Volume 23/1, June 2021, pp. 259-271
Moses Mulumba, Ana Lorena Ruano, Katrina Perehudoff, and Gorik Ooms
Abstract
This paper presents a case study of how colonial legacies in Uganda have affected the shape and breadth of community participation in health system governance. Using Habermas’s theory of deliberative democracy and the right to health, we examine the key components required for decolonizing health governance in postcolonial countries. We argue that colonization distorts community participation, which is critical for building a strong state and a responsive health system. Participation processes grounded in the principles of democracy and the right to health increase public trust in health governance. The introduction and maintenance of British laws in Uganda, and their influence over local health governance, denies citizens the opportunity to participate in key decisions that affect them, which impacts public trust in the government. Postcolonial societies must tackle how imported legal frameworks exclude and limit community participation. Without meaningful participation, health policy implementation and accountability will remain elusive.
Introduction
Community participation is a critically important component of building public trust in health governance, as well as a key feature of the right to health.[1] It refers to the free, active, meaningful, and inclusive processes through which people make decisions on issues that affect them, their families, and their communities.[2] Colonialism deeply affects a country’s social fabric and inherently changes social, cultural, political, and economic structures in a way that continues to be felt decades after independence.[3] Using elements of Jürgen Habermas’s theory of deliberative democracy and the right to health as normative frameworks, this paper examines the legacies of colonialism in Uganda and how they have affected community participation in health system governance. We propose that health system decolonization requires embedding community participation through policies that incentivize historically marginalized and excluded groups to better disperse decision-making power, which is a consequential first step in truly achieving self-determination.
Colonization disrupts people’s connection to the land and forces a new country identity on existing cultures, communities, and families, and does so through policies that seek to control, stigmatize, and intervene in their lives.[4] Decolonization calls for the dismantling of several layers of complex and entrenched colonial structures, ideologies, narratives, identities, and practices, as well a reconstruction process that focuses on reclaiming humanity, rebuilding bodily integrity, and reasserting self-determination.[5] The political, economic, social, and cultural control that was leveraged on an occupied nation breaks down local social fabrics and creates inequality and public mistrust in the governance system. As a result, some populations become more and more excluded, and these historical cycles of disempowerment lead to further exclusion.[6] Colonialism also shapes the health system and all governance processes within, with a history of colonization acting as a key determinant of health for many vulnerable population groups.
Decolonizing health systems allows for a return of community participation that establishes true partnerships between communities and decision makers through empowerment cycles. Getting rid of the lasting impact of colonization calls for raising citizen awareness of rights and obligations and building collective action that promotes self-determination through dedicated policy frameworks and incentives that help ensure the dispersion of decision-making power in health policy.[7] This diffuses decision-making power among more stakeholders and ensures that health services reflect local needs, which increases communities’ control over maintaining and improving their health.[8] However, establishing these processes in contexts of exclusion and marginalization requires time and sustained support that allows for the reconfiguration of societal-level power dynamics.[9] This is crucial for strengthening public trust in health governance, which is a central building block of health systems’ ability to provide services efficiently, effectively, and equitably.[10]
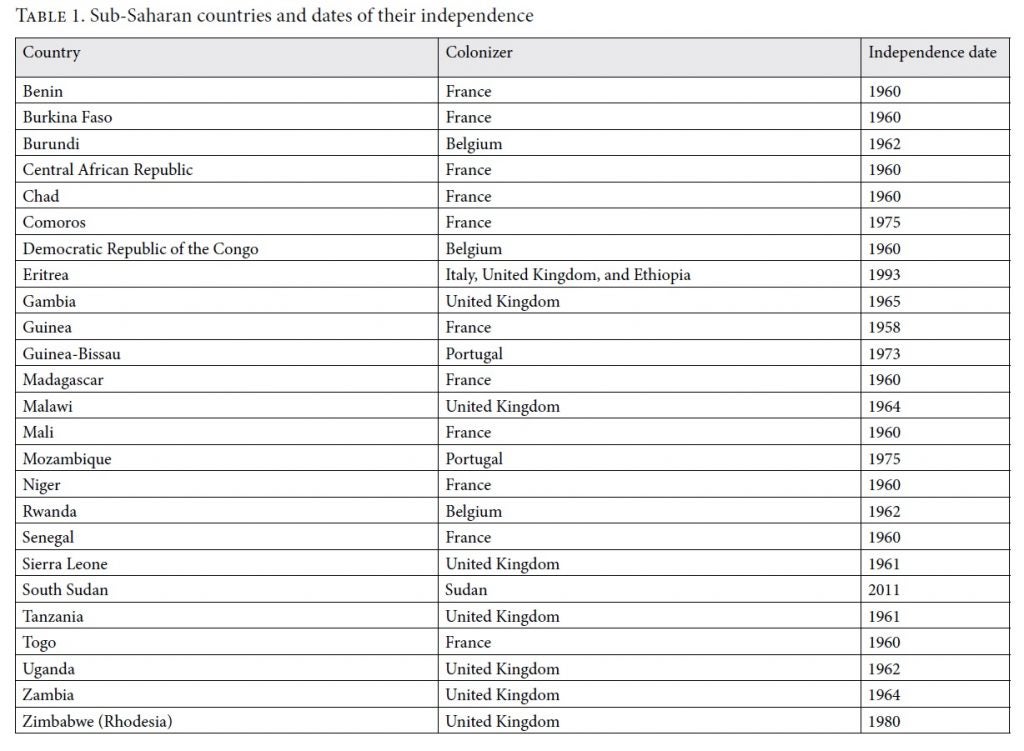
