Volume 23/2, December 2021, pp. 139-151 | PDF
Thalia Viveros-Uehara
Abstract
Given that the health-related impacts of climate change in Latin America disproportionately affect the most marginalized sections of the population, there is a need to enhance countries’ adaptive capacity through improved health systems. Though public health institutions have delineated guidelines to enhance health care systems’ preparedness for climate change, embedding a human rights perspective in their translation into laws and policies further adds important value. Crucially, a rights-based approach strengthens health responses to climate change by calling attention to how climate law and policy fail to account for persistent and interlocking socioeconomic inequalities. This is an area that has not been fully present in the provision of health services in Latin America, which rely almost exclusively on a conventional epidemiological perspective and do not consider the historical and sociocultural nature of health challenges. Hence, this paper draws on two case studies—Brazil and Colombia—to identify the extent to which their national climate change laws and adaptation plans incorporate a human rights-based approach in their tasks to enhance their adaptation capacity through the expansion of affordable and quality health care. With respect to the countries’ laws, the absence of explicit references to the right to health exemplifies the fragmentation between the international human rights framework and international climate change law. Further, both countries’ adaptation plans hold considerable room for improving their engagement with the human rights framework, particularly by establishing mechanisms to promote transparency, monitoring, and the participation of marginalized groups.
Introduction
The impacts of climate change on health have already manifested in the Latin American region. Concerningly, an abundance of scientific evidence has revealed how climate change is exacerbating disease and pest transmission while also increasing morbidity, mortality, and disabilities due to extreme weather events.[1] The Office of the United Nations High Commissioner for Human Rights has documented these climate-related effects as threats to the realization of the right to health.[2]
The highly uneven access to and quality of health care in Latin America further aggravates such risks.[3] Public health researchers have shown that persons living in poverty and members of minority groups often lack access to quality health care—which denies them the opportunity to prevent, treat, cure, and rehabilitate climate-related health conditions.[4]
Health care systems are thus key determinants of countries’ capacity to adapt to climate change.[5] In that vein, states have the obligation to take measures to develop sustainable and resilient health care systems and infrastructure to ensure climate-resilient populations, thereby fulfilling their minimum core obligations with regard to the right to health.[6]
Even though the United Nations human rights system has called for integrating a human rights-based approach (HRBA) into climate adaptation, which includes health-related policies, the technical guidelines for the elaboration of national adaptation plans (NAPs)—the primary instruments for vulnerability reduction under the United Nations Framework Convention on Climate Change (UNFCCC)—have not reflected this approach.[7] The health dimension of NAPs (H-NAPs) has been informed primarily by a public health approach to climate change.[8]
While an HRBA shares several commonalities with good public health practice, it adds further value due to its foundation in international law, which supplies legitimacy (given that countries have agreed to abide by these laws), imposes legal obligations and mechanisms of accountability, and ensures coherence across sectoral policies.[9] Moreover, human rights principles and standards draw attention to how climate law and policy fail to account for persistent and interlocking socioeconomic inequalities. This is an area that has been lacking in the provision of health services in Latin America, which rely almost exclusively on a conventional epidemiological perspective and do not take into consideration the historical and sociocultural nature of health challenges.[10]
Hence, as the adoption of national climate change laws and NAPs has come to be the primary proxy for assessing countries’ progress in adaptation (for example, in indicator 13.2.1 of the Sustainable Development Goals and indicator 2.1.1 of the 2020 Lancet Countdown report), examining the extent to which these laws and plans incorporate an HRBA to health yields useful learnings.[11] Significantly, such a review adds an analytical layer to these indicators by shedding light on the extent to which they capture how socioeconomic inequalities play out in climate adaptation in the health sector.
This paper provides the first review in the literature of the intersection between human rights, climate change adaptation, and health care for NAPs. It observes Brazil and Colombia as two case studies to identify the extent to which their national climate change laws and H-NAPs incorporate an HRBA in their tasks to enhance their adaptation capacity through the expansion of affordable and quality health care. More specifically, the study asks the following overarching question: Do these climate laws and national adaptation plans take a human rights-based approach to expanding affordable and quality health care access, particularly for the most vulnerable persons and groups?
This review purposively studies Brazil and Colombia because they are the only two countries in Latin America that (1) have legally recognized the right to health (by agreeing to abide by the International Covenant on Economic, Social and Cultural Rights and the Protocol of San Salvador); (2) have enacted national climate laws; (3) have submitted their NAPs to the UNFCCC NAP Central; and (4) are experiencing the highest vulnerability across the Lancet Countdown’s indicators pertaining to the impacts of heat, extreme weather events, and climate-sensitive infectious diseases on health (indicators 1.1, 1.2, and 1.3, respectively).[12] It argues that both countries still have room to improve how they embed an HRBA into their national climate change laws and NAPs. This is not a minor issue. Given Brazil’s and Colombia’s socioeconomic inequalities, guiding adaptation efforts toward addressing persistent exclusion in health care and health care policy is a crucial step to avoid further human suffering and losses. An HRBA must therefore be explicitly invoked, starting with planning tools.
This paper begins with a brief overview of the relationship between climate change and health in Brazil and Colombia. It then presents the theoretical background in which an HRBA to health and public health approaches to climate change are brought into interaction. Next, it describes the review’s comparative methodology, followed by a discussion of the findings. Finally, the conclusion comments on future avenues for research.
