Volume 23/2, December 2021, pp. 173-186 | PDF
Sophia A. Zweig,* Alexander J. Zapf,* Chris Beyrer, Debarati Guha-Sapir, and Rohini J. Haar
Abstract
In response to the COVID-19 pandemic, governments around the world have implemented public health policies that limit individual freedoms in order to control disease transmission. While such limitations on liberties are sometimes necessary for pandemic control, many of these policies have been overly broad or have neglected to consider the costs for populations already susceptible to human rights violations. Furthermore, the pandemic has exacerbated preexisting inequities based on health care access, poverty, racial injustice, refugee crises, and lack of education. The worsening of such human rights violations increases the need to utilize a human rights approach in the response to COVID-19. This paper provides a global overview of COVID-19 public health policy interventions implemented from January 1 to June 30, 2020, and identifies their impacts on the human rights of marginalized populations. We find that over 70% of these public health policies negatively affect human rights in at least one way or for at least one population. We recommend that policy makers take a human rights approach to COVID-19 pandemic control by designing public health policies focused on the most marginalized groups in society. Doing so would allow for a more equitable, realistic, and sustainable pandemic response that is centered on the needs of those at highest risk of COVID-19 and human rights violations.
Introduction
The global response to public health emergencies, such as pandemics, often requires enacting public health policy interventions to prevent disease and protect population health. These interventions can and do limit individual freedoms and are widely understood to be appropriate in public health emergencies. The COVID-19 pandemic has prompted the implementation of public health measures at an unprecedented global scale. Policies such as border and school closures, face mask mandates, limitations on social gatherings, and household confinement have been shown to be effective against COVID-19 transmission and disease outcomes.[1] While such interventions are crucial to pandemic mitigation, their public health benefits can result in substantial trade-offs, such as limited access to medical care and public health services for the diagnosis, treatment, and prevention of other diseases, as well as the loss of livelihood and disruptions to education and sociocultural interaction.[2] Furthermore, public health interventions can also come at human rights costs, disproportionately impacting already vulnerable and oppressed communities.[3]
International guidance on the rights-limiting measures allowable during states of emergency is based on the Siracusa Principles.[4] These principles state that regardless of the nature or severity of the emergency, restrictions on human rights must meet standards of legality, legitimacy, necessity, proportionality, evidence, and nondiscrimination.[5] General Comment 14 to the International Covenant on Economic, Social, and Cultural Rights (ICESCR) further emphasizes that states have “the burden of justifying such serious measures” with respect to “demonstrat[ing] that restrictive measures are necessary to curb the spread of infectious diseases so as to ultimately promote the rights and freedoms of individuals.”[6] However, the implementation of these guiding principles can be intricate given that derogations of human rights standards are multifaceted and may be complicated by complex interactions between competing aspects of public health, ethics, economics, and law.[7] Further, there are no international principles or standards for state of emergency declarations, meaning that states are bound solely to national and local public health laws when making these declarations. Therefore, public health interventions can and have been practiced discriminatorily by restricting the social, economic, and cultural rights of specific populations, such as refugees and migrants, who are particularly vulnerable to movement restrictions.[8]
Blanket public health policies can be particularly challenging for disadvantaged populations. For example, people living in impoverished and densely populated urban housing or confined to refugee camps cannot realistically quarantine or avoid gatherings.[9] Incarcerated persons do not have the capability to follow sanitation and masking guidelines without the support of prison policy and resources, and the nature of correctional facilities is not suited to social distancing.[10] Hourly workers and day workers may not be able to afford food, medicine, or other necessities of life when COVID-19 restrictions impair their travel to work. Viewed through a human rights lens, public health interventions are designed to protect the most vulnerable members of society but in practice, the result may be the opposite. Furthermore, policies can be designed ostensibly for pandemic control while their true goal is political—for example, by limiting assemblies and thereby suppressing anti-government demonstrations. Evaluating COVID-19 public health interventions around the needs of vulnerable populations and prioritizing their needs may allow for a pandemic response that is not only more equitable but also more practicable and sustainable for those at highest risk of disease transmission, morbidity, and mortality.[11] To address these concerns, we provide a global overview of public health interventions implemented during the COVID-19 pandemic and analyze their human rights dimensions.
Methods
Defining populations vulnerable to human rights abuses
To examine COVID-19 public health interventions within a human rights framework, we must first define groups vulnerable to human rights abuses. The Committee on Economic, Social and Cultural Rights notes that state parties to the ICESCR are obliged to “give special attention to those individuals and groups who traditionally face difficulties in exercising this right” in the context of social security and human rights.[12] We based our analysis of vulnerable groups on the ICESCR definition and added additional groups that may be relevant to the COVID-19 pandemic based on US research ethics standards.[13] Table 1 outlines the major groups used in our analysis.