Like many countries in Sub-Saharan Africa and around the world, Uganda struggles with a recent colonial past and its legacy. In many former colonies, the effects of often brutal and forced colonization influence all aspects related to governance well into postcolonial self-rule.[11] Table 1 shows how many sub-Saharan countries were under colonial rule from as early as the late 1890s and began achieving independence only in the 1960s. For South Sudan, this came as late 2011. Today, almost all low-income countries in Sub-Saharan Africa have serious health governance challenges, and most still struggle with their colonial legacies.
We argue that achieving the highest attainable standard of health is intrinsically linked to Habermas’s theory of deliberative democracy. Communicative action, the power of speech, legitimacy, and the principles of legitimacy and the public sphere shape community participation and affect the way that communities engage with the health system and enjoy their right to health. Many postcolonial societies with weak deliberative democracy values continue to struggle with democracy because colonization impacted self-determination, which limits popular sovereignty, especially in context of extreme poverty and resource constraints.[12] This exclusion delegitimizes the public space, which is coopted by officials who were not elected by the people. This weakens democracy and increases authoritarian leadership, hence impacting public trust in the health system’s governance.[13] Democracy and human rights are co-original and can act in virtuous cycles of empowerment when they integrate previously excluded groups and lead to the type of systemic change that dismantles colonial structures at the ideological and practical level. Finally, community participation is central to the realization of the right to health, as stated in the United Nations Committee on Economic, Social and Cultural Rights’ General Comment 14.[14] By framing participation disparities as rights violations, public health advocates can draw on international legal standards to frame responsibilities and evaluate policies, shifting the analysis of health reform from a focus on the quality of care to one on social justice.[15]
Colonial governments’ dominance of their colonies required achieving control over the territory, which in turn involved the erosion of self-determination and the imposition of a rule rooted in the colonizer’s beliefs and practices.[16] Oftentimes, this translated into the enforcement of a foreign culture, religion, and social mores and customs through the slave trade, misappropriated natural resources, exploitative trade relations, and unfavorable means of producing wealth.[17] Such foreign systems of rule of law limited local peoples’ self-determination and sovereignty, for subjected communities were beholden to laws that they had not participated in making. The repressive systems that crushed Indigenous legal and health systems also disregarded local traditional values, which were then replaced by those of the colonial rules. These systems include the health system, which was organized by the colonizers based on their own ideas and beliefs around the type and number of services that should be provided to the local population.
As the Ugandan case study demonstrates, postcolonial countries continue to grapple with the impacts of colonial values on their legal and health systems. Laws criminalizing abortion and same-sex unions are just some examples. The missionary hospitals and schools introduced during colonial rule continue to account for almost 20% of Uganda’s health and education systems.[18] The values that guide these systems, instituted through colonial rule, disregard current scientific knowledge and human rights and represent key challenges to the delivery of empowering and liberating health and education systems. Uganda provides a good case study on the influence of political history on community participation.
Methods
This paper uses a qualitative, historical case-study methodology and is guided by an analysis of the political history of community participation in Uganda from the precolonial, colonial, and postcolonial periods.[19] The literature review included publicly available documents located through online searches for academic articles, government documents, nongovernmental organization (NGO) reports, and other gray literature. The publications considered were published in English and used rights-based approaches to health system strengthening. Additionally, publications that described or contextualized the historical events that shaped Uganda’s political setup and a health system were included in the study.
We analyzed data through a content analysis using two normative frameworks: (1) Habermas’s concept of deliberative democracy and (2) the right to health framework. Both frameworks center around the concept of community participation whereby people and communities are at the center of decision-making processes in health. These frameworks emphasize the tenets of the power of speech, legitimacy, and the public sphere, and they advance the argument that the decolonization of health systems is important for allowing community participation in health systems to thrive.
Our analysis focused on understanding the colonial period’s subrogation of community participation and public trust in health governance. By applying the normative guidance provided by Habermas’s deliberative democracy framework and the right to health framework, we uncovered the need for decolonization that emphasizes community participation as part of building public trust in the health system.
The Uganda case study
Uganda provides an opportunity for studying the historical and political influences of colonialism on community participation as an integral part of the right to health and health governance generally. Uganda has transitioned through the precolonial, colonial, and present-day periods of developing a democracy and a health system. The formation of its national development agenda in the post-colonial period and the rolling out of its decentralized health system also offers an opportunity to examine the colonial influences on the structures for community participation through the lens of constitutional provisions, local government legislation, and other policy frameworks that provide the foundation for operationalizing community participation. Through periodization into precolonial, colonial, and postcolonial, the history of the country allows us to critically assess the extent to which community participation was lost during the colonial period. This then provides a basis for examining the decolonization steps needed to bring back community participation as part of good health governance. As we argue, it is difficult to separate Uganda’s current health system from its colonial and political history, as the latter continues to influence the architecture of the health system today.
Precolonial community participation
During the precolonial period, communities organized around kingdoms, in which community participation was a key social tenet.[20] For example, in the Buganda Kingdom, kingship was made into a kind of state lottery in which all clans could participate.[21] The community consolidated its efforts behind a centralized kingship, and this provided the community an opportunity to expand. Everyday life was organized around communal efforts. Social capital was critical for mobilization, which included rotating groups for labor sharing in the clearing, planting, weeding, and harvesting stages of agriculture, as well as emergency-oriented arrangements, such as local burial assistance groups that provided material and psychosocial support to bereaved families.[22] Community participation evolved around self-help projects, which enhanced communities’ economic and social welfare through a scheme called bulungi bwansi (“for the good of the community”).[23] Community participation was therefore interwoven into the fabric of precolonial Ugandan society. It also included some features of deliberative democracy and the right to health.
The practice of traditional medicine was the only health system that existed in Uganda during the precolonial period.[24] Traditional medicine practitioners included herbalists, bonesetters, psychic healers, birth attendants, faith healers, diviners, and spiritualists who used Indigenous knowledge to develop materials and procedures.[25] Despite the colonial government’s suppression of traditional medicine practitioners, traditional medicine survived colonization and continues to play a role in Uganda’s present-day health system. The question of regulating these practices remains a major health governance issue for Uganda’s health system. Communities have continued to demonstrate trust in traditional healers, despite the documented public health hazards that they have caused.
The key lesson from this period is that in the quest for a normative community participation structure that decolonizes health governance, Indigenous ideas and innovation should be taken into account. This is especially important when trying to understand the public sphere and how culture, attributes, beliefs, and norms can inform the normative structure of community participation.[26] In applying the human rights framework, validating and empowering these Indigenous spaces is important for advancing the right to participation as enshrined in international human rights law.
Community participation during Uganda’s colonial period
Uganda was a protectorate of the British Empire from 1894 to 1962, and although the economic, social, and political landscape changed dramatically, the country retained a degree of self-government that was uncommon.[27] Different Indigenous communities now inhabiting the country were brought together during the colonial period following the declaration of a British protectorate over Uganda in 1894.[28] Political dispensations unified traditional kingdoms that had enjoyed sovereign powers until then. New lawmaking processes were developed in Britain and enforced first in Buganda and quickly expanded to other kingdoms. The period saw many developments that would later shape the discussion on community participation in health governance amid British rule and the continued influence of the kingdoms.
The colonial administration imposed its own system of administration through indirect rule, whereby the British administered the protectorate through local chiefs and kings, who surrendered sovereignty in return for British protection. Because the colonialists obliged certain communities to merge, the uniformity of former autonomous chiefdoms was lost along with traditional practices of community participation.[29] The traditional discursive spaces were dismantled as the British enforced their rules and introduced forced labor and exploitative tax systems.