Health and climate change in Brazil and Colombia
The Intergovernmental Panel on Climate Change has documented variations in the climatic patterns of Brazil and Colombia, along with their effects on human health.[13] While both countries exhibit high health vulnerability to climate change, and their projected climate scenarios indicate an increased frequency and intensity of extreme weather events, unequal access to health care services continues to be a major determinant of the health outcomes of minority groups and persons living in poverty, which is concerning.[14]
Over the last half of the 20th century, Southern Brazil has witnessed an increase of 0.6°C per decade in mean annual air temperature, as well as an increased frequency of heavy rainfall.[15] Meanwhile, dryness has increased in North and Northeast Brazil.[16] During the 1990s, changes in land development and regional climate contributed to a resurgence of malaria in the Amazon region.[17] Further, increases in hospital admissions due to diarrhea were associated with climatic variations.[18]
Disparities in health care access and quality within the country are worrying. Brazil’s Amazonian North has 1.1 medical doctors per 1,000 inhabitants, compared to 2.8 per 1,000 in the richer Southeast.[19]
Even though recent decades have witnessed progress in neglected diseases’ control and elimination due to increased policy attention and funding, this progress has been limited for remote populations located far from power centers.[20] Children’s health care has also remained unequal. While Amazonas’ population exceeds Brasília’s by almost one million inhabitants, it has only 344 pediatricians compared to the federal capital’s 1,347.[21] Furthermore, this state’s remote rural settlements are less likely to have primary health care providers.[22]
According to Colombia’s latest national communication to the UNFCCC, almost half of the country’s territory is at high or very high risk of experiencing climate change impacts.[23] From 1959 to 2005, the Colombian Andes experienced a 1°C increase in air temperature.[24] In 1995, outbreaks of leptospirosis were associated with La Niña and El Niño phenomena—weather oscillations that climate change has intensified.[25] More recently, in 2010–2012, floods caused hundreds of deaths and displaced thousands.[26] Furthermore, the number of malaria cases has increased during the last five decades alongside increasing air temperatures.[27]
A view of Colombia’s health care profile puts into perspective the country’s capacity to address emerging climate-related health effects. Although the country introduced social welfare reforms aimed at expanding universal health coverage in the 1990s, the availability of health services is still limited for 29% of its population.[28] The number of nurses per 1,000 people and psychiatrists per 100,000 people remains below the Latin American average, and there is a large disparity between the lowest and highest income quintiles in accessing prenatal care.[29] Moreover, while there is limited research on health disparities along racial and ethnic lines, a few studies in Colombia consistently indicate a higher risk of stunting and wasting among children who self-identify as Indigenous or Afro-descendant.[30]
In conclusion, Brazil and Colombia both face serious and growing impacts on health, particularly among marginalized peoples and communities, due to climate change. At the same time, both countries currently have inadequate and unequal health care systems to meet present health needs.
The right to health and climate adaptation
In the context of the UNFCCC, in 2010, parties to the convention agreed to design national NAPs with the primary objective of reducing vulnerability to current effects and future climate change-related risks.[31] Since then, the World Health Organization (WHO) has issued three guidelines to assist in the development of the health component of such plans—namely, Guidance to Protect Health from Climate Change through Health Adaptation Planning (2014), Operational Framework for Building Climate Resilient Health Systems (2015), and, more recently, Quality Criteria for Health National Adaptation Plans (2021).[32] Though such documents help strengthen national health care systems and are comprehensive from a conventional public health perspective, including health care services, they fail to fully embrace an HRBA.[33]
Hence, a necessary point of departure for the present review is the significance of the human rights framework. Public health practitioners may wonder what the added value of human rights is for increasing countries’ adaptive capacity in health care. Drawing critical insights from recent Latin American perspectives on health sociology, this paper argues that even when both the human rights and the public health frameworks overlap in significant respects, there remain areas in which the former complements the latter.[34] Before elaborating on such a contention, this section offers a brief overview of the distinctive aspects of an HRBA to health.
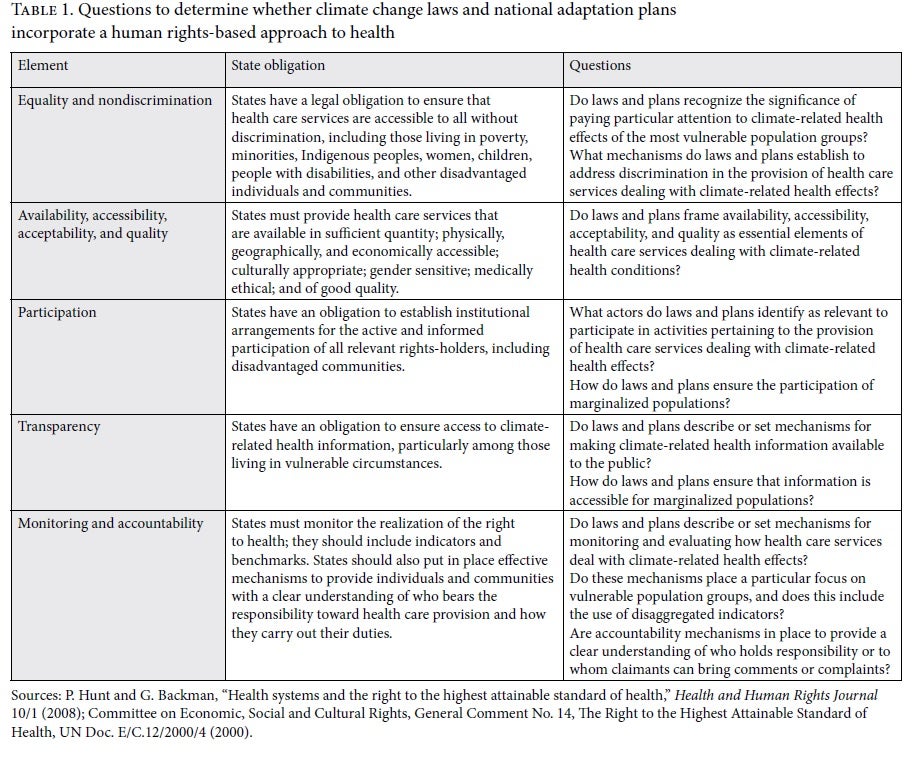
What does a human rights-based approach dictate in relation to health systems and health care provision? Although there is no universally agreed-upon definition of an HRBA to health, analysis of scholarship on the subject and guidance issued by WHO and the Office of the United Nations High Commissioner for Human Rights sheds light on the minimal conceptual and operational attributes of such an approach.[35] These attributes are (1) equality and nondiscrimination; (2) availability, accessibility, acceptability, and quality (AAAQ); (3) participation; (4) transparency; and (5) monitoring and accountability.[36]
The United Nations Committee on Economic, Social and Cultural Rights clarifies the content of these features in its General Comment 14. The equality and nondiscrimination element confers upon states the legal obligation to ensure that health care systems are accessible to all, particularly to disadvantaged individuals and communities.[37] The AAAQ framework calls for the functioning of health care facilities with respect to goods and services that are available in sufficient quantity; accessible physically, geographically, and economically; culturally appropriate; gender sensitive; medically ethical; and of good quality.[38] With regard to participation and transparency, states have an obligation to ensure the informed and active involvement of all relevant rights-holders—especially those living in vulnerable circumstances—and their access to health information. Finally, accountability includes the monitoring of conduct, performance, and outcomes.[39] This means having effective mechanisms to provide individuals and communities with a clear understanding of who bears responsibility toward health care provision and how they carry out their duties.[40] Also, monitoring should include indicators and benchmarks that can be used to assess progress.[41]
An HRBA to health and a public health approach to climate change overlap in significant ways. The former’s attribute of availability, economic accessibility (affordability), and quality resonates with the concept of “effectiveness” in the health literature.[42] Also, the monitoring and accountability aspect has been promoted by some of the WHO guidelines on health systems and climate change.[43] However, given that an HRBA focuses on the most vulnerable sections of the population, its attributes of equality and nondiscrimination, acceptability, participation, and transparency compel policy attention toward pervasive exclusionary practices that affect people’s health outcomes.[44] In other words, unlike the public health approach, an HRBA requires an analysis of the extent to which socioeconomic inequalities are taken into account in climate law and policy in order to redress discriminatory practices and unjust distributions of power.[45] This adds significant value to the organization and administration of health services in Latin America, which rely almost exclusively on a conventional epidemiological perspective and do not take into account the historical and sociocultural nature of health challenges.[46]
Furthermore, while public health approaches to climate change also commend equal access to quality health care as a determinant of countries’ adaptive capacity, the operationalization of such a view remains at the margins of current assessments of NAPs.[47] For example, WHO’s review of health in NAPs and the insights provided by indicator 2.1.1 of the Lancet Countdown on this subject do not look for discriminatory practices or the exclusion of the most marginalized communities in their assessments.[48]
In summary, the analytical layer that the HRBA adds to current assessments on public health responses to climate change makes a distinctive contribution. Particularly, given how Brazil’s and Colombia’s socioeconomic inequalities deeply affect their ability to cope with current climate-related health conditions, guiding adaptation efforts toward addressing persistent exclusion in health care and health care policy is a crucial step to avoid further human suffering and losses. An HRBA must therefore be explicitly invoked, starting with planning tools.[49]
Methodology
This paper applies a qualitative content analysis to identify whether Brazil’s and Colombia’s national climate change laws and H-NAPs incorporate an HRBA. More specifically, it uses a rubric of questions to derive the extent to which such laws and plans embrace the five minimal conceptual and operational attributes of an HRBA to health (as discussed in the previous section)—namely, equality and nondiscrimination, AAAQ, participation, transparency, and monitoring and accountability. Table 1 presents the questions applied to the analysis for each of these attributes. The formulation of the rubric was informed by previous work assessing an HRBA to health policies and programs, particularly that of Sofia Gruskin and Laura Ferguson, as well as a subsequent methodological proposition of Laura Ferguson.[50] The coding and data analysis was conducted using NVivo software.
The applied qualitative content analysis is constructive in epistemology; it seeks to be meaningful when applied in specific contexts rather than being universally applicable.[51] That is, even though the rubric of questions guides a systemic analysis of the attributes commonly considered to be part of an HRBA, it focuses more on description and does not provide generalizable findings.[52]
This study selected national climate change laws and NAPs as units of analysis, since they constitute the immediate and overarching regulatory and planning instruments that direct how climate adaptation on health ought to be conducted. At the same time, as mentioned above, these instruments have become the measure by which indicator 13.2.1 of the Sustainable Development Goals and indicator 2.1.1 of the 2020 Lancet Countdown report assess countries’ adaptation progress and health risks related to climate change.[53]
Nonetheless, this paper’s methodological approach has some limitations. First, the study does not include the regulatory framework for health care or disaster risk prevention and management, which may also deal with climate-related challenges to health. Further, its scope does not stretch beyond the planning level. In other words, the implementation of Brazil’s and Colombia’s national laws and plans falls outside the scope of this study.
The review
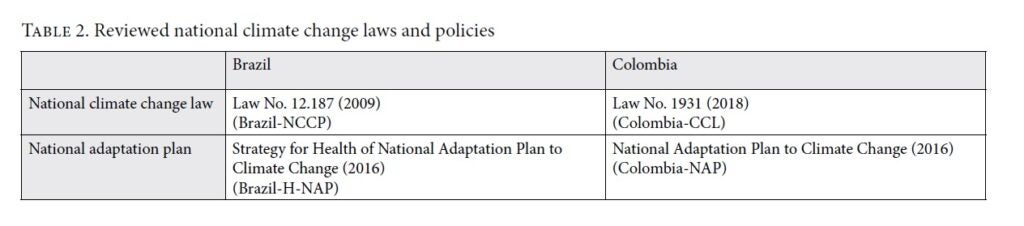
In December 2009, Brazil enacted Law No. 12.187, establishing the National Climate Change Policy (Brazil-NCCP), which provided the foundation for the country’s national adaptation plan (Brazil-NAP).[54] The Executive Group of the Inter-Ministerial Committee on Climate Change developed such a plan over three years (2013–2016) through a process that included contributions from thematic networks and public participation.[55] Brazil submitted its NAP to the UNFCCC NAP Central in May 2016.[56]
Brazil-NAP entails one general and eleven sectoral strategies, one of which pertains specifically to health (Brazil-H-NAP). Brazil-H-NAP is relevant to Brazil’s health care services, given that it provides inputs for the definition of objectives, goals, and actions of the country’s Unified Health System management model.[57]
Colombia adopted Law 1.931 on Climate Change (Colombia-CCL) in July 2018, after a two-year national consultation process convened by the Intersectoral Climate Change Commission.[58] This law sets the institutional and procedural arrangements for the design, implementation, and evaluation of mitigation and adaptation measures; it also creates the Intersectoral Climate Change Commission. Strikingly, while Colombia-CCL incorporates several ministries into this commission, it does not include its Ministry of Health (article 4 of the law). This is not a minor omission, considering that the commission is in charge of dictating the direction and content of climate change actions.
Colombia’s 2016 National Adaptation Plan (Colombia-NAP) constitutes the country’s overarching policy to reduce socioeconomic and environmental impacts from climate change.[59] The National Planning Department spearheaded its drafting based on the 2010–2014 and 2014–2018 National Development Plans. Colombia-NAP was submitted to the UNFCCC NAP Central in February 2018.[60]
The remainder of this section offers a detailed look at the findings on the aforementioned regulations. For clarity purposes, this paper organizes the analysis according to HRBA element. Table 2 outlines the reviewed laws and NAPs.
Equality and nondiscrimination
Brazil-NCCP does not explicitly refer to nondiscrimination. However, it recognizes particular population needs according to their socioeconomic contexts (article 3). Moreover, eradicating poverty and reducing social inequalities form part of its objectives (article 4).
Likewise, Brazil-H-NAP embraces equality and nondiscrimination partially. While guideline no. 6 sets forth a specific focus on vulnerable social groups, it confines such differentiated attention to rural areas, wetlands, forests, Indigenous peoples, and homeless people. Given that Brazil’s health disparities unfold beyond these spatial and group boundaries—as previous sections have noted—this guideline does little to summon efforts in all the directions required. Further, the plan does not set mechanisms to address discrimination in health care services.
Equality and nondiscrimination would be absent in Colombia-CCL if not for the law’s definition of “vulnerability.” By delineating this concept as the social and economic fragility to suffer adverse effects of climate change, article 3(19) opens an avenue within the law’s scope to provide particular attention to excluded populations and groups. Contrastingly, article 8(3) undermines the significance of supporting climate adaptation for all marginalized populations. By limiting adaptation programs, projects, and actions to coastal municipalities and districts, it takes critical focus away from the noncoastal territories, where poverty and exclusion are also everyday realities.[61]
Colombia-NAP explicitly mandates particular attention to vulnerable population groups: its objective no. 1 emphasizes the importance of following differentiated approaches that account for gender, age, and disability perspectives. However, the plan does not reiterate this specific objective across its objectives. Hence, unless bold interpretation efforts are applied, incorporating gender, age, and disability perspectives may not be central to actions arising from the plan’s objectives no. 2 and 3. Moreover, Colombia-NAP does not set explicit mechanisms to address discrimination in health care provision.
Availability, accessibility, acceptability, and quality
The AAAQ framework is absent from Brazil-NCCP. However, the country’s H-NAP calls for ensuring that public health care infrastructure is well suited to resist and operate in extreme weather conditions (guideline no. 5). In the same vein, it focuses on training and building capacity for health professionals on climate change-related issues (guideline no. 3). While these provisions touch on crucial quality aspects of health care systems, Brazil-H-NAP does not include courses of action to ensure availability, accessibility, or acceptability in health care services.
Likewise, Colombia-CCL does not refer to the AAAQ framework. Nonetheless, the country’s NAP embraces the health component of climate adaptation (objective no. 3). It underscores the importance of deploying coordinated action between the local, state, and national levels in epidemiological surveillance systems. Particularly, capacity-building among health professionals and community members is considered paramount to identifying and preventing health risks associated with climate change. Besides this provision, which refers to a crucial aspect for enhancing the quality of health care systems, the plan sets out no other consideration related to availability, accessibility, or acceptability.
Participation
Brazil-NCCP sets out public participation as one of its five principles (article 3). Article 4 states that the NCCP will aim to implement climate change adaptation with the participation and collaboration of, among others, those especially vulnerable to its adverse effects. Further, article 5 emphasizes the involvement of organized civil society in developing and implementing policies, plans, programs, and actions related to climate change.