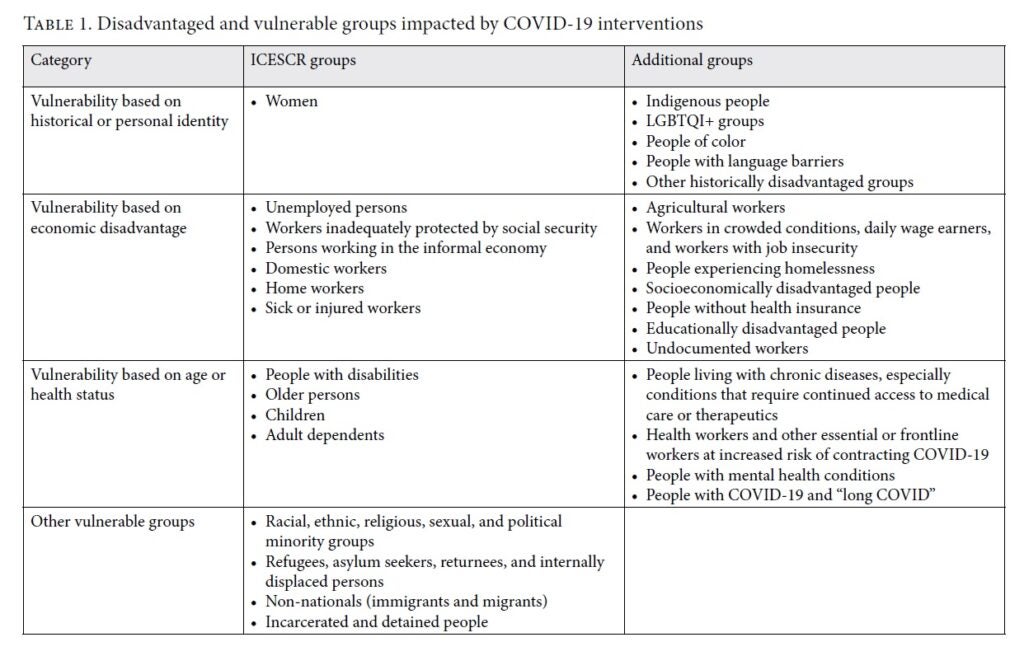
Database for public health interventions and applied human rights norms
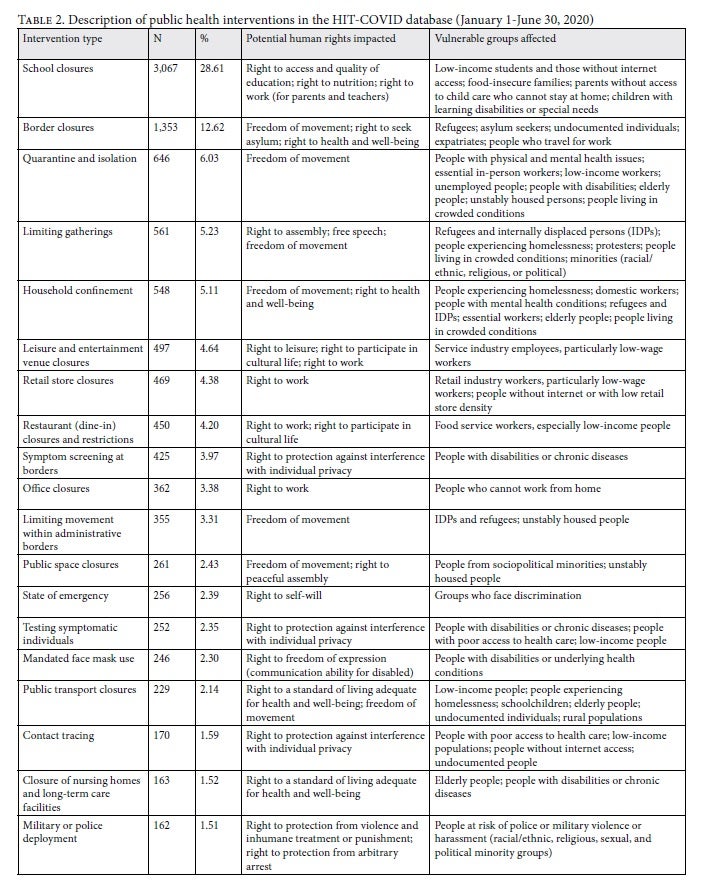
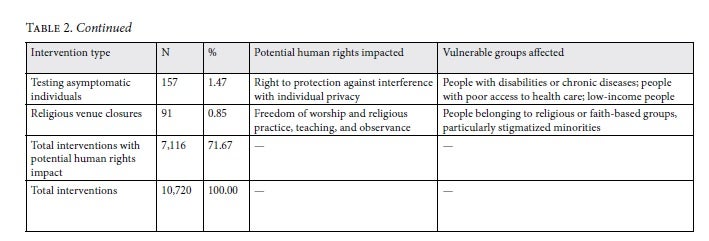
To categorize the key types of public health interventions that were implemented in the first six months of the COVID-19 pandemic (January 1 to June 30, 2020), we utilized curated data on global public health interventions from the free, open-access Health Intervention Tracking for COVID-19 (HIT-COVID) database.[14] Established in April 2020, the HIT-COVID database catalogues the implementation and relaxation of COVID-19 public health interventions at the national and subnational level, with geographic granularity down to the local level (cities and towns) where applicable. Within the available data for this period, 59% of the records were for the subnational level. The time frame from January 1 to June 30, 2020, was chosen because database entries during this period provided the most complete coverage and were therefore considered to yield more robust findings. As of March 31, 2021, there were 13,429 public health interventions catalogued in the database, of which 10,720 were implemented from January 1 to June 30, 2020. We abstracted these 10,720 public health interventions into 21 categories that the database had assigned a priori, based on the most common and relevant COVID-19 interventions. Then, we tabulated the absolute and relative frequency of public health interventions within these categories (Table 2). Notably, due to the time frame underlying our data extraction, more recent issues such as vaccine inequities, emerging COVID-19 variants, and global health disparities were not analyzed here.
Guided by the standards set forth in the Universal Declaration of Human Rights (UDHR), we cross-compared the 21 intervention categories by their potential human rights impacts. For each intervention category, we also identified the population groups most likely to be impacted from a human rights perspective, identifying groups that were most vulnerable to human rights abuses in such categories (Table 2).
Results
The most common public health interventions implemented in the first six months of the pandemic: School closures, border closures, and movement restrictions
Of the 10,720 public health interventions recorded during the first six months of the pandemic in the HIT-COVID database, the majority (71.67%) were identified as restricting human rights in at least one way or for at least one population (Table 2). Among all 21 public health intervention categories in the database, the five most prevalent categories covered 57.60% of interventions. These five categories were school closures (28.61%), border closures (12.62%), quarantine and isolation (6.03%), limiting gathering size (5.23%), and household confinement (5.11%). School closures refer to limited hours or days at school, the utilization of online learning, and universal school closure. Border closures refer to the closing of borders to other countries or subnational units, including restrictions imposed on certain subpopulations (based on geographic origin or on COVID-19 exposure or test results). Quarantine refers to the separation and restriction of movement for individuals who have had potential COVID-19 exposure or who have not had a confirmed infection (such as travelers and persons in contact with confirmed or suspected cases). Home isolation refers to people who are symptomatic or have a confirmed infection (such as symptomatic suspected cases, non-hospitalized confirmed cases, and cases discharged from the hospital). Limiting gatherings refers to the imposition of size limits on indoor and outdoor gatherings. Household confinement refers to curfews, stay-at-home orders, and lockdowns that require people to stay within their household except for essential trips (for example, for medical care or food). These orders may also restrict the movement of high-risk groups, such as elderly or chronically ill people.