During this period, Britain signed a number of agreements with both Buganda as a kingdom and later Uganda as a protectorate that spelled out governance issues between the colonizers and the colony.[30] Through these agreements, Britain shaped the structure of government, including provisional administrative decisions and the administration of justice and maintenance of order.[31] However, the structures introduced were devoid of key elements of deliberative democracy, such as a public sphere. Local communities were excluded from formal decision-making, which was now the exclusive competence of the colonial rulers. At the signing of the 1900 Buganda Agreement, for instance, the Buganda signatories were allowed only to append signatures, and there is no evidence of them being included in the development of the agreement itself.[32] Therefore, the Buganda Agreement was not a legitimate instrument when seen through the lens of deliberative democracy.
The agreement then became part of Uganda’s modern legal system. Interestingly, it also introduced the concept of public interest, which was not discussed but mentions cursorily that government was to be the custodian of resources on behalf of the people. Today, the families and communities affiliated with those who benefited from the Buganda Agreement continue to dominate land ownership. Given the centrality of land as a resource, a large amount of decision-making power is now concentrated among a few families, and critical processes such as the allocation of land for health facilities and leadership in community participation structures are still separated from the people who would benefit the most from them.[33] These families act as power centers and exert control in many governance processes, including those related to the health system.
The next significant step that the British government took to solidify its rule in the Protectorate of Uganda after the Buganda Agreement was the establishment of the 1902 Orders in Council.[34] The Orders in Council dealt with matters of constitutional significance and were the benchmark against which many laws in colonial and postcolonial Uganda were built, as they provided the first legal instrument for establishing a legal framework of government for the entire protectorate.[35] Their major limitation was that they brought in UK legal frameworks without any adaptation to the local context. This was in complete disregard of the importance of community participation in legal decision-making for a country. Lord Denning, in the case of Nyali Ltd. v. Attorney General, challenged this practice when he used an analogy of an oak tree and concluded that one cannot transplant an oak tree from English soil and plant it on Kenyan soil and expect it to flourish well like it did before.[36]
Article 15(1) of the 1902 Orders in Council established the judicial system, including the High Court, which was to have full civil and criminal jurisdiction over all persons and matters in Uganda. The court system is critical for health governance given the important role of litigation in health issues, as witnessed in present-day Uganda. The relevance of courts in health governance is visible in the important court decisions and pronouncements in relation to accessing health care. The Constitutional Court, for instance, has ruled that the government’s failure to provide adequate maternal health services violates human rights protected in international treaties and the Ugandan Constitution, including the right to health, the right to life, the rights of women, and the prohibition of inhuman and degrading treatment.[37] The courts have also declared the criminal legislation concerning mental health as violating rights and have called for provisions that better enhance the rights of persons with disabilities.[38] The colonial procedural challenges in the usage of courts to advance health have seen some of these cases take as long as nine years to be decided.
Although the 1902 Orders in Council put in place the basic elements and structures of government, they did not further democracy in the protectorate. Uganda remained under direct control of the British, and there was no Indigenous representation within the government. The concept of democracy calls for the representation of people in government, and their exclusion signals an absence of it. The subjugation of community participation and the direct importation of British laws denied Ugandans the opportunity to participate in key decisions that affected them. As Kwanele Asante has argued, a non-rights-based approach absolves state parties of their duty to ensure that patients (communities) are substantively involved in the development of key health policies.[39] We agree with Asante that diluted community inclusion not only absolves states of their human rights duties with respect to the right to health and right to participate, but also renders communities unable to hold policy makers and governments accountable for inadequately discharging their right to health duties.