In the same vein, Brazil-H-NAP encourages community participation in the formulation of adaptation policies (guideline no. 3). In particular, it promotes the strengthening of community involvement in deciding the priority of public health policies. Moreover, it calls for public participation in the integration of climate change and human health themes on the agenda of the Standing Committees for Health Surveillance, which further supports the response actions of health care networks (guideline no. 8). While the plan prompts participation across several activities pertaining to health care systems, in some of them, such engagement is limited to institutional actors, thereby limiting the opportunities of marginalized communities to be involved in decision-making. For example, guideline no. 8 encourages the involvement of “partner institutions” in preparing and implementing public health emergency plans; however, it gives no consideration to the inclusion of disadvantaged communities.
Colombia-CCL conceives of participation as a responsibility (article 2). In doing so, this law shifts the burden of engaging in climate action to civil society, as if participation were a matter of people’s mere willingness and personal choices. This clouds the fact that the state—as the sole human rights duty-bearer—holds the information, resources, and power necessary to promote participation. Thus, unless governments commit to making such tools available, civil society will not be able to take part in climate actions effectively.
Moreover, while Colombia-NAP refers to participation (objective no. 1), it does not place special emphasis on marginalized populations. As a result, the plan does not consider specific mechanisms to ensure the participation of these groups.
Transparency
Brazil-NCCP embraces the dissemination of information as one of the main principles upon which climate policies should be built (article 5). In the same way, Brazil-H-NAP emphasizes the provision of data and information to promote adaptation in the health sector (guideline no. 4). However, unlike the country’s climate law, Brazil-H-NAP further calls for the establishment of mechanisms to promote the informed and active involvement of vulnerable populations in policies aimed at increasing the resiliency of these groups (guideline no. 6).
Colombia-CCL creates a National Climate Change Information System, to which the law confers the mandate to provide transparent and timely data for decision-making processes related to climate change management (article 26). Nonetheless, because the law does not elaborate on how to ensure that such information is available and accessible to all populations, there remain some interpretative pathways that could eventually allow the system to limit certain information to decision-makers only. Likewise, while Colombia-NAP emphasizes the significance of transparent decision-making processes, it does not outline mechanisms to make information available to the most marginalized population groups.
Monitoring and accountability
Brazil-NCCP mandates monitoring as a climate policy instrument. However, this is limited to capturing meteorological data. The law does not address policy evaluation in terms of the performance or outcomes of health systems. To fill such a gap, Brazil-H-NAP handles monitoring to a greater extent. It covers various aspects, such as the quality of information (guideline no. 1), the importance of traditional knowledge (guideline no. 2), and multidimensional surveillance (guidelines no. 4 and 8).
Moreover, Brazil-NCCP identifies the institutions responsible for implementing the country’s national climate change policy—including adaptation (article 7). It also tasks public financial institutions with providing credit to support climate-related actions (article 8). Brazil-H-NAP also determines who is responsible for implementing each plan’s objectives; however, it falls short in specifying mechanisms whereby affected populations can raise their concerns.
Colombia-CCL embraces the monitoring and evaluation of adaptation outcomes as components of climate change management. Nonetheless, no provisions ensure that these processes focus on including marginalized populations or calling for collecting multidimensional data. However, Colombia-NAP mandates monitoring (1) vulnerability and climate risk indicators and (2) the outcomes of adaptation measures to reduce climate impacts on health. In this regard, the plan sets forth a methodological framework specifically tailored to the country’s circumstances and calls for related indicators. While these mechanisms do consider a particular focus on disadvantaged population groups, they do not consider the deployment of disaggregated indicators.
On the matter of accountability, both Colombia-CCL (article 6) and the country’s NAP define the agencies responsible for accomplishing the country’s adaptation goals. Yet neither of them outlines specific mechanisms before which complaints can be brought.
In brief, Brazil’s and Colombia’s climate change laws and NAPs incorporate an HRBA to varying degrees. While these regulations fall short in establishing mechanisms for advancing equality and nondiscrimination, participation, and transparency with a particular focus on marginalized populations, they include quality of health care services and monitoring to a greater extent. Table 3 summarizes these findings.
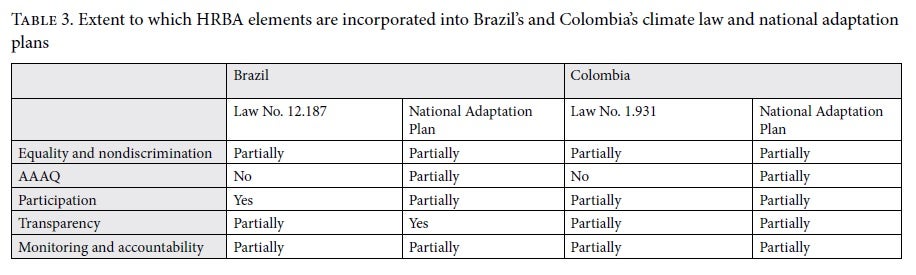
Discussion
The review of Brazil’s and Colombia’s national climate change laws and NAPs reveals varying levels of engagement with an HRBA. In the case of laws, although both countries had legally recognized the right to health before joining the UNFCCC, the absence of explicit references to the key attributes of this right exemplifies the disconnect between international human rights law and international climate change law.[62]
The practical implications of such a weak integration should not be disregarded. Leaving human rights out of national climate change laws and NAPs has a large impact on the most vulnerable communities. Unless the key attributes of the HRBA to health are acknowledged and incorporated, it cannot be assumed that the actions directed by the laws will improve the realization of the right to health.[63] As former Special Rapporteur on the right to health Paul Hunt notes in his interpretative analysis of the right to health and the rights-based approach to health, “it is unrealistic to expect health policy makers or practitioners to read either a treaty provision or its corresponding general comment and then grasp how they are to operationalize the right to health.”[64] He argues that “a more detailed, specific, and practical human rights guidance is essential.”[65] References to an HRBA in the law are therefore crucial to facilitate legal interpretations that address discriminatory practices and existing and interlocking inequalities that hinder the ability of health care systems to cope with climate change.
While this paper has identified some interpretative pathways through which human rights elements can be inferred from the national climate change laws, it has also underscored the avenues in which the lack of their explicit reference can translate into weak attention toward marginalized communities. For example, full integration of the equality and nondiscrimination principles in Brazil-NCCP would provide a legal basis for pressuring decision-makers to address health disparities experienced by communities of color resulting from climate change. Furthermore, the fact that Brazil-H-NAP and Colombia-NAP pay no attention to the availability, accessibility, or acceptability elements of health care limits opportunities to prepare health care systems for a changing climate.
At the same time, however, this review has also laid bare how some of the attributes of the HRBA are taken on by Brazil’s and Colombia’s NAPs, such as in the case of monitoring.
Although these findings may seem to support the conclusion of the United Nations Economic Commission for Latin America and the Caribbean (ECLAC) that “most countries of the region of Latin America and the Caribbean have incorporated international human rights standards into their climate change policies and strategic planning,” they are divergent in a fundamental way.[66] Specifically, by highlighting how the rights-based attributes identified in Brazil’s and Colombia’s NAPs support the preparation of health care systems to withstand climate change, this review points to the specific areas in which the approach ought to be reinforced. That is, unlike ECLAC’s contention, the analysis drawn posits that both countries’ adaptation plans still hold considerable room for improving their engagement with the human rights framework, particularly with respect to their health care systems. For example, even though Colombia’s NAP refers to participation, transparency, and monitoring, it does not establish mechanisms through which these elements can integrate marginalized populations.
The way forward
By providing an in-depth review of the extent to which Brazil’s and Colombia’s national climate change laws and NAPs incorporate an HRBA to health, this paper has broadened the analytical perspectives by which countries’ progress in adapting health care systems to accommodate climate change are currently assessed. From this view, simply counting the number of countries with a climate change adaptation plan, as a primary proxy for how well they are integrating climate change measures into health policy, is insufficient.
Furthermore, unlike similar studies on the mainstreaming of human rights in climate change legislation and policies, this review has indicated that more specific regulations are needed to promote health care systems that can respond to climate change. Because this appears to be the first review of the intersection between human rights, climate change adaptation, and health care in NAPs, further research is required to understand how rights-based approaches can facilitate the strengthening of health care systems at subnational levels. Analyses of these regulations’ interactions with specific health care systems and disaster risk prevention and management laws is also a key research gap.
Climate change laws and NAPs are the basis for translating planning into action. Thus, if health care systems are to contribute to the realization of the right to health in a changing climate, these regulations ought to provide a clear substantive and operational basis to reduce marginalized populations’ vulnerability to climate change. An HRBA can ensure that these groups are protected.
Acknowledgments
I am very grateful to my former academic advisor, Professor Gillian MacNaughton, for her encouragement and support and to Dr. José Luis Viveros Dorantes for his insights on the public health approach to climate change. I also express my deepest appreciation to the editors and reviewers, whose insightful comments helped me improve the paper. The views and any mistakes are my responsibility.
Thalia Viveros-Uehara, MSc, is a PhD student at the School for Global Inclusion and Social Development at the University of Massachusetts Boston, USA.
Please address correspondence to the author. Email: t.viverosuehara001@umb.edu
Competing interests: None declared.
Copyright © 2021 Viveros-Uehara. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
[1] G. O. Magrin, C. Gay García, D. Cruz Choque, et al., “Latin America,” in M. L. Parry, O. F. Canziani, J. P. Palutikof, et al. (eds), Climate change 2007: Impacts, adaptation and vulnerability; Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change (Cambridge: Cambridge University Press, 2007), p. 599; G. O. Magrin, J. A. Marengo, J.-P. Buolanger, et al., “Central and South America,” in V. R. Barros, C. B. Field, D. J. Dokken et al. (eds), Climate change 2014: Impacts, adaptation, and vulnerability; Part B: Regional aspects; Contribution of Working Group II to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change (Cambridge: Cambridge University Press, 2014), p. 1535; N. Watts, M. Amann, N. Arnell, et al., “The 2020 report of the Lancet Countdown on health and climate change: Responding to converging crises,” Lancet 397 (2021), pp. 129–170.
[2] Office of the United Nations High Commissioner for Human Rights, Analytical Study on the Relationship between Climate Change and the Human Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health, UN Doc. A/HRC/32/23 (2016).
[3] L. Parry, C. Radel, S. B. Adamo, et al., “The (in)visible health risks of climate change,” Social Science and Medicine 241 (2019)
[4] L. Manderson, J. Aagaard-Hansen, P. Allotey, et al., “Social research on neglected diseases of poverty: Continuing and emerging themes,” PLOS Neglected Tropical Diseases 3/2 (2009), p. e332; GBD 2016 Healthcare Access and Quality Collaborators, “Measuring performance on the healthcare access and quality index for 195 countries and territories and selected subnational locations: A systematic analysis from the global burden of disease study 2016,” Lancet 391/10136 (2018), pp. 2236–2271.
[5] A. Grambsch and B. Menne, “Adaptation and adaptive capacity in the public health context,” in A. J. McMichael, D. H. Campbell-Lendrum, C. F. Corvalán, et al. (eds), Climate change and human health: Risks and responses (Geneva: World Health Organization, 2003), p. 220–221.
[6] Office of the United Nations High Commissioner for Human Rights (see note 2), para. 57.
[7] Ibid., para. 11; S. Hamerling, “Climate change impacts: Human rights in climate adaptation and loss and damage,” in S. Duyck, S. Jodoin, and A. Johl (eds), Routledge handbook of human rights and climate governance (New York: Routledge, 2018), p. 97.
[8] K. L. Ebi and E. Villalobos Prats, “Health in national climate change adaptation planning,” Annals of Global Health 81/3 (2015), pp. 418–426.
[9] P. Hunt and G. MacNaughton, “Impact assessments, poverty and human rights: A case study using the right to the highest attainable standard of health” (submitted to UNESCO, May 2006). Available at http://repository.essex.ac.uk/9784/1/impact-assessments-poverty-human-rights-report.pdf; L. Ferguson, “Assessing work at the intersection of health and human rights: Why, how and who?,” in B. A. Adreassen, H. Sano, and S. McInerney-Lankford (eds), Research methods in human rights (Cheltenham: Edward Elgar Publishing, 2017), pp. 417–418.
[10] A. Sy, “Socio/ethno-epidemiologies: Proposals and possibilities from the Latin American production,” in F. G. De Maio, I. Llovet, and G. Dinardi (eds), Latin American perspectives on the sociology of health and illness (New York: Routledge, 2019), p. 75.
[11] United Nations General Assembly, Work of the Statistical Commission pertaining to the 2030 Agenda for Sustainable Development, UN Doc. A/RES/71/313 (2017), goal 13; Watts et al. (see note 1), p. 144.
[12] “Climate change impacts, exposures and vulnerability,” Lancet Countdown (2019). Available at https://www.lancetcountdown.org/data-platform/climate-change-impacts-exposures-and-vulnerability; United Nations Human Rights Treaty Bodies, Ratification status for CESCR–International Covenant on Economic, Social and Cultural Rights (2021). Available at https://tbinternet.ohchr.org/_layouts/15/TreatyBodyExternal/Treaty.aspx; Department of International Law of the Organization of American States, Signatories and ratifications, Additional Protocol to the American Convention on Human Rights in the Area of Economic, Social, and Cultural Rights “Protocol of San Salvador” (2021). Available at https://www.oas.org/juridico/english/sigs/a-52.html.
[13] Magrin et al. (2014, see note 1), pp. 1506–1536.
[14] República de Colombia, Tercera comunicación nacional de Colombia a la Convención Marco de las Naciones Unidas sobre el Cambio Climático (Colombia: IDEAM, PNUD, MADS, DND, Cancillería, FMAM, 2017), pp. 25–28; “Climate change impacts, exposures and vulnerability” (see note 12); Parry et al. (2019, see note 3); Federative Republic of Brazil, Fourth national communication of Brazil to the United Nations Framework Convention on Climate Change (Brazil: Ministry of Science, Technology and Innovation, 2020), pp. 194–208. Available at https://unfccc.int/sites/default/files/resource/4a%20Comunicacao%20Nacional.pdf.
[15] Magrin et al. (2014, see note 1), p. 1506.
[16] Ibid., p. 1507.
[17] A. R. Moreno, “Climate change and human health in Latin America: Drivers, effects, and policies,” Regional Environmental Change 6/3 (2006), pp. 157–164.
[18] Ibid.
[19] M. Scheffer, Demografia médica no Brasil (São Paulo: Departamento de Medicina Preventiva, Faculdade de Medicina da USP, Conselho Regional de Medicina do Estado de São Paulo, Conselho Federal de Medicina, 2015), pp. 56–57. Available at http://www.usp.br/agen/wp-content/uploads/DemografiaMedica30nov2015.pdf.
[20] F. R. Martins-Melo, A. N. Ramos Jr., C. H. Alencar, et al., “Trends and spatial patterns of mortality related to neglected tropical diseases in Brazil,” Parasite Epidemiology and Control 1 (2016), pp. 56–65; D. H. Molyneux, L. Savioli, and D. Engels, “Neglected tropical diseases: Progress towards addressing the chronic pandemic,” Lancet 389/10066 (2017), p. 321.
[21] Scheffer (see note 19), pp. 153–157.
[22] L. Parry, B. Day, S. Amaral, et al., “Drivers of rural exodus from Amazonian headwaters,” Population and Environment 32 (2010), pp. 137–176.
[23] República de Colombia (see note 14), p. 91
[24] Magrin et al. (2014, see note 1), p. 1507; B. Wang, X. Luo, Y. Yang, et al., “Historical change of El Niño properties sheds light on future changes of extreme El Niño,” Proceedings of the National Academy of Sciences 116/45 (2019) pp. 22512–22517.
[25] Moreno (2006, see note 17), p. 160.
[26] Magrin et al. (2014, see note 1), p. 1535.
[27] Ibid.
[28] R. Atun, L. O. Monteiro de Andrade, G. Almeida, et al., “Health-system reform and universal health coverage in Latin America,” Lancet 385/9974 (2015) p. 1232.
[29] OECD and World Bank, Health at a glance: Latin America and the Caribbean 2020 (Paris: OECD Publishing, 2020), pp. 23–32.
[30] L. Mena-Meléndez, “Ethnoracial child health inequalities in Latin America: Multilevel evidence from Bolivia, Colombia, Guatemala, and Peru,” SSM – Population Health 12 (2020), p. 7
[31] Hamerling (see note 7), p. 97.
[32] World Health Organization, WHO guidance to protect health from climate change through health adaptation planning (Geneva: WHO, 2014); World Health Organization, Operational framework for building climate resilient health systems (Geneva: WHO, 2015); World Health Organization, Quality criteria for health national adaptation plans (Geneva: WHO, 2021).
[33] Hamerling (see note 7), p. 97.
[34] F. G. De Maio, I. Llovet, and G. Dinardi, Latin American perspectives on the sociology of health and illness (New York: Routledge, 2019), pp. 1–127.
[35] P. Hunt, “Interpreting the international right to health in a human rights-based approach to health,” Health and Human Rights Journal 18/2 (2016), pp. 109–130.
[36] P. Hunt and G. Backman, “Health systems and the right to the highest attainable standard of health,” Health and Human Rights Journal 10/1 (2008), p. 87; S. Gruskin, D. Bogecho, and L. Ferguson, “Rights-based approaches to health policies and programmes: Articulations, ambiguities and assessment,” Journal of Public Health Policy 31 (2010), pp. 138–139.
[37] Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4 (2000).
[38] Ibid.; P. A. Villarreal, “El derecho a la salud en lo individual y en lo colectivo: la calidad en los servicios de salud a partir de Poblete Vilches vs. Chile,” in M. Morales Antoniazzi and L. Clérico (eds), Interamericanización del derecho a la salud (Querétaro: Instituto de Estudios Constitucionales del Estado de Querétaro, 2019), pp. 291–292.
[39] Hunt and Backman (see note 36), p. 83.
[40] Ibid., p. 89–90.
[41] Committee on Economic, Social and Cultural Rights (see note 37), para. 43(f).
[42] M. Lindelow, S. Nahrgang, T. Dmytraczenko, et al., “Assessing progress toward universal health coverage: Beyond utilization and financial protection,” in T. Dmytraczenko and G. Almeida (eds), Toward universal health coverage and equity in Latin America and the Caribbean (Washington, DC: World Bank, 2015), p. 151.
[43] World Health Organization (2015 and 2021, see note 32).
[44] Office of the United Nations High Commissioner for Human Rights (see note 2), paras. 46–52; Gruskin et al. (see note 36), pp. 130–134.
[45] Office of the United Nations High Commissioner for Human Rights (see note 2).
[46] Sy (see note 10), p. 75.
[47] Grambsch and Menne (see note 5), pp. 230–231.
[48] World Health Organization (2021, see note 32), pp. 1–16; Watts et al. (see note 1), p. 144.
[49] Ferguson (see note 9).
[50] Ibid., pp. 416–418; Gruskin et al. (see note 36), pp. 129–145.
[51] J. W. Drisko and T. Maschi, Content analysis (New York: Oxford University Press, 2016), pp. 81–120.
[52] Ibid.
[53] United Nations General Assembly (see note 11); Watts et al. (see note 1), p. 144.
[54] Lei No. 12.187, de 29 de Dezembro de 2009 (2009). Available at http://www.planalto.gov.br/ccivil_03/_ato2007-2010/2009/lei/l12187.htm.
[55] Brazil Ministry of Environment, National adaptation plan to climate change: Volume I general strategy (Brasilia: Ministry of Environment, 2016), p. 6. Available at https://www4.unfccc.int/sites/NAPC/Documents/Parties/Brazil%20NAP%20English.pdf.
[56] “National adaptation plans,” UNFCCC NAP Central (August 2021). Available at https://www4.unfccc.int/sites/NAPC/Pages/national-adaptation-plans.aspx.
[57] Brazil Ministry of Environment, National adaptation plan to climate change: Volume II sectoral and thematic strategies (Brasilia: Ministry of Environment, 2016), p. 176. Available at https://www4.unfccc.int/sites/NAPC/Documents/Parties/English_PNA_Part2%20v4.pdf.
[58] Ministerio de Ambiente y Desarrollo Sostenible, Ley de Cambio Climático (February 2021). Available at https://www.minambiente.gov.co/index.php/ley-de-cambio-climatico; Congreso de Colombia, Ley No. 1931 del 27 de julio de 2018 por la cual se establecen directrices para la gestión del cambio climático (2018). Available at https://www.minambiente.gov.co/index.php/ley-de-cambio-climatico.
[59] Departamento Nacional de Planeación, Plan nacional de adaptación al cambio climático (Bogotá: Departamento Nacional de Planeación, 2016). Available at https://www4.unfccc.int/sites/NAPC/Documents/Parties/Colombia%20NAP%20Spanish.pdf.
[60] “National adaptation plans,” UNFCCC NAP Central (August 2021). Available at https://www4.unfccc.int/sites/NAPC/Pages/national-adaptation-plans.aspx.
[61] D. E. Cuartas and F. Méndez, “Cambio climático y salud: Retos para Colombia,” Revista de La Universidad Industrial de Santander 48/4 (2016), pp. 428–435.
[62] A. L. Phelan, “The environment, a changing climate and planetary health,” in L. O. Gostin and B. Mason Meier (eds), Foundations of global health and human rights (New York: Oxford University Press, 2020) p. 421–422.
[63] Ferguson (see note 9).
[64] Hunt (see note 35), p. 116.
[65] Ibid.
[66] United Nations Economic Commission for Latin America and the Caribbean, Climate change and human rights: Contributions by and for Latin America and the Caribbean (Santiago: United Nations, 2019), p. 68.