Human rights dimensions most frequently impacted by public health interventions
All of the 21 public health intervention categories have impacts on human rights. The most common human right that is impacted by these interventions is freedom of movement, which is affected by border closures, household confinement, public space and public transport closures, and quarantine and isolation. While limiting movement is aimed at reducing contact rates between infected and susceptible persons to control community transmission, medically and socially vulnerable populations are disproportionately affected by such restrictions. For example, elderly people and individuals with underlying medical conditions may experience reduced access to health care and essential therapeutics, which in turn can result in delayed detection and prevention or treatment of diseases.
Other human rights that are frequently impacted by public health interventions include the right to protection against interference with individual privacy and the right to peaceful assembly. The curtailment of these rights has often resulted in resistance and protest among affected populations globally.[15]
Nonetheless, it is important to emphasize that due to country-level variations in government structures and human rights standards, the impact of these public health interventions differs by country. For example, restrictions on the freedom of movement may be more accepted and realistic in countries with better internet coverage and digital infrastructure, which enables the continuity of work from home; and acceptance of interference with individual privacy to protect the health of others may be higher among societies that culturally value collective action and solidarity.
Case studies from around the globe to explore the human rights impacts of COVID-19 restrictions
Below, we review the five most frequent types of interventions in order to understand the range of restrictions enacted, the potential human rights concerns around these restrictions, and their potential sequelae, particularly for vulnerable groups.
School closures
School closures made up more than one-fourth of all public health interventions in the HIT-COVID database that were implemented from January to June 2020. The right to an accessible and affordable education is protected under article 26 of the UDHR.[16] Epidemiologically, in-person school settings were initially considered a high-risk environment for the spread of COVID-19, but updated data analyses consider them a lower-risk environment regarding for transmission, especially at the elementary school level.[17] School closures have profound consequences for students’ learning, social well-being, and mental health, as well as the ability of parents to work.[18] While various governments have provided virtual education due to in-person school closures, it is not feasible to guarantee quality education or equal access to virtual learning during the pandemic due to inequities in resources (such as internet access) and in parents’ availability to supervise children adequately.[19] Many of these inequities were preexisting and were exacerbated during the pandemic. Thus, this disruption of learning inevitably results in substantial educational gaps for children across the world. The effects of educational gaps have been shown, both historically and currently, to negatively impact learning and life outcomes. A mere three-month school closure could reduce students’ long-term learning by a year, as suggested by modeling simulations.[20] School disruption during World War II was found to be associated with significant income loss 30 years later in life.[21]
School closures also lead to increased prevalence and exacerbation of mental health issues, such as anxiety and depression, among students.[22] School closures place vulnerable children at higher risk of food insecurity, and in many low- and middle-income countries, lack of access to education puts girls in particular at increased risk of child marriage, gender-based violence, sexual assault, and teen pregnancy. For example, the rate of child marriage in Malawi increased by 83% from March to May of 2020 compared to 2019, and the rate of sexual assault, which is linked to child marriage, increased by 151%.[23] Given that child brides are more likely to drop out of school and face gender-based violence, protecting access to education, particularly for girls, should be an imperative in the COVID-19 response, especially in low- and middle-income countries.[24]
Border closures
Border closures and movement restrictions are in tension with article 13 of the UDHR, which states that “everyone has the right to freedom of movement and residence within the borders of each state.”[25] Further, the International Health Regulations specifically state that public health interventions should be implemented “to prevent, protect against, control and provide a public health response to the international spread of disease in ways that are commensurate with and restricted to public health risks, and which avoid unnecessary interference with international traffic and trade.”[26] Even though border closures and movement restrictions were almost universally implemented by governments early in the pandemic, their effectiveness in reducing COVID-19 transmission is disputed, as it remains methodologically complex to distinguish the independent impact of individual interventions that have been implemented at the same point in space and time.[27] While border closures may be effective in delaying the spread of COVID-19, if implemented prior to establishment of community transmission within a country, their overall effect on transmission of COVID-19 is modest and not sustainable.[28]
For country or territory borders that are fraught or politically unstable, changes to border policies can have drastic consequences. For example, in the United States, border entry for immigrants and asylum seekers has been severely restricted. In response to COVID-19, many legal immigration proceedings were halted, leaving thousands in detention camps, where they are extremely vulnerable to contracting COVID-19 due to crowded living conditions, poor ventilation, and other inhumane treatment.[29] As of July 9, 2020, the cumulative test positivity rate among ICE detainees was 22.7%.[30] However, an independent investigation by the Vera Institute of Justice indicated that COVID-19 testing at ICE facilities was too limited to capture the actual number of cases and that the real number may have been much higher.[31] Furthermore, communication records indicate that some ICE officials ignored COVID-19 safety recommendations. For example, in one San Diego detention facility, testing guidelines were ignored, detainees did not receive face masks for weeks, and detainees were required to sign a waiver “saying that it wasn’t our fault if we got sick,” according to one detainee.[32] Due to the decentralized oversight of ICE facilities, many of which are under private ownership, the COVID-19 response has been slow moving and uncoordinated, putting detainees at high risk for contracting the virus.[33]
Quarantine and isolation
Quarantine and isolation are ancient but effective public health mitigation measures dating back to medieval Europe, when incoming ships were quarantined to prevent plague transmission.[34] Today, quarantine and isolation are regarded as necessary but not sufficient outbreak prevention strategies, as they require additional actions such as contact tracing.[35] Despite the importance of such measures in pandemic response, they may erode human rights, especially for marginalized populations such as detained people, refugees, immigrants, women, and children.[36] Thus, governments should consider their human rights impacts, particularly with regard to the right to safe shelter, the right to protection from violence, and the right to medical treatment, testing, and mental health services.[37] Further, these measures should not extend beyond the required minimum time period based on the incubation period of the virus.[38]
Quarantine and isolation policies during the COVID-19 pandemic have had negative consequences for vulnerable populations such as children because they increase the risk of abuse and neglect.[39] These policies can also have adverse effects on mental health that may last for years, and both social isolation and poor mental health are risk factors for violence.[40] Quarantine and isolation also increase the risk of domestic violence by increasing daily proximity to perpetrators of violence under stressful conditions.[41]
However, some policy makers have utilized quarantine and isolation orders as an opportunity to provide safe housing and health protection for vulnerable populations who are unable to isolate or quarantine. For example, New York City and Baltimore have hotel quarantine and isolation programs for COVID-19 positive or suspected positive patients who cannot otherwise isolate due to housing instability or crowding. Both programs are offered at no cost and include free meals, and the Baltimore program offers assistance to undocumented individuals.[42]
Limiting gatherings
Article 20 of the UDHR declares the right to freedom of peaceful assembly and association to be fundamental.[43] Limiting gatherings is a crucial public health intervention to contain transmission of COVID-19, especially for preventing “superspreader” events.[44] However, limitations on gatherings can easily be used to restrict the fundamental right to protest, and some governments have utilized the banning of gatherings to suppress political protesters. For example, in Algeria, all forms of street protests were banned in March 2020, ending a year of mass anti-government demonstrations by the Hirak movement, although protests reemerged in February 2021.[45]
Limiting gatherings is also unfeasible for people living in crowded areas, including people experiencing homelessness, residents of slums, and refugees housed in camps. For such populations, it is unrealistic to avoid gatherings when crowding is an integral part of unstable housing conditions.[46] Unstably housed populations are often already at higher risk of COVID-19 due to systemic inequities such as poverty, lack of health care access, unemployment, preexisting health conditions, and unsanitary living conditions. For example, Dharavi, India’s largest slum, is one of the most densely populated areas of the world, with an area of 2.1 square kilometers and about one million residents. Crowded housing and limited sanitation mean that residents share both private and public spaces. Under these conditions, it is impossible for Dharavi residents to avoid gatherings, close contact, and crowding, which increases their risk of COVID-19 transmission.[47] By implicitly violating these restrictions, people in these communities may face stigma or judgment and, in turn, avoid seeking health care services when ill. While limiting gatherings has a clear public health justification, there are circumstances where blanket restrictions can repress vital freedoms and harm health.
Household confinement
Article 13 of the UDHR states that people have the right to freedom of movement.[48] Household confinement policies such as curfews, lockdowns, and stay-at-home orders are a significant component of the public health response to COVID-19 because they aim to protect individuals from exposure and transmission. Such policies often aim to shield medically vulnerable populations, such as elderly persons and pregnant people. Various studies have found associations between household confinement policies and decreased COVID-19 transmission and mortality.[49] However, household confinement also inherently restricts the right to freedom of movement. Household confinement policies are dangerous and potentially deadly for those facing unsafe conditions at home, such as violence and abuse.[50] Additionally, adherence to home isolation orders is difficult, perhaps impossible, for housing-insecure people such as residents of slums, people living in refugee camps, and people experiencing homelessness. Many groups already facing housing insecurity have experienced the exacerbation of human rights threats during the COVID-19 pandemic.
When household confinement orders are followed, individuals are at risk of social isolation, poor mental health outcomes, and limited access to necessities such as food, supplies, and health care.[51] To address these issues, in China, medically vulnerable populations such as elderly persons have increasingly turned to technology and mobile apps for essential services such as home delivery of food and supplies.[52]
In other cases, the enforcement of household confinement measures can be a dangerous excuse for military and police personnel to use violence and corruption. For example, during the first 10 days of Kenya’s curfew, excessive police force resulted in the deaths of at least six people and injuries to many others. The dusk-to-dawn curfew was enforced with police brutality, including shootings, beatings, whipping, tear gassing, looting, and financial extortion. In some cases, police began such violence well before the curfew began. Videos also show police not wearing masks and physically crowding civilians together.[53] Overall, public health and legal experts have argued that voluntary self-isolation efforts, compared to coercive efforts, are more likely to result in cooperation and trust in the public health system.[54]
Another key human rights impact of household confinement (and the inherent movement restrictions) is the potential infringement of the right to health and well-being as protected by article 25 of the UDHR, specifically with regard to access to health care.[55] While such extreme movement restrictions may affect most of the population, their consequences are especially pronounced among populations with an increased need to access health care, such as pregnant women and young children. The COVID-19 pandemic has reduced maternal health care seeking and provision globally, and slum communities in low- and middle-income countries have been particularly disadvantaged in terms of access to health care services.[56] While the underlying mechanisms are complex and most likely multicausal, disruptions to routine health care have been estimated to result in devastating child and maternal mortality.[57] Additionally, household confinements to contain the spread of COVID-19 have led to major disruptions to routine childhood vaccination coverage, resulting in immunity gaps for other infectious diseases such as measles, which most likely will exacerbate the pandemic’s detrimental effect on maternal and child health.[58]
Discussion
This paper demonstrates that COVID-19 public health policies enacted in the first six months of the pandemic present potential human rights violations and discusses the need to design such policies in a way that centers the needs of vulnerable groups. While pandemic containment policies are essential for controlling transmission and reducing mortality, governments must be vigilant against these measures slipping into human rights abuses by design or by negligence.
We analyzed COVID-19-related public health policies implemented from January 1 to June 30, 2020. Using the UDHR standards as a guide, we found that 71.67% of the 10,720 interventions implemented in these six months had potential human rights impacts. In particular, we examined the five most common types of policies (school closures, border closures, quarantine and isolation, limiting gatherings, and household confinement) in further detail through a human rights lens. We found that some COVID-19 public health interventions may be impractical or impossible to adhere to for vulnerable groups, such as refugees, unstably housed people, low-income people, and undocumented individuals. For instance, household confinement orders are impractical to follow for people who are unstably housed due to lack of housing or living in overcrowded settings. These interventions may also put these groups and others at risk of further human rights violations. For example, people who cannot follow household confinement orders, such as the unstably housed, may face violence by members of the police or military who are enforcing household confinement with force.
This paper has limitations. First, our analysis was descriptive and deductive: we did not focus on any specific subpopulations or analyze empirical data related to human rights violations. We did not directly assess the human rights implications of COVID-19 policies and thus cannot provide a causal analysis of any specific human rights violations as a result of COVID-19 policies. Due to data availability, we were able to discuss only those policies enacted in the first six months of the pandemic, which does not cover more current concerns such as vaccine inequities and treatments for novel SARS-CoV-2 variants that will require additional human rights analysis. While this article focuses on public health restrictions, the emphasis on vulnerable communities and negative human rights impacts is also relevant to other aspects of the COVID-19 response, such as vaccine hesitancy, ongoing debates about mask mandates, and public acceptance of policies related to COVID-19. Finally, due to the underreporting of COVID-19 policies in low-income countries, our data are probably not fully representative of all policies implemented in the study period.
An in-depth consideration of whom public health policies impact and how they may disproportionately affect specific groups, intentionally or not, is critical to ensuring meaningful equity and effectiveness of interventions. This pandemic has exacerbated many preexisting societal inequities and human rights violations affecting marginalized populations, making it even more crucial to design intentionally equitable policy responses that are based on human rights principles.
Human rights, such as the rights to assembly, movement, religion, and privacy, can be negatively impacted by COVID-19 public health policies, particularly with regard to already marginalized or vulnerable people. Socially equitable interventions might be more tailored, focusing human rights restrictions on communities in limited ways, or enforcing them with consideration of the needs and abilities of vulnerable communities. Blanket public policies run the risk of violating basic human rights without the necessity and proportionality laid out in the Siracusa Principles and the ICESCR. This idea is informed by the harm reduction approach of the HIV/AIDS pandemic and acknowledges that a strict all-or-nothing approach is not practical for all.[59] As a result, there is an urgent need to consider the protection of vulnerable populations from human rights abuses when implementing COVID-19 interventions and ensure that any derogations from human rights norms are conducted “in accordance with the law; based on a legitimate objective; strictly necessary in a democratic society; the least restrictive and intrusive means available; and not arbitrary, unreasonable, or discriminatory.”[60] These stipulations, laid out in the Siracusa Principles, could protect citizens from discriminatory and unnecessary restrictions but will require more concrete integration into national and local public health laws and policies in order to be effective. In authoritarian settings, reliance on international accountability mechanisms will be critical to protect vulnerable people.
Consideration of human rights may also increase the effectiveness of public health policies. With sweeping public health interventions, those who are already at higher risk of morbidity and mortality may be subjected to more severe health and economic costs. Without considering the costs and trade-offs of interventions and ensuring that their design considers their secondary impacts, such public health policies may paradoxically violate the right to health as defined by the World Health Organization: “a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity.”[61] In doing so, these policies can risk worsening the health of marginalized communities.
Recommendations for future policy and practice at the nexus of public health and human rights
We argue that public health interventions should (1) prioritize the most vulnerable and underserved populations, (2) ensure additional support for such communities, including access to financial, social, and medical resources, and (3) be formulated to consider not only pandemic control but also the health and human rights of those they impact. Based on our analysis, public health decision-makers must ensure that public health interventions are executed with a human rights lens by taking concrete steps in both policy and practice (see Table 3).
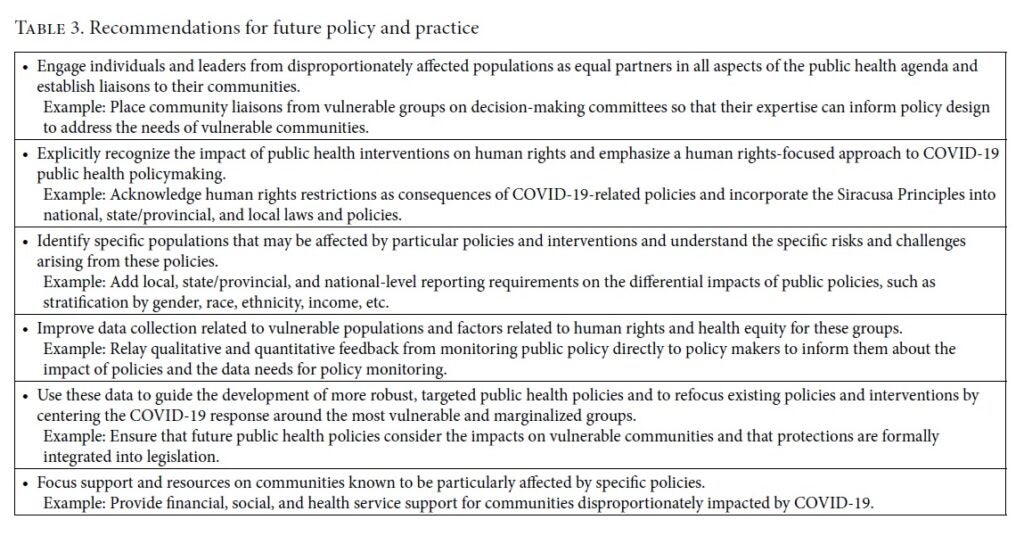
Decision-makers must follow a forward-thinking approach while constantly assessing and reassessing policies and restrictions for potential impacts on human rights and inequities. Likewise, policy decisions need to be adapted to emerging issues and challenges that arise during long-lasting crises. Whereas our analysis focused on the early phases of the COVID-19 pandemic, global inequities in access to COVID-19 vaccines have emerged as the dominant human rights issue in 2021, with high-income countries controlling the vast majority of the global vaccine supply.[62] Our database did not include information on vaccination policies, but this example strikingly demonstrates how both data collection and policymaking need to flexibly adjust to rapid developments to ensure that emerging human rights issues can be addressed in a timely manner.
While these recommendations can help reduce the negative human rights impacts of public health interventions, there will still be communities that disproportionately suffer. It is imperative that any utilitarian approach look deeply at the short- and long-term impacts on marginalized communities and establish concrete mechanisms for redress and compensation.[63] This could include financial support, additional health services, health insurance coverage, policy changes, and social support. While these steps may be aspirational in practice, they are required to build a healthier and fairer world. Curbing the COVID-19 pandemic requires a strong public health response—but to do it equitably and effectively requires a human rights framework.
Acknowledgments
We thank Leonard Rubenstein and Swetha Manne for catalyzing this research concept.
Sophia A. Zweig, ScM, is a medical student at SUNY Downstate Health Sciences University College of Medicine, Brooklyn, USA.
Alexander J. Zapf, MSPH, MSc, is an epidemiologist in the Department of International Health at the Johns Hopkins Bloomberg School of Public Health, Baltimore, USA.
Chris Beyrer, MD, MPH, is the Desmond M. Tutu Professor of Public Health and Human Rights in the Department of Epidemiology at the Johns Hopkins Bloomberg School of Public Health, Baltimore, USA.
Debarati Guha-Sapir, PhD, is the director of the Centre for Research on the Epidemiology of Disasters and a professor at the University of Louvain School of Public Health, Brussels, Belgium.
Rohini J. Haar, MD, MPH, is an adjunct professor in the Division of Epidemiology, School of Public Health and a research fellow in the Human Rights Center, School of Law at the University of California, Berkeley, USA.
*Both authors contributed equally to this manuscript as first authors.
Please address correspondence to Rohini J. Haar. Email: rohinihaar@berkeley.edu.
Competing Interests: None declared.
Copyright © 2021 Zweig, Zapf, Beyrer, Guha-Sapir, and Haar. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted noncommercial use, distribution, and reproduction.
References
[1]. J. M. Brauner, S. Mindermann, M. Sharma, et al., “Inferring the effectiveness of government interventions against COVID-19,” Science 371/6531 (2020); Y. Liu, C. Morgenstern, J. Kelly, et al., “The impact of non-pharmaceutical interventions on SARS-COV-2 transmission across 130 countries and territories,” BMC Medicine 19/1 (2021), pp. 1–12.
[2]. M. Aragona, A. Barbato, A. Cavani, et al., “Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties,” Public Health 186 (2020), pp. 52–56; A. Peterman, A. Potts, M. O’Donnell, et al., “Pandemics and violence against women and children,” Center for Global Development working paper 528 (2020). Available at https://www.un.org/sexualviolenceinconflict/wp-content/uploads/2020/05/press/pandemics-and-violence-against-women-and-children/pandemics-and-vawg-april2.pdf; D. Guha-Sapir, M. Moitinho de Almedia, M. Jaita, et al., “COVID-19 policies: Remember measles,” Science 369/ 6501 (2020), p. 261.
[3]. L. Gostin, “Towards a human rights-based approach to COVID-19,” National Academy of Medicine (2020). Available at http://www.youtube.com/watch?v=MkcYlMtTQN4; D. G. McNeil, “Using a tactic unseen in a century, countries cordon off Ebola-racked areas,” New York Times (August 13, 2014). Available at https://www.nytimes.com/2014/08/13/science/using-a-tactic-unseen-in-a-century-countries-cordon-off-ebola-racked-areas.html?smid=url-share.
[4]. International Commission of Jurists, Siracusa Principles on the Limitation and Derogation Provisions in the International Covenant on Civil and Political Rights (1984).
[5]. A. Ponta, “Human rights law in the time of the coronavirus,” American Society of International Law 24/5 (2020).
[6]. International Covenant on Economic, Social and Cultural Rights, G.A. Res. 2200A (XXI) (1966), art. 14; D. S. Silva and M. J. Smith, “Limiting rights and freedoms in the context of Ebola and other public health emergencies: How the principle of reciprocity can enrich the application of the Siracusa principles,” Health and Human Rights Journal 17/1 (2015), p. 52.
[7]. Silva and Smith (see note 6); L. O. Gostin, J. T. Monahan, J. Kaldor, et al., “The legal determinants of health: Harnessing the power of law for global health and sustainable development,” Lancet 4/393 (2019), pp. 1857–1910; L. O. Gostin, “When terrorism threatens health: How far are limitations on human rights justified?” Journal of Law, Medicine and Ethics 31/4 (2003), pp. 524–528.
[8]. S. Sekalala, L. Forman, R. Habibi, et al., “Health and human rights are inextricably linked in the COVID19 response,” BMJ Global Health 5/9 (2020), pp. 1–7.
[9]. A. Hayakawa, In India’s slums, social distancing is a luxury that can’t be afforded (2020). Available at http://asia.nikkei.com/Spotlight/Coronavirus/In-India-s-slums-social-distancing-is-a-luxury-that-can-t-be-afforded.
[10]. C. Pettus-Davis, S. C. Kennedy, amd C. A. Veeh, “Incarcerated individuals’ experiences of COVID-19 in the United States,” International Journal of Prisoner Health (2021). Available a https://www.meta.org/papers/incarcerated-individuals-experiences-of-covid-19/33760428.
[11]. Gostin (2020, see note 3).
[12]. Committee on Economic, Social and Cultural Rights, General Comment No. 19, UN Doc. E/C.12/GC/19 (2008), para. 31.
[13]. Othering and Belonging Institute, University of California, Berkeley, COVID-19: Mapping vulnerable populations in California (2020). Available at http://belonging.berkeley.edu/covid-19-mapping-vulnerable-populations-california; Social Protection and Human Rights, Disadvantaged and vulnerable groups (2018). Available at http://socialprotection-humanrights.org/key-issues/disadvantaged-and-vulnerable-groups.
[14]. Q. Zheng, F. K. Jones, S. V. Leavitt, et al., “HIT-COVID, a global database tracking public health interventions to COVID-19,” Scientific Data 7/1 (2020), pp. 1–8.
[15]. J. McCarthy, “Protesters across Europe clash with police over COVID-19 lockdowns,” National Public Radio (March 21, 2021). Available at http://www.npr.org/2021/03/21/979653125/protesters-across-europe-clash-with-police-over-covid-19-lockdowns; “Michigan protesters demonstrate against stay-at-home order,” NBC News (April 30, 2020). Available at http://www.nbcnews.com/video/michigan-protesters-demonstrate-against-stay-at-home-order-82826309570; A. Taylor, “Three nights of anti-lockdown violence in the Netherlands,” Washington Post (January 26, 2021). Available at http://www.washingtonpost.com/graphics/photography/2021/01/26/dutch-coronavirus-curfew-riots-photos/.
[16]. Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948).
[17]. K. A. Auger, S. S. Shah, T. Richardson, et al., “Association between statewide school closure and COVID-19 incidence and mortality in the US,” JAMA 324/9 (2020), pp. 859–870; S. Walsh, A. Chowdhury, V. Braithwaite, et al., “Do school closures reduce community transmission of COVID-19? A systematic review of observational studies,” MedRxiv (2021).
[18]. J. M. Donohue and E. Miller, “COVID-19 and school closures,” JAMA 324/9 (2020), pp. 845–847; E. Bendavid, C. Oh, J. Bhattacharya, and J. Ioannidis, “Assessing mandatory stay‐at‐home and business Closure effects on the spread of COVID‐19,” European Journal of Clinical Investigation 51/4 (2021), p. e13484.
[19]. Pew Research Center, “Internet, science and tech: Demographics of internet and home broadband usage in the United States” (2019). Available at http://www.pewresearch.org/internet/fact-sheet/internet-broadband/.
[20]. M. Kaffenberger, “Modelling the long-run learning impact of the COVID-19 learning shock: Actions to (more than) mitigate loss,” International Journal of Educational Development 81 (2021).
[21]. G. P. Vegas, H. Patrinos, V. Collis, et al., “The COVID-19 cost of school closures,” Brookings (April 29, 2020). Available at http://www.brookings.edu/blog/education-plus-development/2020/04/29/the-covid-19-cost-of-school-closures/.
[22]. J. Lee, “Mental health effects of school closures during COVID-19,” Lancet Child and Adolescent Health 4/6 (2020), p. 421; YoungMinds, Coronavirus report: Impact on young people with mental health needs (2021).
[23]. H. Grant, “Why COVID school closures are making girls marry early,” Guardian (September 7, 2020). Available at http://www.theguardian.com/global-development/2020/sep/07/why-covid-school-closures-are-making-girls-marry-early/.
[24]. World Bank, Educating girls, ending child marriage (August 24, 2017). Available at http://www.worldbank.org/en/news/immersive-story/2017/08/22/educating-girls-ending-child-marriage/.
[25]. Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948), art. 13.
[26]. World Health Organization, International health regulations (2005), 3rd edition (Geneva: World Health Organization, 2016), p. 1.
[27]. N. Haug, L. Geyrhofer, A. Londei, et al., “Ranking the effectiveness of worldwide COVID-19 government interventions,” medRxiv (2020); B. J. Cowling, S.T. Ali, T.W.Y. Ng, et al., “Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: An observational study,” Lancet Public Health 5/5 (2020), pp. e279–e288; M.U. Kraemer, C. Yang, B. Gutierrez, et al., “The effect of human mobility and control measures on the COVID-19 epidemic in China,” Science 368/6490 (2020), pp. 493–497.
[28]. S. Lai, N. W. Ruktanonchai, L. Zhou, et al., “Effect of non-pharmaceutical interventions to contain COVID-19 in China,” Nature 585/7825 (2020), pp. 410–413; H. Tian, Y. Liu, Y. Li, et al., “The impact of transmission control measures during the first 50 days of the COVID-19 epidemic in China,” Science 368/6491 (2020), pp. 638–642; M. Chinazzi, J. T. Davis, M. Ajelli, et al., “The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak,” Science 368/6489 (2020), pp. 395–400; Kraemer et al. (see note 27).
[29]. J. Loweree, A. Reichlin-Melnick, and W. Ewing, The impact of COVID-19 on noncitizens and across the U.S. immigration system (Washington, DC: American Immigration Council, 2020); N. Smart and A. Garcia, “Tracking COVID-19 in immigration detention,” Vera Institute of Justice (November 18, 2020). Available at http://www.vera.org/tracking-covid-19-in-immigration-detention.
[30]. ICE Guidance on COVID-19.” U.S. Immigration and Customs Enforcement. (July 12, 2020). Available at https://web.archive.org/web/20200712042337/http://www.ice.gov/coronavirus; Immigration and Customs Enforcement. (July 14, 2020). Available at https://web.archive.org/web/20200714055538/http://www.ice.gov/coronavirus#tab2.
[31]. Smart and Garcia (see note 29).
[32]. E. Cahan, “America’s immigration system is a COVID Superspreader,” Scientific American. Available at http://www.scientificamerican.com/article/americas-immigration-system-is-a-covid-superspreader/.
[33]. A. Ibarra and B. Lyons, “Immigration detention centers showcase vaccine chaos,” Cal Matters (February 22, 2021). Available at http://calmatters.org/health/coronavirus/2021/02/immigrants-detention-centers-vaccine/.
[34]. J. Matovinovic, “A short history of quarantine,” University of Michigan Medical Center Journal 35/4 (1969), pp. 224–228.
[35]. W. E. Parmet and M. S. Sinha, “COVID-19: The law and limits of quarantine,” New England Journal of Medicine 382/15 (2020), pp. e(28)1–e(28)3; L. O. Gostin and L. F. Wiley, “Governmental public health powers during the COVID-19 pandemic,” JAMA 323/21 (2020), p. 2137; A. J. Kucharski, P. Klepac, A. J. Conlan, et al., “Effectiveness of isolation, testing, contact tracing, and physical distancing on reducing transmission of SARS-Cov-2 in different settings: A mathematical modelling study,” Lancet Infectious Diseases 20/10 (2020), pp. 1151–1160.
[36]. Gostin and Wiley (2020, see note 35); J. J. Openshaw and M.A. Travassos, “COVID-19, quarantines, Sheltering-in-place, and Human rights: The developing crisis,” American Journal of Tropical Medicine and Hygiene 103/2 (2020), pp. 578–580.
[37]. Openshaw and Travassos (see note 36); M. Wallace, M. Marlow, and S. Simonson, “Public health response to COVID-19 cases in correctional and detention facilities: Louisiana, March–April 2020,” Morbidity and Mortality Weekly Report 69 (2020), pp. 594–598; V. Bhavsar, K. Kirkpatrick, M. Calcia, et al., “Lockdown, domestic abuse perpetration, and mental health care: Gaps in training, research, and policy,” Lancet Psychiatry 8/3 (2021), pp. 172–174; M. L. Evans, M. Lindauer, and M. E. Farrell, “A pandemic within a pandemic: Intimate partner violence during COVID-19,” New England Journal of Medicine 383/24 (2020), pp. 2302–2304; Aragona et al. (see note 2); S. K. Brooks, R. K. Webster, L. E. Smith, et al., “The psychological impact of quarantine and how to reduce it: Rapid review of the evidence,” Lancet 395/10227 (2020), pp. 912–920; P. C. Terry, R. L. Parsons-Smith, and V. R. Terry, “Mood responses associated with COVID-19 restrictions,” Frontiers in Psychology 11/589598 (2020).
[38]. International Commission of Jurists (see note 4); Brooks et al. (see note 37).
[39]. M. Roje Đapić, G. Buljan Flander, and K. Prijatelj, “Children behind closed doors due to COVID-19 isolation: Abuse, neglect and domestic violence,” Archives of Psychiatry Research 56/2 (2020), pp. 181–192.
[40]. H. Jeong, H. W. Yim, Y. Song, et al., “Mental health status of people isolated due to Middle East respiratory syndrome,” Epidemiology and Health 38 (2016).
[41]. Peterman et al. (see note 2).
[42]. City of New York, Isolation hotel program for those with COVID-19 (2021). Available at http://www1.nyc.gov/site/helpnownyc/get-help/covid-19-hotel-program.page; Baltimore City Health Department, Lord Baltimore Hotel, triage, respite, and isolation (TRI) center (2020). Available at http://www.icarol.info/ResultDetails.aspx?org=2046&agencynum=68805084.
[43]. Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948), art. 20.
[44]. D. Dave, A. Friedson, D. McNichols, et al., “The contagion externality of a superspreading event: The Sturgis motorcycle rally and COVID-19,” National Bureau of Economic Research working paper 27813 (2020). Available at http://www.nber.org/papers/w27813; U.S. Centers for Disease Control and Prevention, Deciding to go out (2019). Available at http://www.cdc.gov/coronavirus/2019-ncov/daily-life-coping/deciding-to-go-out.html.
[45]. “Thousands protest in Algeria, hoping to rekindle mass demos,” Reuters (February 16, 2021). Available at http://www.reuters.com/article/algeria-protests-anniversary-kherrata-in/thousands-protest-in-algeria-hoping-to-rekindle-mass-demos-idUSKBN2AG1UK.
[46]. L. von Seidlein, G. Alabaster, J. Deen, et al., “Crowding has consequences: Prevention and management of COVID-19 in informal urban settlements,” Building and Environment 188 (2021).
[47]. Hayakawa (see note 9).
[48]. Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948), art. 13.
[49]. R.C. Castillo, E. D. Staguhn, and E. Weston-Farber, “The effect of state-level stay-at-home orders on COVID-19 infection rates,” American Journal of Infection Control 48/8 (2020), pp. 958–960.
[50]. United Nations, COVID-19 and human rights: We are all in this together (2020). Available at http://www.un.org/victimsofterrorism/sites/www.un.org.victimsofterrorism/files/un_-_human_rights_and_covid_april_2020.pdf.
[51]. Peterman et al. (see note 2).
[52]. Sixth Tone, How COVID-19 sparked a silver tech revolution in China (2020). Available at http://www.sixthtone.com/news/1005303/how-covid-19-sparked-a-silver-tech-revolution-in-china.
[53]. Human Rights Watch, Kenya: Police brutality during curfew (April 22, 2020). Available at http://www.hrw.org/news/2020/04/22/kenya-police-brutality-during-curfew.
[54]. Human Rights Watch, Human rights dimensions of COVID-19 response (March 19, 2020). Available at https://www.hrw.org/news/2020/03/19/human-rights-dimensions-covid-19-response; Brooks et al. (see note 37).
[55]. Universal Declaration of Human Rights, G.A. Res. 217A (III) (1948), art. 25.
[56]. R. Townsend, B. Chmielewska, I. Barratt, et al., “Global changes in maternity care provision during the COVID-19 pandemic: A systematic review and meta analysis,” EClinicalMedicine 37 (July 1, 2021); S. A. K. S. Ahmed, M. Ajisola, et al., “Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: Results of pre-COVID and COVID-19 lockdown stakeholder engagements,” BMJ Global Health 5/8 (2020).
[57]. T. Roberton, E. D. Carter, V. B. Chou, et al., “Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: A modelling study,” Lancet Global Health 8/7 (2020), pp. e901–e908.
[58]. K. Causey, N. Fullman, R. J. D. Sorensen, et al., “Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: A modelling study,” Lancet 398/10299 (2021), pp. 522–534; World Health Organization, COVID-19 pandemic leads to major backsliding on childhood vaccinations, new WHO, UNICEF data shows (2021). Available at https://www.who.int/news/item/15-07-2021-covid-19-pandemic-leads-to-major-backsliding-on-childhood-vaccinations-new-who-unicef-data-shows; D. N. Durrheim, J. K. Andrus, S. Tabassum, et al., “A dangerous measles future looms beyond the COVID-19 pandemic,” Nature Medicine 27/3 (2021), pp. 360–361.
[59]. E. Kutscher and R. E. Greene, “A harm-reduction approach to coronavirus disease 2019 (COVID-19)-safer Socializing,” JAMA Health Forum (2020). Available at http://jamanetwork.com/channels/health-forum/fullarticle/2766837; D. Leonhardt, “COVID absolutism,” New York Times (February 12, 2021). Available at http://www.nytimes.com/2021/02/12/briefing/trump-covid-chick-corea-olympics-president.html; C. Arnold, “COVID-19: How the lessons of HIV can help end the pandemic,” BMJ 16/372 (2021).
[60]. Silva and Smith (see note 6); Gostin (2003, see note 7).
[61]. Constitution of the World Health Organization (1946).
[62]. “WHO calls for moratorium on COVID-19 booster jabs,” UN News (August 4, 2021). Available at https://news.un.org/en/story/2021/08/1097102.
[63]. Silva and Smith (see note 6).
