Volume 22/1, June 2020, pp 21 – 34
Petr Winkler, Lucie Kondrátová, Anna Kagstrom, Matěj Kučera, Tereza Palánová, Marie Salomonová, Petr Šturma, Zbyněk Roboch, and Melita Murko
Abstract
This study sought to evaluate the quality of care in Czech psychiatric hospitals and adherence to the Convention on the Rights of Persons with Disabilities (CRPD). Each psychiatric hospital was evaluated by a team comprising a service user, a psychiatrist, a social worker, a human rights lawyer, and a researcher, all trained in using the World Health Organization’s QualityRights Toolkit. We conducted content analysis on internal documents from psychiatric hospitals, observed everyday practices, and conducted 579 interviews across public psychiatric hospitals between 2017 and 2019. We found that none of the CRPD articles as assessed by the QualityRights Toolkit was fully adhered to in Czech psychiatric hospitals. We recommend both facility- and system-level interventions to improve CRPD adherence in the Czech context and in the wider region of Central and Eastern Europe. To achieve this, substantial investments are required.
Introduction
Psychiatric hospitals have been associated with violations of the human rights of service users all over the world.1 In many countries, this has triggered a deinstitutionalization of psychiatric services, which is understood as shifting the locus of care from psychiatric hospitals to care in the community.2 Deinstitutionalization began in the 1950s and has been successfully pursued in many countries worldwide, but not in the region of Central and Eastern Europe.3 Evidence from Scandinavia suggests that deinstitutionalization has led to both a decrease in suicide and a lower mortality gap between people with mental disorders and the general population.4
Mental health care systems in Central and Eastern Europe—despite a significant development of community services, increased participation of service users, and stronger emphasis on human rights over the last three decades—remain hospital based and inefficiently funded.5 The Strategy for Mental Health Care Reform published by the Ministry of Health of the Czech Republic places a strong emphasis on human rights and includes deinstitutionalization as a major aim for reform.6 The strategy has been translated into implementation projects funded by European structural and investment funds. One of these projects is entitled “Deinstitutionalization” and is focused on the transformation of Czech psychiatric hospitals. Increased adherence toward the human rights of people with mental health problems is one of the primary aims of this project.
The Convention on the Rights of People with Disabilities (CRPD) was adopted by the United Nations in 2006 to “promote, protect and ensure full and equal enjoyment of all human rights and fundamental freedoms by all persons with disabilities, and to promote respect for their inherent dignity.”7 The CRPD has introduced new challenges for mental health care legislation and practice, and it is now considered a milestone in safeguarding the human rights of people with mental health problems.8
In 2017, the World Health Organization (WHO) used its QualityRights Toolkit to evaluate adherence to the CRPD in selected European long-term residential institutions for people with psychosocial disabilities.9 We aimed to follow up on this initiative and assess adherence to the CRPD in all Czech psychiatric hospitals.
Methods
Participating psychiatric hospitals
The Institute of Health Information and Statistics of the Czech Republic registered a total of 21 psychiatric hospitals in the Czech Republic in 2017. Of those, three care specifically for children and adolescents, three are primarily for people addicted to alcohol and other substances, and one is for people with organic mental disorders. The remaining 15 psychiatric hospitals provide long-term care for various groups of people with mental illness, including long-term care (six months and longer) for adults with severe mental illnesses. Eighteen psychiatric hospitals are public and belong to either the Ministry of Health or a Czech administrative region; three psychiatric hospitals are private.
Two Czech psychiatric hospitals participated in the aforementioned 2017 WHO survey assessing adherence to the CRPD.10 For our study, we invited all but one of the Czech Republic’s public psychiatric hospitals to participate in a nationwide evaluation of adherence to the CRPD in 2018 or early 2019. One smaller public psychiatric hospital was not included because it was already assessed within the 2017 WHO survey. We did, however, invite the other psychiatric hospital that participated in the 2017 survey because only a portion of the hospital’s approximately 30 wards had participated in the WHO survey.
In total, 16 of the 17 public psychiatric hospitals we invited participated in our study. The one public hospital that declined our invitation is a relatively small institution, with 70 beds, and belongs to one of the Czech administrative regions. This paper synthesizes the findings from our study, as well as the results from one of the hospitals that participated in the 2017 WHO survey, in order to present results for 17 of the country’s 18 public psychiatric hospitals.
Instrument
The WHO QualityRights Toolkit is divided into five basic themes, each focused on specific articles of the CRPD: (1) articles 12 and 14 (the right to exercise legal capacity and the right to personal liberty and the security of person); (2) articles 15 and 16 (freedom from torture and cruel, inhuman, or degrading treatment or punishment and freedom from exploitation, violence, and abuse); (3) article 19 (the right to live independently and be included in the community); (4) article 25 (the right to enjoyment of the highest attainable standard of physical and mental health); and (5) article 28 (the right to an adequate standard of living). The themes are divided into standards, which consist of different criteria. The instrument allows each criterion to be scored as follows: “not initiated,” “achievement initiated,” “achieved partially,” “achieved in full,” and “not applicable.” Under the tool, criteria are evaluated first. Then, a score is assigned to individual standards, based on both the scores of all criteria belonging to a given standard and on a discussion among team members. Therefore, the score for a standard is not a mere arithmetical mean of its criteria, nor is the score for a given theme. As a result, the evaluating team provides descriptions and justifications for the scores it awards to each criterion, standard, and theme, especially when adherence is considered to have only been initiated or not initiated at all.
Assessment
Our evaluation teams consisted of five evaluators: a psychiatrist, a social worker, a human rights lawyer, a service user, and a researcher. All evaluators, with the exception of substitutes, were trained in the use of the WHO QualityRights Toolkit by WHO experts during two-day workshops. Evaluation team members were encouraged to avoid any conflict of interest—that is, to dismiss themselves from assessments where a conflict of interest could arise, for example, because they were previously admitted to or employed by a hospital or because they had professional ties with a given hospital.
Evaluation visits were initiated by the Ministry of Health and planned in cooperation with management from each hospital. Visits lasted two or three days (according to the size of the psychiatric hospital) and included interviews with service users, relatives and close friends of service users, and hospital staff; an analysis of internal documents; non-participant observations; and participant observations (for example, participation in selected therapeutic activities). Overall, we conducted 579 interviews with 308 staff members (72 members of management, 224 staff who provide direct care, and 9 in other positions), 250 service users, and 21 family members and friends.
All members of the evaluation team were present during visits. Evaluation reports were produced following each visit. These reports included a basic description of the facility; the team’s assessment methodology and a basic description of the sample; scores and justifications for each standard, criterion, and theme; context surrounding the institution; discussion surrounding the five themes; and recommendations for improving CRPD adherence. Evaluation scores were determined by consensus—in other words, based on discussion and agreement among the evaluation team. The evaluation team considered all available information, including observations, documentation, and interviews with service users, professionals, and family members. Interviews were guided by the WHO QualityRights Toolkit, which provides a set of questions for each standard.11 In the case of ambiguity, the team conducted additional interviews. Rarely, when team members were unable to reach consensus, they voted in order to arrive at a final score.
Analyses
The data are presented anonymously and graphically, using clustered bar charts. One chart presents the results for adherence across all five themes, and five individual charts present the results for individual standards within each theme. In order to identify priority areas for improvement across psychiatric hospitals, we further analyzed the standards and themes that were least frequently adhered to according to the charts. To do this, we extracted qualitative descriptions and justifications provided by evaluation teams’ reports across priority themes and standards for individual institutions and across all assessed institutions. Narrative discussion surrounding each of the five themes and recommendations for improving adherence are provided for both individual institutions and Czech psychiatric hospitals generally. The recommendations are our own and do not necessarily reflect the views of the evaluation teams.
Ethical considerations
All members of our evaluation teams signed a nondisclosure agreement. All interviewees received information about the study and provided written informed consent. Ethical approval for this study was provided by the Ethical Committee of the National Institute of Mental Health in 2017 (ID 188/17) and the Ethical Committee of the Ministry of Health in 2018 (ID MZDRP011FZ5B).
Results
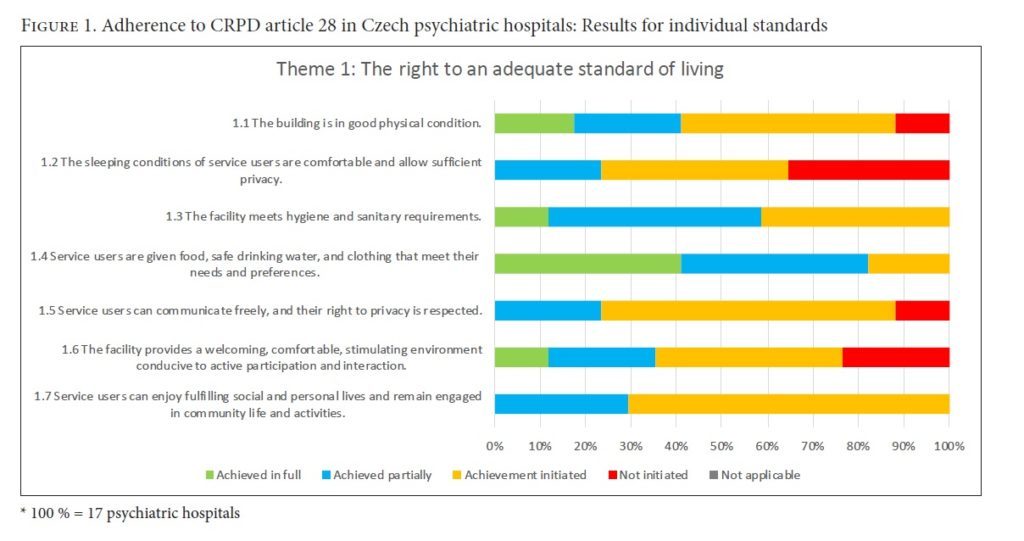
Theme 1: The right to an adequate standard of living (CRPD art. 28)
In regard to overall adherence to theme 1, only one hospital was not actively initiating changes to assure an adequate standard of living for patients. However, no hospitals fully met the criteria of this standard. The hospital buildings were found suitable for usage following some technical adjustments. Almost one-third (5 of 17) of the hospitals were not wheelchair accessible, and only two psychiatric hospitals were fully barrier free. While most of the hospitals were investing in building reconstruction, only three hospital buildings provided a sufficiently adequate standard of living according to CRPD standards.
The evaluation teams found serious shortcomings in the area of comfortable sleep conditions and privacy, as well as room capacity discrepancies between buildings and hospitals. In newly reconstructed buildings, rooms usually accommodated two to three beds; however, some wards had fourteen-bed rooms. A strict daily regime was followed in most of the hospitals, and half of them allowed patients to choose when to get up and go to bed. Patients’ rooms had non-locking doors, and lockers were not provided for personal belongings. Additionally, mobile phones, personal documents, and other personal belongings were usually kept in the nurses’ office.
Patients’ overall right to privacy was not fully respected within the hospitals. The majority of the hospitals we evaluated had not fully achieved CRPD-compliant conditions regarding facility sanitation. Patients shared common toilets with non-lockable doors and open showers. Regarding the food served, the dietary preferences of hospitalized patients were not considered, but minimum dietary requirements were fully adhered to.
Evaluation teams agreed that the food served should contain more fresh fruit and vegetables, legumes, and dairy products. However, most patients did not complain about the quality of their diet. Most of the hospitals (12 of 17) fully respected the patient’s right to choose their clothing.
The evaluation teams found significant shortcomings in terms of the communication technologies available to patients. Time restrictions were applied to private mobile phone use, Wi-Fi connections were rarely available, and few wards employed a point reward system as a condition for using the facility phone. There also was a lack of privacy for personal communication, with insufficient or no rooms for personal visits, and no sound barriers for facility phones. Some hospitals (3 of 17) had no measures in place to meet adherence to this standard.
Consistent with the state of buildings, room furnishings required significant remodeling. Rooms were scarcely equipped, usually consisting of only a bed, bedside table, and closet. Some wards lacked a common room, which significantly limited social life within the facility, since patients, personnel, and visitors could not come together in a common setting. Staff rooms were sometimes located outside of the ward, separating personnel and service users and decreasing the sense of community. Leisure time activities usually took place in the eatery or hallways. Only a third (5 of 17) of hospitals fully met CRPD adherence in providing an environment conducive to active participation and interaction.
None of the hospitals we assessed fully achieved the CRPD standard for patients’ engagement in the community. Patients could meet with patients of the opposite sex only through gaining permission to leave their department. However, personnel in most psychiatric hospitals (12 of 17) proactively provided assistance for patients’ personal affairs (for example, attending a wedding or a funeral). All psychiatric hospitals at least initiated organizing and providing information about social events within the hospital facility. On the other hand, none fully respected the CRPD recommendation to build an interactive environment between hospital and community.
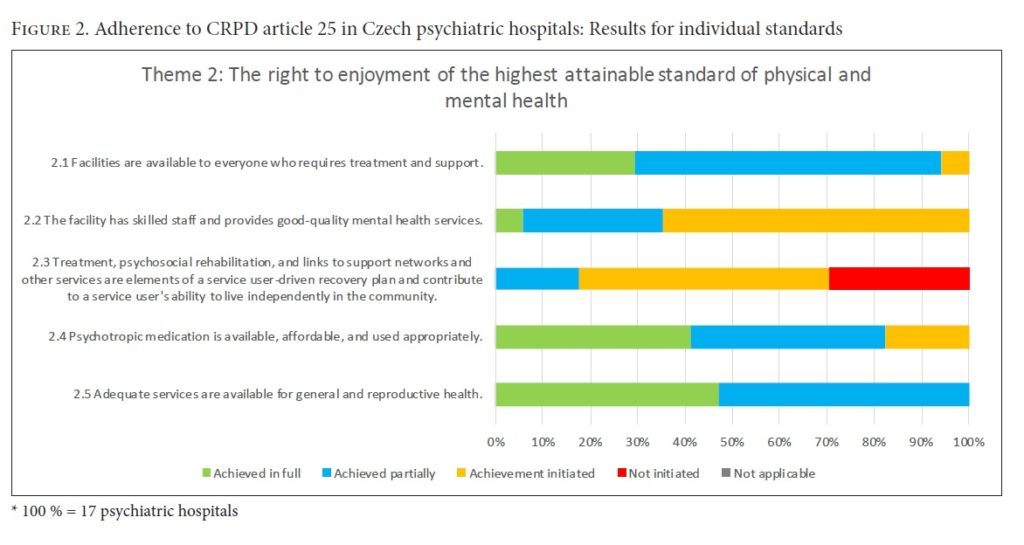
Theme 2: The right to enjoyment of the highest attainable standard of physical and mental health (CRPD art. 25)
While adherence to theme 2 was fully achieved in only one psychiatric facility, all of them had at least initiated changes toward fulfilling the theme. Almost all psychiatric hospitals at least partially met the standard of providing adequate treatment and support to everyone in need. However, treatment for foreigners and people with disabilities fell short. A lack of translation services acted as a barrier to non-Czech speaking patients’ participation in talking therapy. Additionally, the inaccessible state of hospital buildings detailed in theme 1 limited the scope of care provided to people with physical disabilities. No cases were uncovered where treatment was denied to anyone based on economic or social status, race, sex, religion, or political or philosophical opinions. Additionally, service users often remained hospitalized for non-health-related reasons, usually a lack of transitionary and follow-up services or inadequate financial security of service users.
Facility staff demonstrated significant knowledge gaps in terms of patients’ rights—11 of the 17 hospitals had no rights-based trainings. Trainings on how to adequately support patients in social and community integration and independent living were largely lacking, with only a third of psychiatric hospitals training their staff in the benefits of multidisciplinary treatment and community-based care models. Some wards lacked adequate numbers of mental health professionals, though patients had adequate access to individual consultations with a psychiatrist. Most psychiatric hospitals had at least initiated mechanisms for service users to express their opinions on service provision and improvements. Areas for improvement identified by patients included the establishment of independent commissions and the introduction of anonymous complaint processes that are accessible and understandable to patients.
The evaluation teams identified various deficits surrounding recovery plans. According to service users, a third of the hospitals (5 of 17) had initiated no efforts toward the preparation of recovery plans. Of the remaining facilities, only two at least partially met the criteria stated by standard 2.3. Patients’ individual preferences were not considered because of the strict regime of treatment. In the majority of hospitals (11 of 17), individual recovery plans did not exist; and in three, individual plans existed but lacked complexity, excluding the patient from the process of developing the plan. A few psychiatric hospitals had guidelines regarding the development of either recovery plans or “previously expressed wishes,” but the development and implementation of such documents was lacking, and neither patients nor staff were acquainted with these guidelines or documents.
Psychosocial therapeutic programs were available and systematically incorporated into individual treatments in all psychiatric hospitals except one; however, these programs were not accessible to all patients. Patients were not sufficiently supported in keeping social contact with family and close ones. The strict regime in psychiatric hospitals (including limited outings, visiting hours, ward visits, mobile phone usage, and Wi-Fi connections), scarce communication between hospital staff and patients’ families, and insufficient staff capacity prevented adequate support networks for patients. About a third of the hospitals (5 of 17) had fully developed systems for follow-up services, including health (outpatient psychiatric clinics and somatic services) and social (mental health community care and social-based inpatient facilities) services. The remaining facilities had a shortage of integrated social-health professionals, resulting in social services being dependent on external providers.
About a quarter (4 of 17) of the hospitals fully met the standard on availability, affordability, and adequate usage of psychopharmaceutic drugs. Generally, psychopharmaceuticals were widely available. About half of the hospitals (7 of 17) used modern medications and conducted regular reviews of prescribed medications. According to the CRPD, patients in psychiatric hospitals should be adequately informed about the purpose and potential side effects of prescribed medications, as well as attainable alternatives to medications, which was not adhered to. Service users occasionally did not know which medication they were on and were generally uninformed of the drug’s purposes, side effects, and alternative treatments. Service users’ lack of knowledge of alternatives to medication (such as psychotherapy) is worth considering, especially in the context of the unavailability of these alternatives in the majority of psychiatric hospitals (10 of 17).
Services for physical health were accessible in all of the psychiatric hospitals. Specifically, physical health screening was available upon admission, and no deficits were found in the provision of surgical or medical procedures provided outside of the facility. However, preventive education programs on general health and reproductive health were not systematically provided in the vast majority of hospitals, apart from smoking reduction programs.
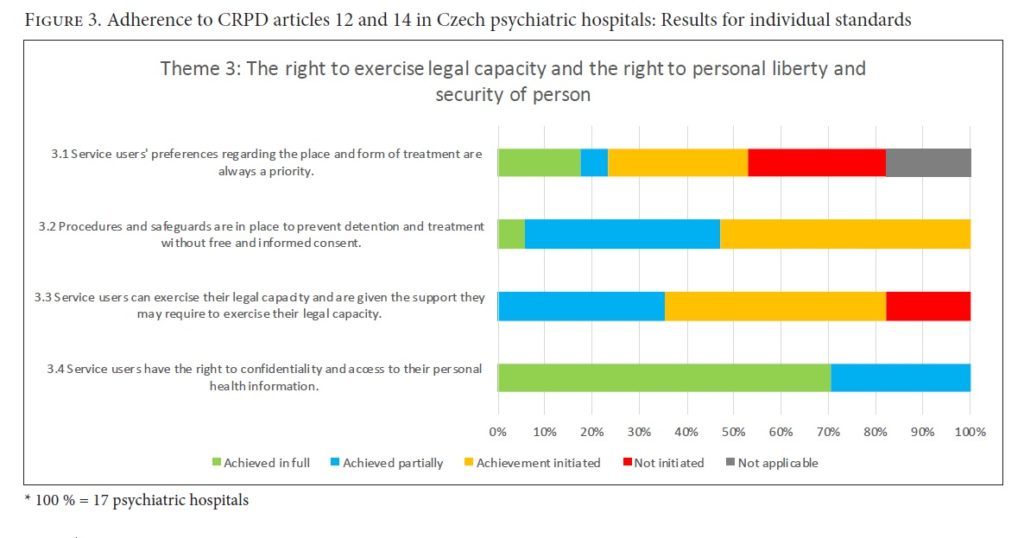
Theme 3: The right to exercise legal capacity and the right to personal liberty and the security of person (CRPD arts. 12 and 14)
All 17 psychiatric hospitals had at least initiated changes toward fulfilling patients’ rights regarding legal capacity and personal liberty and security. However, patients’ preferences concerning the place and form of their treatment were not prioritized.
According to the CRPD, treatment should be based on patients’ free and informed consent. In general, fulfilment of this standard had been at least initiated in all of the psychiatric hospitals. However, treatment-related communication was not always fully understandable to patients, and the document containing “previously expressed wishes” was used in only 3 of the 17 hospitals. There were no cases of neglecting a patient’s right to refuse treatment or of inappropriate involuntary treatment found within the health records we reviewed. On the other hand, the opportunity to appeal involuntary treatment was not clearly or adequately communicated or detailed to service users.
While 13 hospitals had taken measures toward adhering to the exercise of patients’ legal rights, a paternalistic approach to service users remained dominant in most facilities. Education on rights and treatment was lacking, and supported decision-making was not systematically incorporated into services.
Service users’ right to access personal health information was respected, and access to one’s own medical records was available to all patients. Service users were also permitted to add supplemental information to their records; however, most patients were not aware of this option. Personal health information was treated as confidential.
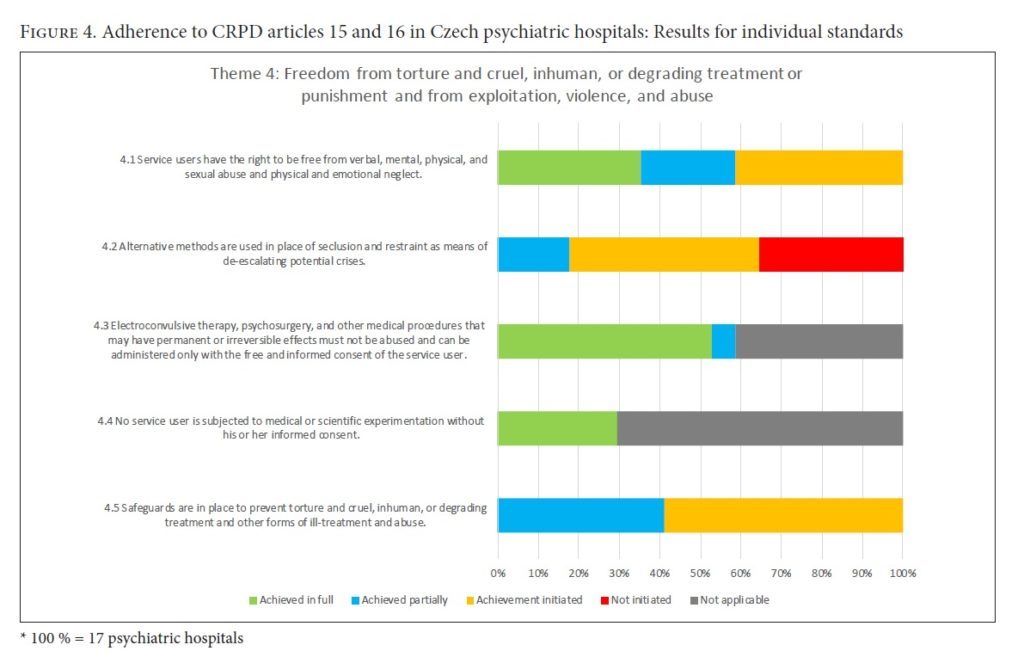
Theme 4: Freedom from torture and cruel, inhuman, or degrading treatment or punishment, and from exploitation, violence, and abuse (CRPD arts. 15 and 16)
While none of the psychiatric hospitals fully adhered to this theme, more than half had at least initiated efforts toward its achievement. In 13 of the 17 hospitals, the use of medical restraints was in line with Czech legislation, and such instances were reported consistently to the head of the facility. Alternative methods to seclusion or restraint (such as de-escalation methods for potential crises) were often not in place. In 11 psychiatric hospitals, de-escalation methods were not used, nor were potential trigger factors for crisis evaluated. Emergency plans and personal recovery plans were missing across all of the psychiatric hospitals.
Insufficient access to legal representation was found in 8 of the 17 hospitals. Service users were not given information on independent legal authorities (such as the Ombudsman’s Office). Additionally, when service users’ communication was perceived as inappropriate (for example, shouting), punishments were in place (for instance, transfer to a closed department). Bullying among users was also noted as an issue.
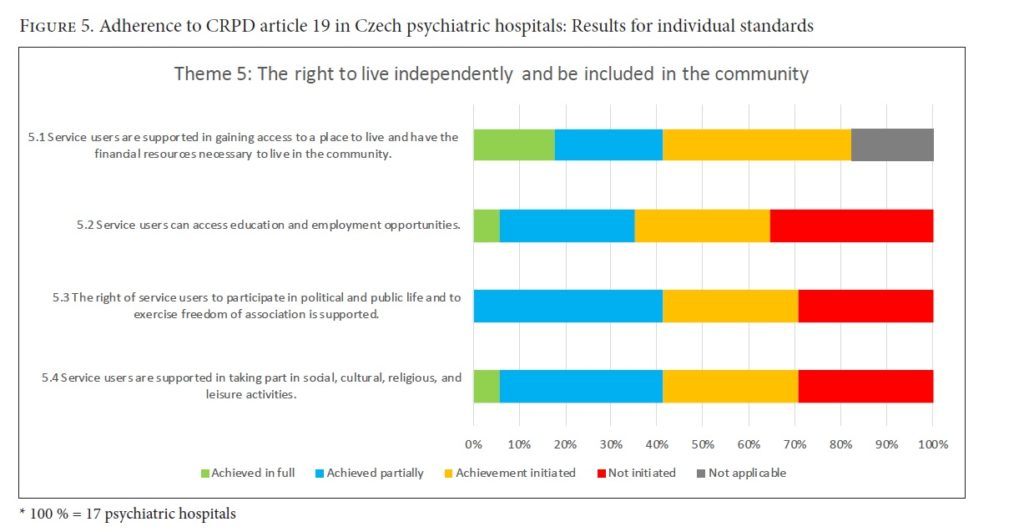
Theme 5: The right to live independently and be included in the community (CRPD art. 29)
Service users were supported in securing a place to live in the community. However, the lack of staff, especially social workers, prevented service users from being adequately informed about all available options. Additionally, only two hospitals provided patients with sufficient access to education. The hospitals did not prevent users from participating in political, public, or community life, but they did not actively support or promote it.
Summary of results
In general, Czech psychiatric hospitals are in poor physical shape, are suboptimal for quality sleep, lack comfort and room for interaction, and do not meet many hygiene and sanitary requirements. Nutrition and clothing are mostly up to standards, except for some shortcomings with respect to the preferences of service users. Freedom of communication is low because of censorship, a lack of privacy, and service users’ restricted access to facility premises. The social life of patients is also limited, especially with regard to social and cultural events outside of the hospital. The availability of care in psychiatric hospitals is very good, however provision of mutli-sectoral services and human rights training for staff lack.
Individual recovery plans are scarce, and treatment and rehabilitation do not sufficiently take into account service users’ preferences. Psychopharmaceuticals are widely available, but service users receive little information related to psychopharmacological treatment. Physical and reproductive health care is available, but again, service users receive little information about health care options.
Across the psychiatric hospitals, service users enjoy marginal participation in deciding their treatment and lifestyle, advanced directives are not utilized, and service users are provided with minimal support for decision making. Although the maintenance of patient records is good, service users have very little opportunity to add their comments, opinions, and perspectives. Patients are generally treated with dignity, but help and support are not optimally provided in cases of adverse events. Protection against inappropriate treatment is also suboptimal.
A major problem is the use of constraints, both in the context of crisis management and in the context of subsequent evaluation of crisis; and again, service users’ preferences are often not taken into account. The use of special medical procedures, such as electroconvulsive therapy, is generally good, with the exception of one hospital that, according to the electroconvulsive therapist, applied such treatment to young people aged 16–17 approximately 10 times over the past five years. All research studies in psychiatric hospitals practice adhere to the CRPD.
Service users are provided with good support for life in society in terms of assistance with housing and income. However, access to education and employment, as well as support for participation in public life, is very low.
From the perspective of service users, boredom and limited opportunities for independent living are major problems. This is illustrated in the following excerpts from our interviews with service users:
People here have low moods, everyone is just sleeping. As soon as 7 p.m. comes, after pharmaceuticals, all go to bed, because there is nothing they would enjoy. Smoking, sleeping, smoking, sleeping—this is the rhythm of this ward.
They close bedrooms for the whole midmorning, they say it’s so they can be ventilated. So we lay around on the ground. We have pharmaceuticals that make us sleepy, but we cannot go to bed.
They close bedrooms for the whole midmorning, they say for cleaning purposes, but the reason is to not allow us to lie in beds. At least they do not close the smoking room.
We cannot have any money—we have a card which we can use just in one shop [located on the hospital premises]. There they note what we buy, and a social nurse discounts this from our account.
I have been here since I was 18, and now I am 81, which is 63 years. It is such a certainty for me. Actually, I spend all my time in one room, where there are a total of seven people. I am used to it now. I have been here longer than most of the doctors or nurses.
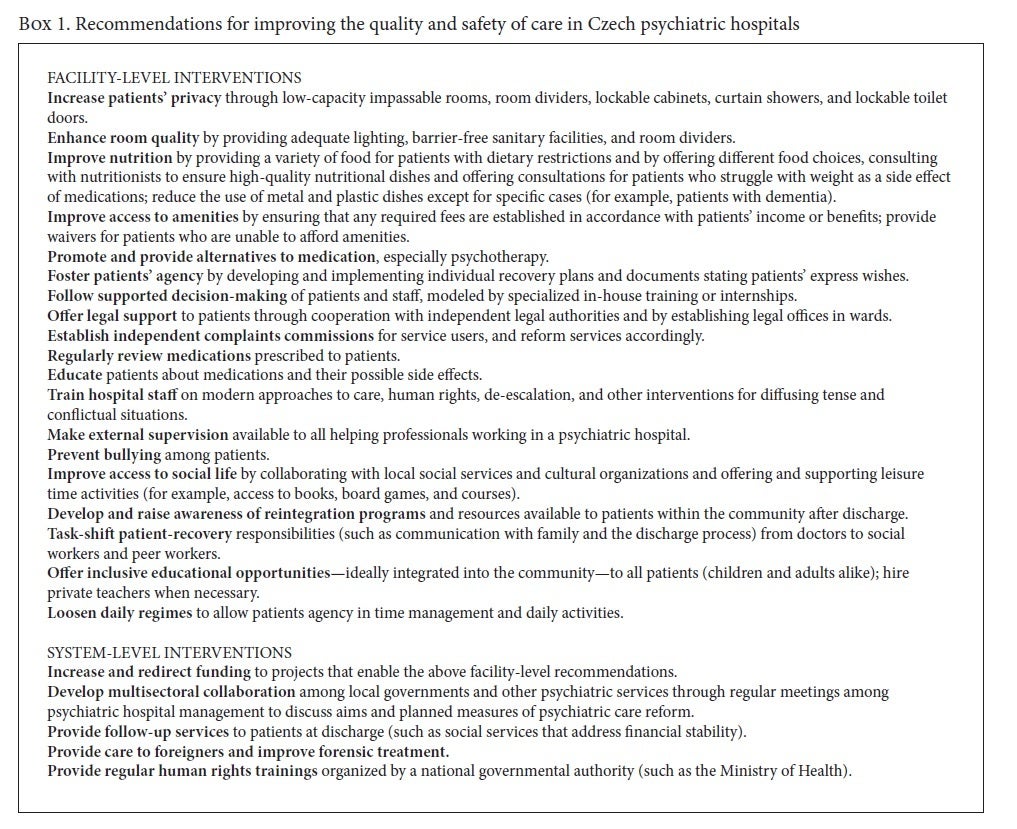
Recommendations based on our study’s results are outlined in Box 1.
Discussion
Our systematic assessment of the quality of care and adherence to the CRPD in Czech psychiatric hospitals revealed serious shortages in almost all themes within the WHO QualityRights Toolkit. The majority of shortcomings are linked to the unsatisfactory state of buildings, the lack of qualified and thoroughly trained staff, insufficient support for service users’ decisions and preferences, and insufficient emphasis on service users’ integration into society.
These results are notably worse than the results of the 2017 WHO study assessing European long-term residential institutions for people with psychosocial disabilities.12 Discrepancies may be partially explained by the fact that participating institutions from the WHO study were chosen by countries’ ministries of health or social affairs and thus may not have been nationally representative. The WHO study also included countries from all over Europe, with various historical, cultural, and political contexts. Our study confirms some of the findings from the WHO study, including the restriction of service users’ communication, lack of staff knowledge about consent for admission and treatment, lack of supported decision-making for service users, lack of individualized treatment and recovery plans, and lack of access to supported community housing.13 However, unlike the WHO study, our study did not reveal the potential exploitation of service users’ labor as a problem in the Czech Republic.
Psychiatric hospital buildings in the Czech Republic are in a profound state of disrepair and require extensive renovations to create an environment suitable for CRPD adherence. From an economic point of view, community-based care has been found to be highly cost-effective when compared to psychiatric hospitals both in “old” European Union member states and in the Czech Republic.14 Taking into consideration that there is an overlap between service users in psychiatric hospitals and those in community care, the pursuit of deinstitutionalization of mental health services is supported by both a human rights perspective and an economic one.
The use of restraint and seclusion measures is particularly problematic. Most staff lack training in de-escalation techniques, and patient-preferred methods of intervention during crisis are not taken into account. Following this finding, a workshop for staff from Czech psychiatric hospitals on alternatives to restrictive interventions was organized by the “Deinstitutionalization” project team in collaboration with WHO in February 2019. Further workshops and training activities will follow within the course of reform. Regardless, deinstitutionalization needs to be pursued to achieve full adherence to the CRPD and hopefully also to improve other important outcomes, such as suicide and mortality rates, which are particularly high among people hospitalized in Czech psychiatric hospitals.15
The strengths of our study include a high participation rate (17 out of 18 psychiatric hospitals participated in the evaluation); thoroughly trained evaluation teams; the use of a comprehensive WHO QualityRights Toolkit instrument; and a high number of interviews. All of these factors contributed to a detailed assessment of facilities’ adherence to the CRPD. Some noteworthy limitations exist, including the fact that only a few wards in each of the participating hospitals were assessed, which might have influenced the representativeness and consequently the generalizability of our results. Indeed, evaluation teams reported that the quality of the wards from the same psychiatric hospital may differ substantially, depending, for instance, on staff training and traits. Furthermore, evaluation teams were ambivalent when scoring in areas that were felt to mirror specific cultural values. This was the case, for instance, with regard to dietary requirements and, perhaps even more importantly, the issues of freedom of movement, sexual needs, and freedom of choices. In these instances, psychiatrist team members often expressed the opinion that it is necessary or normal for users, for example, to be woken up around 5 a.m. because hospitals’ regimes require this. In these cases, discussions occasionally ended up with disagreements, and voting had to be used to arrive at a final score for a given criterion. Additionally, evaluation teams occasionally reported that some of the interviewed patients might have been afraid to speak openly because of the anticipated negative rewards from hospital personnel. Despite being somewhat worried, service users were notably more critical than professionals. Professionals were often convinced that the living standards in the hospitals were “not that bad” and that there was no reason for complaint. Frequently, there was no alignment between the views of patients and those of professionals.
The results of our nationwide study are in line with previous findings from the Czech ombudsman and are considerably worse than the results of the 2017 WHO survey.16 Despite current efforts to improve the quality of care in Czech psychiatric hospitals, such as the “System of Integrated Psychiatric Rehabilitation” project, treatment and rehabilitation does not sufficiently follow recovery principles.17
The 2017 WHO European study synthesized overarching priorities for improved CRPD adherence, including (1) continuous assessments and monitoring of progress; (2) staff training; and (3) exchange of knowledge and learning in pursuit of CRPD adherence in Europe.18 Taking into consideration these and the priorities emerging from our study, we developed specific recommendations for improving the quality and safety of care in psychiatric hospitals at both the facility and the system level (Box 1). The results from our study not only provide justification for the continued reform of psychiatric care in the Czech Republic but also offer a resource to help motivate and inform rights-based mental health initiatives in neighboring countries in Central and Eastern Europe, which share a history of communist and socialist influences on their sociopolitical and economic state and, in turn, on the development and provision of mental health services.19 Based on the results of our study, some important steps to improve the quality and safety of care in Czech psychiatric hospitals, such as the recent WHO-led training of staff to reduce the use of restrictive measures, have already been launched. Hopefully, other countries in the region will follow suit.
Funding
We were supported by the project “Sustainability for the National Institute of Mental Health” (grant LO1611), funded by the Ministry of Education, Youth and Sports of the Czech Republic; and by the project “Deinstitutionalization of Mental Health Care” (CZ.03.2.63/0.0/0.0/15_039/0006213), funded by the European Structural and Investment Funds as administered via the Ministry of Labor and Social Affairs of the Czech Republic. The funding bodies had no role whatsoever in the design of our study, methodology used, data collection, data analysis, data interpretation, or writing of this paper.
Petr Winkler, PhDr, PhD, is Head of the Department of Public Mental Health at the National Institute of Mental Health, Czech Republic.
Lucie Kondrátová, MSc, is a researcher at the Department of Public Mental Health at the National Institute of Mental Health, Czech Republic.
Anna Kagstrom, MSc, is a researcher at the Department of Public Mental Health at the National Institute of Mental Health, Czech Republic.
Matěj Kučera is a researcher at the Department of Public Mental Health at the National Institute of Mental Health, Czech Republic.
Maria Salomonová, MSc, is Chief Executive Officer at Nevypusť duši, Czech Republic.
Petr Šturma is a freelance manager and lecturer with extensive experience in community mental health and anti-stigma projects, Czech Republic.
Zbyněk Roboch is a researcher at the Department of Public Mental Health at the National Institute of Mental Health, Czech Republic.
Melita Murko is a Technical Officer with the Mental Health Programme, World Health Organization Regional Office for Europe, Denmark.
Please address correspondence to Petr Winkler. Email: petr.winkler@nudz.cz.
Competing interests: None declared.
Copyright © 2020 Winkler, Kondrátová, Kagstrom, Kučera, Palánová, Salomonová, Šturma, Roboch, and Murko. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- E. Dwyer, “The final years of Central State Hospital,” Journal of the History of Medicine and Allied Sciences 74 (2019), pp. 107–126; P. Murthy, M. Isaac, and H. Dabholkar, “Mental hospitals in India in the 21st century: Transformation and relevance,” Epidemiology and Psychiatric Sciences 26 (2017), pp. 10–15; M. Rekhis, A. Ben Hamouda, S. Ouanes, et al., “Rights of people with mental disorders: Realities in healthcare facilities in Tunisia,” International Journal of Social Psychiatry 63 (2017), pp. 439–447; R. Van Voren, Psychiatry as a tool for coercion in post-Soviet countries (Brussels: Directorate-General for External Policies of the Union, European Union, 2013).
- R. Christenfeld, “Deinstitutionalization and its critics: A commentary on Brown,” Journal of Community Psychology 10 (1982), pp. 176–180; A. D. Lesage, R. Morissette, L. Fortier, et al., “I. Downsizing psychiatric hospitals: Needs for care and services of current and discharged long-stay inpatients,” Canadian Journal of Psychiatry 45 (2001), pp. 526–532; G. Thornicroft and P. Bebbington, “Deinstitutionalisation: From hospital closure to service development,” British Journal of Psychiatry 155 (1989), pp. 739–753.
- P. Winkler, B. Barrett, P. Mccrone, et al., “Deinstitutionalised patients, homelessness and imprisonment: Systematic review,” British Journal of Psychiatry 208 (2016), pp. 421–428; P. Winkler, D. Krupchanka, T. Roberts, et al., “A blind spot on the global mental health map: A scoping review of 25 years’ development of mental health care for people with severe mental illnesses in central and eastern Europe,” Lancet Psychiatry 4 (2017), pp. 634–642.
- S. Pirkola, B. Sohlman, H. Heilä, et al., “Reductions in postdischarge suicide after deinstitutionalization and decentralization: A nationwide register study in Finland,” Psychiatric Services 58 (2007), pp. 221–226; S. Pirkola, R. Sund, E. Sailas, et al., “Community mental-health services and suicide rate in Finland: A nationwide small-area analysis,” Lancet 373 (2009), pp. 147–153.
- Winkler et al. (2017, see note 3).
- Ministry of Health of the Czech Republic, Reforma péče o duševní zdraví: Strategie reformy psychiatrické péče [Mental health care reform: Strategy] (Prague: Ministry of Health, Czech Republic, 2013).
- Convention on the Rights of Persons with Disabilities, G.A. Res. 61/106 (2006).
- N. Drew, M. Funk, S. Tang, et al., “Human rights violations of people with mental and psychosocial disabilities: An unresolved global crisis,” Lancet 378 (2011), pp. 1664–1675; M. C. Freeman, K. Kolappa, J. M. C. De Almeida, et al., “Reversing hard won victories in the name of human rights: A critique of the General Comment on Article 12 of the UN Convention on the Rights of Persons with Disabilities,” Lancet Psychiatry 2 (2015), pp. 844–850; G. Szmukler, R. Daw, and F. Callard, “Mental health law and the UN Convention on the rights of persons with disabilities,” International Journal of Law and Psychiatry 37 (2014), pp. 245–252.
- World Health Organization, Mental health, human rights and standards of care: Assessment of the quality of institutional care for adults with psychosocial and intellectual disabilities in the WHO European Region (Copenhagen: World Health Organization, 2018).
- Ibid.
- World Health Organization, WHO QualityRights tool kit to assess and improve quality and human rights in mental health and social care facilities (Geneva: World Health Organization, 2012).
- World Health Organization (2018, see note 9).
- Ibid.
- M. Knapp, J. Beecham, D. Mcdaid, et al., “The economic consequences of deinstitutionalisation of mental health services: Lessons from a systematic review of European experience,” Health and Social Care in the Community 19 (2011), pp. 113–125; P. Winkler, H. M. Broulíková, L. Kondrátová, et al., “Value of schizophrenia treatment II: Decision modelling for developing early detection and early intervention services in the Czech Republic,” European Psychiatry 53 (2018), pp. 116–122; P. Winkler, L. Koeser, L. Kondrátová, et al., Cost-effectiveness of care for people with psychosis in the community and psychiatric hospitals in the Czech Republic: An economic analysis,” Lancet Psychiatry 12 (2018), pp. 1023–1031.
- Winkler et al. (2017, see note 3); P. Winkler, K. Mladá, L. Csémy, et al., “Suicides following inpatient psychiatric hospitalization: A nationwide case control study,” Journal of Affective Disorders 184 (2015), pp. 164–169.
- World Health Organization (2018, see note 9).
- L. Kalisova, M. Pav, P. Winkler, et al., “Quality of care in long-term care departments in mental health facilities across the Czech Republic,” European Journal of Public Health 28 (2018), pp. 885–890.
- World Health Organization (2018, see note 9).
- Winkler et al. (2017, see note 3); Ministry of Health of the Czech Republic (see note 6).