The control of sleeping sickness—the focal medical policy between 1900–1908—is an example of the implications of the aforementioned colonial governance structures for health. Sleeping sickness is caused by the tsetse fly, commonly found in tropical climates, including the region around Lake Victoria in Uganda. Kirk Arden Hoppe recounts how from 1906 onward local ordinances devoid of community participation were imposed by British rulers under the guise of disease control. For example, the Entebbe Township Ordinance of 1906 permitted the inspection and punishment of Ugandan canoe owners and crew who were found to have a tsetse fly on board. Punishment was in the form of a fine or one month’s imprisonment. The 1907 Uganda Fishing Ordinance made it illegal to fish on Lake Victoria and to possess or sell lake fish, which was an important source of nutrition and income for local Ugandans. In 1908 and 1909, health regulations were issued to consolidate and later evict 33 island communities in Lake Victoria to the mainland. Although framed as a disease control initiative, these regulations were a covert method of strategically depopulating people from an area (the Lake Victoria region) rich in hunting, fishing, and charcoal.[40]
These laws and regulations further marginalized Ugandans by depriving them of interdependent civil, economic, and social rights, including autonomy and the social determinants of health. Ugandans affected by these rules had no avenue for recourse to hold colonial decision-makers accountable, which is an essential component of the right to health. However, by the time of independence, Uganda had begun to witness some form of democracy that would see citizens participate in decision-making on issues affecting them.
Health governance in the colonial period
The colonial period saw the introduction of the formal health system through the establishment of mission hospitals. By 1909, three health centers in Mulago, Mengo, and Masaka were established for the treatment of venereal diseases, a new epidemic that affected mostly Europeans doing the postcolonial work and Indians who had been brought in to develop the infrastructure. Controlling venereal disease was a core medical policy of the colonial government from 1908 until the 1920s.[41] The Mulago health center was later developed into a general national referral hospital for venereal diseases. More hospitals and dispensaries were established in provincial and district headquarters throughout Uganda. These institutions were planned from the central level and without any community participation. Moreover, the epidemic of venereal disease was an opportunity for the colonial government to exert social control and to impose notions about sexuality and Christian values brought by missionaries.[42] These ideas, differing from local conceptions of venereal disease, were later enshrined in the Venereal Diseases Act of 1977.[43] One example of how the Venereal Disease Act violates the right to health is the requirement that a person with a sexually transmitted disease identify the person who infected him or her. Such forced disclosure tears at the social fabric of a community.
However, it was also during the colonial period that Uganda first witnessed a form of decentralization, when the British secretary for colonial administration made it colonial policy to promote the creation of local governments. This decentralization influenced Uganda’s health system through the introduction of health subdistricts.
The colonial control systems equated the practice of traditional medicine with witchcraft. As a result, the colonial government introduced the Witchcraft Act in 1957, which had provisions for the prevention of witchcraft and punishments for persons practicing witchcraft. In this way, the law attempted to strip Ugandans of the informal health system offered by traditional medicine. In 1997, the Supreme Court of Uganda, in the case of Salvatori Abuki and Richard Abuga v. Attorney General, held section 7 of this legislation unconstitutional for permitting the banishment of persons convicted of practicing witchcraft from their homes.[44] This judgment is a good example of some of the efforts to decolonize legislation introduced during colonial times. The judgment emphasized the importance of measuring the colonial laws against Uganda’s constitutional values.
Much of the health-related legislation that remains on the books today was imposed through the doctrine of legal reception, in which the British legal culture was transferred to Uganda. Laws such as the Public Health Act (1935), the Mental Treatment Act (1938), the Venereal Diseases Act (1977), the Penal Code Act (1950), and many others still affect health governance in Uganda. Starting in the 1930s, the colonial government shifted its medical focus to public health policy.[45] During this time, many laws relating to public health were adopted and have not been comprehensively reviewed since. Changing socioeconomic conditions call for legal frameworks to be updated, and often strengthened.[46] Some of these laws have been criticized for being restrictive in the area of reproductive rights, such as with regard to sexual orientation and access to safe and legal abortion.[47] In such cases, as part of decolonization, it is important to open a participatory dialogue around legal review to address gaps between policy, law, and practice.
It is also important to note that while colonial laws have stayed on the books, a number of areas that these laws targeted—such as harmful practices by traditional healers—continue today. For example, the recent wave of ritual murders, including child sacrifice, have prompted Ugandan parliamentarians to call for a law regulating the activities and practices of traditional healers and herbalists.[48] Abortion practices criminalized in the colonial Penal Code Act continue to contribute 1,200 deaths out of the total 6,500 maternal deaths each year.[49] There are also shared positive experiences and preferences by the population to use traditional healers because of their easy access, the ability to pay in installments or in kind for services rendered, and the kindness of traditional birth attendants.[50] These are important indications of the need to ensure community participation in the development of new regulatory frameworks that could address the country’s current health governance needs.
Postcolonial Uganda and community participation
Uganda gained independence on October 9, 1962, with signs of constitutionalism.[51] A constitution had been worked out as a result of negotiation among the major political actors.[52] Direct universal suffrage was put in place except for Buganda, where representatives to Parliament were indirectly elected through the Council of Buganda. On the first anniversary of independence, the Constitution was amended by Parliament to provide for a ceremonial president to replace the governor-general.[53] Overall, postcolonial Uganda had a mix of struggles to establish democratic structures and an early turbulent time with civil wars and coups that saw the obliteration of the earlier democratic structures that would have facilitated community participation in the health system. The post-colonial Uganda descended into dictatorial regimes in the tenures of Milton Obote, Idi Amin, Yusuf Lule, and Godfrey Binaisa, a period that did not feature community participation in decision-making for the country. In 1971, for instance, President Idi Amin Dada contradicted most of the constitutional provisions of 1962 and 1966. He denied Ugandan citizens democracy and ruled by decree.
Developments in the health system included the creation of the Ministry of Health, which had been formed just before independence to replace the colonial medical department responsible for medical services.[54] In addition, missionary health organizations provided health services in rural and urban areas through cost sharing.[55] The most important factors affecting the provision of socialized health services were the prevailing economic and political conditions in the country.
The government and its Ministry of Health had an ambitious program to build 22 100-bed hospitals, which was feasible due to the country’s economic prosperity between 1962 and 1971, during the first tenure of President Obote.[56] The country had four recognized health care service types and levels: (1) primary health care, consisting of centers and clinics; (2) secondary health care, consisting of district hospitals; (3) tertiary health care, consisting of general referral hospitals; and (4) quaternary health care, consisting of two national referral hospitals.[57] There were regional referral hospitals throughout the country. The role of health in Uganda’s development was one of high priority. The country’s planning strategies had health services and education as one of three important development goals.[58]
Uganda’s health system was going through some important reforms, but there is no evidence of community participation in the making of the policies or the implementation of health reforms during this period. The challenges that resulted from this nonparticipation were the adoption of reforms based on technical considerations without the integration of community perspectives. As a result, some of the health governance structures (such as health unit management committees) do not respond to community needs, and communities do not view them as “theirs.” This approach advances a colonial legacy of focusing on communities as passive beneficiaries.
The political and economic turmoil of the 1970s and 1980s also severely curtailed community engagement in the health systems. Social services, including health, broke down.[59] The working environment in the health sector became hostile, and many physicians migrated to other countries for security and economic reasons. Medicines, equipment, and hospital facilities were in limited supply, and the quality of health care fell drastically. At the same time, an unregulated private sector mushroomed rapidly to fill the services gap created by the poorly functioning government facilities that dominated the colonial health system architecture. This situation dashed any hopes of building a health system grounded in community participation.
After independence in 1962, efforts to strengthen national and cultural identities began to reemerge. For instance, it is now clear that the government is interested in providing support to the practice of traditional medicine. The repeal of the 1968 Medical and Dental Practitioners Act in 1996 created a situation in which traditional practitioners are tolerated as long as they do not claim to be registered medical practitioners.[60]
During this postcolonial period, a number of colonial laws have been successfully challenged before Ugandan courts as unconstitutional and in violation of human rights standards. For instance, section 130 of the Penal Code Act has been held unconstitutional insofar as it refers to persons with mental disabilities as idiots and imbeciles.[61] In this case, the petitioners successfully argued that the Penal Code subjected persons with mental disabilities to inhuman and degrading treatment, contrary to articles 24 and 35 of Uganda’s Constitution.
Discussion
This paper has demonstrated that understanding a country’s historical context is key for decolonizing its health governance. Through the Ugandan case study, we have identified key events that are central in defining a basis for decolonizing governance in health systems. The colonial legacy in Uganda imposed values and systems that undermined self-determination and sovereignty, which eroded even the most cherished precolonial systems that would provide a base for community participation as part of health governance.
While there was no defined formal space for participation in the delivery of health services in precolonial Uganda, the few existing informal spaces for community participation demonstrate the importance of community participation in decision-making on issues that affect them. However, during colonial times, there was clear subjugation of community participation in Uganda’s governance, which left a legacy that problematized precolonial arrangements; failed to appreciate and uphold the strength of Indigenous systems; created a conflicting situation within Ugandan society; and diminished public trust in health governance. There are still some practices of community joint work through bulungi bwansi that are still visible even in other postcolonial countries such as Rwanda, which takes the form of Umuganda.[62]
The precolonial systems that brought communities together were particularly important for vulnerable groups such as women, who had spaces for addressing their social issues, including health. The introduction of laws such as the Buganda Agreement took away key land resources from the communities, severing their means of welfare and access to the social determinants of health. This agreement also made them subject to royal rule, eroding their autonomy, community systems of health governance, and voice in health decision-making. This marginalized many Ugandans, made them vulnerable to ill-health, and imposed barriers to forming, contributing to, and accessing health care. These challenges continue to exist among landless communities.
The direct importation of British laws and the continued influence of Britain in Uganda’s governance denied Ugandans the opportunity to participate in key decisions that affected their health. Laws were devoid of the legitimacy envisioned by Habermas, and the previous spaces of community participation in precolonial Uganda were eroded. The imposition of a judicial system through the Orders in Council not only undermined the Indigenous justice system but also introduced a judicial system that still adjudicates on right to health cases with procedural complexities. The current legal technicalities that undermine the enforcement of the right to health and limit judicial interpretation of justice issues in the health system at the national level can be traced from the colonial legacy.
A number of colonial laws are still being applied, and while some laws have been amended, a number of them have not been subjected to the discursive test as advanced by Habermas. The most contested aspects of sexual and reproductive health and rights—such as access to safe and legal abortion, sexual orientation, comprehensive sexuality education, access to family planning, and control of venereal diseases—are still regulated through colonial legislation such as the Penal Code Act of 1950 and the Public Health Act of 1935. These laws perpetuate colonial attempts at social control and the degradation of Indigenous community fabrics.
The decolonization process requires that Uganda undertake a legal audit of all its laws and policies to assess them through the lens of human rights and current scientific evidence. The Uganda Law Reform Commission should create public spheres as spaces for discussing the areas of weakness in these laws. The parliamentary lawmaking process should equally have opportunities for people to speak and deliver opinions on aspects that the laws should address. The outcome should be laws that meet the test of legitimacy as guided by Habermas’s views of deliberative democracy.
The current model of delivery of health services is still built largely on the colonial model. Missionary hospitals dominate the provision of health care, delivering care aligned with religious values, which permeate training schools organized by religious groups that were introduced by colonizers.
The colonial period also introduced missionary NGOs that deliver health care through a cost-sharing mechanism that has persisted as part of Uganda’s health system. These NGOs remain a major force in promoting religious-values-based health care delivery and have in many cases openly opposed the implementation of progressive sexual and reproductive health and rights policies. Such efforts have impeded the implementation of a human rights-based approach as part of Uganda’s health governance. Part of the decolonization process would require that Uganda, as a postcolonial country, revisit its NGO policies and ensure a regulatory framework that insulates NGO mission work from a biased model of delivery of health services based solely on religious values. This process could include a deliberate effort to build, support, and include the work of Indigenous NGOs that advance a science- and rights-based approach to health services delivery and advocacy as part of government programming. Such Indigenous NGOs can provide a forum for community participation in the delivery of health services and in decision-making around priorities for the health system.
The current structure of Ugandan health facilities is still rooted in the architecture of the colonial masters, and the upgrading of hospitals and other health facilities has been slow. The division between the delivery of physical health and the delivery of mental health introduced during colonial times continues to be the model today. This separation has led to mental health being undermined and overlooked in mainstream programming. The decolonization process requires that the design and capacities of national referral hospitals, regional referral hospitals, and other health facilities be upgraded from the colonial estimations that were based on Uganda’s population and public health needs then. In undertaking this process, the government should end the practice of making plans and decisions in technical offices without engaging local communities. The design of such health facilities should be infused with ideas of the context-specific needs of the communities where such health facilities are being proposed. This will in many ways help ensure that health facilities are designed for and embraced by the communities they serve.
The colonial training models for health professionals have continued to guide medical training in Uganda. Colonial high schools and post-high school institutions continue to dominate Uganda’s education system. In many of these schools, future health professionals receive training based on religious values that were imposed by colonial governments. The danger of such an approach has been the churning out of health professionals and policy makers who base their decisions on religious values as opposed to science and human rights. The decolonization process requires that the education system be scrutinized through a comprehensive stakeholder consultation process to ensure the maximum participation of all those affected. Impacts of the colonial legacy should be expunged and replaced with the present needs. The various training curricula should be revised and upgraded to address current training needs that result in professionals who base their decisions on evidence- and rights-based approaches. Training of trainers’ modules and workshops should be undertaken to examine the best postcolonial methodologies for training health professionals. Such methodologies should be grounded in contextual needs to ensure relevancy.
Conclusion
In conclusion, for the decolonization of health governance in postcolonial countries, a conceptual framework combining deliberative democracy and the right to health is needed. Decolonization calls for arrangements that strive for community participation, Indigenous ideas, and national sovereignty. This process should also take into account Habermas’s concept of deliberative democracy, which emphasizes the importance of focusing on the tenets of power of speech, legitimacy, and the public sphere.
As part of the conceptual framework grounded in the right to health and deliberative democracy, decolonizing community participation must be premised on the recognition of each person as a valid speaking partner with a unique and valuable knowledge to contribute. Thus, respect for the inherent dignity of persons and self-determination must inform all participatory processes and strategies, and each person’s expertise, experience, and input must be valued. Local ownership and community context should inform decision-making in the health sector. This calls for efforts to examine the history and diversity of the community as important elements for shaping effective and efficient community participation as part of the right to health. Respecting local knowledge, the ability of communities, and their potential is key for decolonizing health systems that are participatory. Overall, participation should go beyond mere consultation and should build community capacity and foster public mobilization and awareness.
This paper has illustrated how Uganda’s history and political context has shaped the nation’s current system of health governance. We have argued that when decolonizing a postcolonial country’s health governance, its health system cannot be divorced from its political setup. It is thus important that the political history is mapped to identify opportunities for operationalizing decolonization in health governance.
This paper has also demonstrated that a combination of deliberative democracy and right to health principles provides both structural and procedural parameters for community participation as part of decolonization in health governance. The application of these standards, however, is highly dependent on the context of each country and community. It is therefore important to indigenize this theoretical framework. We recommend that countries undertaking decolonization strive to embed the principles of the rule of law—including respect for the right to community participation and self-determination—in order to dismantle colonial legacies.
Moses Mulumba, LLB, LLM, MPhil, is the Executive Director of the Center for Health, Human Rights and Development, Kampala, Uganda, and a doctoral researcher at the Faculty of Medicine and Health Sciences, Ghent University, Belgium.
Ana Lorena Ruano, PhD, is an Associate Professor at the Center for International Health, Department of Global Public Health and Primary Care, University of Bergen, Norway, and a researcher at the Center for the Study of Equity and Governance in Health Systems, Guatemala City, Guatemala.
Katrina Perehudoff, PhD, LLM, MSc, is Senior Research Fellow and Co-Director of the Law Centre for Health and Life at the University of Amsterdam, Netherlands; a Post-Doctoral Assistant at the International Centre for Reproductive Health at Ghent University, Belgium; and a Fellow at the Amsterdam Institute for Global Health and Development, Netherlands.
Gorik Ooms, LicJur, PhD, is a Professor in the Department of Public Health and Primary Care, Ghent University, Belgium.
Please address correspondence to Moses Mulumba. Email: mulumba@cehurd.org.
Competing interests: None declared.
Copyright © 2021 Mulumba, Ruano, Perehudoff, and Ooms. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted noncommercial use, distribution, and reproduction.
Acknowledgment
This research benefited from funding from the Flemish Interuniversity Council (VLIR-UOS) and the Belgian Directorate-General for Development Cooperation.
References
[1] M. Mulumba, L. London, J. Nantaba, et al., “Using health committees to promote community participation as a social determinant of the right to health,” Health and Human Rights Journal 20/2 (2018), pp. 11–17; See also Q. Han, B. Zheng, M. Cristea, et al., “Trust in government and its associations with health behaviour and prosocial behaviour during the COVID-19 pandemic,” Psychological Medicine (March 26, 2021).
[2] Mulumba et al. (2018, see note 1).
[3] K. Griffiths, C. Coleman, V. Lee, and R. Madden, “How colonisation determines social justice and Indigenous health: A review of the literature,” Journal of Population Research 33/1 (2016), pp. 9–30.
[4] M. A. Sweet, P. Dudgeon, K. McCallum, et al., “Decolonising practices: Can journalism learn from health care to improve indigenous health outcomes?,” Medical Journal of Australia 200/11 (2014), pp. 626–627.
[5] S. Tamale, Decolonization and Afro-feminism (Ottawa: Daraja Press, 2020).
[7] A. L. Ruano, The role of social participation in municipal-level health systems: The case of Palencia, Guatemala (doctoral dissertation, