffe, W. D. Hutchinson, and R. E. Cancelado (eds), Integrated pest management: Concepts, strategies, tactics and case studies (Cambridge: Cambridge University Press, 2009), pp. 205–220.
[9] L. M Jaacks, N. Diao, A. M. Calafat, et al., “Association of prenatal pesticide exposures with adverse pregnancy outcomes and stunting in rural Bangladesh,” Environment International 133 (2019).
[10] M. Peden, K. Oyegbite, J. Ozanne-Smith, et al., World report on child injury prevention (Geneva: WHO Press, 2008); S. H. Reuben, Reducing environmental cancer risk: What we can do now; President’s Cancer Panel 2008–2009 annual report (Bethesda: US Department of Health and Human Services, 2010); S. A. Widyawati, S. Suhartono, M. Mexitalia, et al., “The relationships between pesticide exposure and umbilical serum IGF-1 levels and low-birth weight: A case-control study in Brebes, Indonesia,” International Journal of Occupational and Environmental Medicine 11/1 (2020), pp. 15–23; A. M. Mora, J. A. Hoppin, L. Cordoba, et al., “Prenatal pesticide exposure and respiratory health outcomes in the first year of life: Results from the Infants’ Environmental Health (ISA) study,” International Journal of Hygiene and Environmental Health 225 (2020).
[11] Human Rights Council, Report of the Special Rapporteur on the Implications for Human Rights of the Environmentally Sound Management and Disposal of Hazardous Substances and Wastes, UN Doc. A/HRC/33/41 (2016).
[12] I. Devi, J. Thomas, and R. Raju, “Pesticide consumption in India: A spatiotemporal analysis,” Agricultural Economics Research Review 30 (2017), pp. 163–172; Top pesticide exporters. Available at http://www.worldstopexports.com/top-pesticides-exporters/.
[13] UNICEF, The state of the world’s children 2019: Statistical tables; Demographics. Available at https://data.unicef.org/resources/dataset/sowc-2019-statistical-tables/; G. Gururaj and M. S. Gautham, Advancing child safety in India: Implementation is the key (Bengaluru: National Institute of Mental Health and Neuro Sciences, 2019).
[14] L. Utyasheva and M. Eddleston, “Prevention of pesticide suicide and the right to life: The intersection of human rights and public health priorities,” Journal of Human Rights 20/1 (2021), pp. 52–71.
[15] M. Azemi, M. Berisha, S. Kolgeci, et al., “Frequency, etiology and several sociodemographic characteristics of acute poisoning in children treated in the intensive care unit,” Materia Socio-medica 24/2 (2012), pp. 76–80; A. Yimaer, G. Chen, M. Zhang, et al., “Childhood pesticide poisoning in Zhejiang, China: A retrospective analysis from 2006 to 2015,” BMC Public Health 17 (2017).
[16] D. Gunnell, D. Knipe, S-S. Chang, et al., “Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: A systematic review of the international evidence,” Lancet Global Health 5/10 (2017), pp. e1026–e1037.
[17] “Toxic exports: A Syngenta pesticide banned in Switzerland pollutes drinking water in Brazil,” Public Eye (January 9, 2020). Available at https://www.publiceye.ch/en/media-corner/press-releases/detail/toxic-exports-a-syngenta-pesticide-banned-in-switzerland-pollutes-drinking-water-in-brazil.
[18] Ibid.
[19] M. Eddleston and D. Gunnell, “Preventing suicide through pesticide regulation,” Lancet Psychiatry 7/1 (2020) pp. 9–11.
[20] D. Mohan, “Childhood injuries in India: Extent of the problem and strategies for control,” Indian Journal of Pediatrics 53/5 (1986), pp. 607–615; Roberts et al. (see note 4).
[21] Human Rights Council, Report of the Special Rapporteur on the Right to Food, UN Doc. A/HRC/34/48 (2017).
[22] Committee on the Rights of the Child, Concluding Observations: Haiti, UN Doc. CRC/C/HTI/CO/2-3 (2016), para. 53(d); Committee on the Rights of the Child, Concluding Observations: Argentina UN Doc. CRC/C/ARG/CO/5-6 (2018).
[23] Committee on the Rights of the Child, Concluding Observations: Mexico, UN Doc. CRC/C/MEX/CO/4-5 (2015), para. 51.
[24] Peden et al. (see note 10).
[25] Ibid.; Gunnell et al. (see note 16).
[26] Peden et al. (see note 10).
[27] J. Jagnoor, M. Ponnaiah, M. Varghese, et al., “Potential for establishing an injury surveillance system in India: A review of data sources and reporting systems,” BMC Public Health 20 (2020); Gururaj and Gautham (see note 13).
[28] Office of the Registrar General of India, Report on medical certification of cause of death 2017 (New Delhi: Ministry of Home Affairs, 2017).
[29] W. Boedeker, M. Watts, P. Clausing, et al., “The global distribution of acute unintentional pesticide poisoning: Estimations based on a systematic review,” BMC Public Health 20 (2020).
[30] M. Jayashree and S. Singhi, “Changing trends and predictors of outcome in patients with acute poisoning admitted to the intensive care,” Journal of Tropical Pediatrics 57/5 (2011), pp. 340–346; N. K. Bhat, M. Dhar, S. Ahmad, et al., “Profile of poisoning in children and adolescents at a North Indian tertiary care center,” Journal: Indian Academy of Clinical Medicine 13/1 (2013), pp. 37–42.
[31] A. Dutta, A. Seth, P. Goyal, et al., “Poisoning in children: Indian scenario,” Indian Journal of Pediatrics 65/3 (1998), pp. 365–370; A. Jose, S. Sivanandam, and J. Matthai, “Poisoning in children from an educationally and economically advanced urban area of South India,” Asian Journal of Epidemiology 5/4 (2012), pp. 123–129.
[32] B. Aggarwal, S. K. Rana, and N. Chhavi, “Pattern of poisoning in children: An experience from a teaching hospital in Northern India,” JK Science 16/4 (2014), pp. 174–178.
[33] G. S. Sanghera, Child labour in India: Globalization, power, and the politics of international children’s rights (New Delhi: Oxford University Press, 2016).
[34] See Pesticide Action Network Asia Pacific, Global governance of hazardous pesticides to protect children beyond 2020 (2017).
[35] P. Yip, E. Caine, S. Yousuf, et al., “Means restriction for suicide prevention,” Lancet 379/9834 (2012), pp. 2393–2399.
[36] Eddleston and Gunnell (see note 19); M. Pearson, C. Metcalfe, S. Jayamanne, et al., “Effectiveness of household lockable pesticide storage to reduce pesticide self-poisoning in rural Asia: A community-based, cluster-randomised controlled trial,” Lancet 390 (10105), pp. 1863–1872.
[37] Eddleston and Gunnell (see note 19); Pearson et al. (see note 36).
[38] Rotterdam Convention on the Prior Informed Consent Procedure for Certain Hazardous Chemicals and Pesticides in International Trade (1998); Stockholm Convention on Persistent Organic Pollutants (2001).
[39] Gunnell et al. (see note 16); T. Bonvoisin, L. Utyasheva, D. Knipe, et al., “Suicide by pesticide poisoning in India: A review of pesticide regulations and their impact on suicide trends,” BMC Public Health 20/1 (2020).
[40] D. Gunnell, M. Eddleston, M. R. Phillips, et al., “The global distribution of fatal pesticide self-poisoning: Systematic review,” BMC Public Health 7/1 (2007).
[41] D. Knipe, S-S. Chang, A. Dawson, et al., “Suicide prevention through means restriction: Impact of the 2008–2011 pesticide restrictions on suicide in Sri Lanka,” PLOS One 12/3 (2017).
[42] R. Dandona and D. Gunnell, “Pesticide surveillance and deaths by suicide,” Lancet Global Health 9/6 (2021), pp. e738–e739; M. Pearson, A. B. Zwi, N. A. Buckley, et al., “Policymaking ‘under the radar’: A case of pesticide regulation to prevent intentional poisoning in Sri Lanka,” Health Policy and Planning 30/1 (2015), pp. 56–67.
[43] A. D. D. Kumar and C. Jayakumar, “From precautionary principle to nationwide ban on endosulfan in India,” Business and Human Rights Journal 4/2 (2019), pp. 343–349.
[44] Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948); International Covenant on Civil and Political Rights, G.A. Res. 2200A (XXI) (1966); Convention on the Rights of the Child, G.A. Res. 44/25 (1989).
[45] International Covenant on Civil and Political Rights, G.A. Res. 2200A (XXI) (1966), art. 24.
[46] Human Rights Committee, General Comment No. 36 on Article 6 of the International Covenant on Civil and Political Rights, on the Right to Life, UN Doc. CCPR/C/GC/36 (2018).
[47] Committee on the Rights of the Child, General Comment No. 15: The Right of the Child to the Enjoyment of the Highest Attainable Standard of Health, UN Doc. CRC/C/GC/15 (2013), para. 16.
[48] International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966).
[49] Committee on the Rights of the Child (2013, see note 47), para. 2.
[50] Committee on Economic, Social and Cultural Rights, General Comment No. 14: The Right to the Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4 (2000).
[51] Ibid., para. 25.
[52] Human Rights Council (2016, see note 11).
[53] Committee on the Elimination of Discrimination against Women, General Recommendation No. 34 on the Rights of Rural Women, UN Doc. CEDAW/C/GC/34 (2016); Committee on the Rights of the Child (2013, see note 47), para. 18.
[54] F. Z. Ksentini, UN Special Rapporteur on Human Rights and the Environment, Final Report, UN Doc. E/CN.4/Sub.2/1994/9 (1994), pp. 204–206.
[55] H. A. Rother, “Pesticide labels: Protecting liability or health? Unpacking ‘misuse’ of pesticides,” Current Opinion in Environmental Science and Health 4 (2018), pp. 10–15.
[56] Convention on the Rights of the Child, G.A. Res. 44/25 (1989), art. 32.
[57] International Labour Organization, Minimum Age Convention, C138 (1973).
[58] Food and Agriculture Organization, FAO framework on ending child labour in agriculture (Rome: FAO, 2020).
[59] Human Rights Council (2016, see note 11), para. 46.
[60] Committee on the Rights of the Child, General Comment No. 12 (2009), The Right of the Child to Be Heard, UN Doc. CRC/C/GC/12 (2009); Committee on the Rights of the Child, General Comment No. 5, General Measures of Implementation of the Convention on the Rights of the Child, UN Doc. CRC/GC/2003/5 (2003); Committee on the Rights of the Child, General Comment No. 14 (2013) on the Right of the Child to Have His or Her Best Interests Taken as a Primary Consideration, UN Doc. CRC/C/GC/14 (2013).
[61] See Francis Coralie Mullin v. Administrator, Union Territory of Delhi and Others (1981), 1 S.C.C. 608, para. 7; State of Himachal Pradesh v. Umed Ram Sharma and Others (1986), 2 S.C.C. 68, para. 11.
[62] Chameli Singh and Others v. State of UP and Another (1996), 2 S.C.C. 549, para. 8.
[63] State of Himachal Pradesh (see note 61), para. 11; Dr Ashok v. Union of India and Others (1997), 5 S.C.C. 10, para. 4.
[64] Kumar and Jayakumar (see note 43).
[65] Occupational Health and Safety Association v. Union of India and Others (2014), 3 S.C.C. 547, para. 10.
[66] Constitution of India (1950), Seventh Schedule, List II (state list), item 6.
[67] Gujarat Public Health Act (2008).
[68] Goa Children’s Act (2003), Goa Act 18 of 2003 (July 8, 2003).
[69] Bonded Labour System (Abolition) Act (1976), Act No. 19 of 1976 (February 9, 1976).
[70] See Human Rights Watch, The small hands of slavery: Bonded child labour in India (1996). Available at https://www.hrw.org/reports/1996/India3.htm; Physicians for Human Rights Child Rights Group, “Child labour in India: A health and human rights perspective,” Lancet 362 (2003), pp. s32–s33.
[71] The Child and Adolescent Labour (Prohibition and Regulation) Act (1986), Act No. 61 of 1986 (December 23, 1986) (as amended).
[72] The Factories Act (1948), Act No. 63 of 1948 (September 23, 1948) (as amended), First Schedule.
[73] The Child and Adolescent Labour (Prohibition and Regulation) Amendment Rules (2017), GSR 543(E) (June 2, 2017).
[74] Constitution of India (1950), articles 243(d)–(g).
[75] Environmental Management and Policy Research Institute, Environmental guidelines for “Karnataka Panchayat Strengthening and Poverty Alleviation Project” (Bangalore: EMPRI, 2005).
[76] Kerala Panchayat Raj (Issue of Licence to Dangerous and Offensive Trades and Factories) Rules (1996), SRO No. 76/96 (January 18, 1996).
[77] Andhra Pradesh Panchayat Raj (Functions of Panchayat Secretary) Rules (2007), GOMs No. 199 (May 18, 2007); Telangana Panchayat Raj (Functions of Panchayat Secretary) Rules (2018), GO No. 108 (September 26, 2018).
[78] M. R. Mathur and S. Reddy, “Child health policies in India: Moving from a discernible past to a promising future,” Indian Journal of Pediatrics 86/6 (2019), pp. 520–522.
[79] National Policy for Children (2013), Resolution No. 16-1/2012-CW-1 (May 11, 2013).
[80] The Pesticide Management Bill (2020), Bill No. XXII of 2020. Available at https://prsindia.org/files/bills_acts/bills_parliament/Pesticide-bill.pdf.
[81] Ibid.
[82] V. Kumar, “Pesticide Management Bill 2020 must address important concerns,” DownToEarth (February 14, 2020). Available at https://www.downtoearth.org.in/blog/agriculture/pesticide-management-bill-2020-must-address-important-concerns-69303.
[83] Pesticides (Prohibition) Order (2018), Notification S.O. 3951(E) (August 8, 2018). See also Banning of Insecticides Order (2020), Notification S.O. 1512(E) (May 14, 2020).
[84] P. Jebaraj, “Move to ban 27 pesticides opposed,” Hindu (June 10, 2020); PTI, “Industry body PMFAI opposes govt proposal to ban 27 pesticides fearing biz loss worth RS 6,000 crore,” New Indian Express (June 9, 2020).
[85] L. Liu, S. Oza, D. Hogan, et al., “Global, regional, and national causes of under-6 mortality in 2000-15: An updated systematic analysis with implications for the Sustainable Development Goals,” Lancet 388/10063 (2016), pp. 3027–3035; K. Rastogi, K. Goel, T. Jain, et al., “Evaluation of National Injury Surveillance Centre, India, 2015–2016,” Indian Journal of Community Health 32/1 (2020), pp. 51–56; Jagnoor et al. (see note 27).
[86] Human Rights Council (2016, see note 11).
[87] P. Birthal, O. Sharma, and S. Kumar, “Economics of integrated pest management: Evidences and issues,” Indian Journal of Agricultural Economics 55/4 (2000), pp. 644–659; S. Patil, P. Reidsma, P. Shah, et al., “Comparing conventional and organic agriculture in Karnataka, India: Where and when can organic farming be sustainable?,” Land Use Policy 37 (2014), pp. 40–51; ICAR-Agricultural Technology Application Research Institute, KVKs at farmers’ doorsteps for strengthening capabilities to combat whitefly epidemic in cotton,’ First Hand Report (ICAR: Ludhiana, n.d.).
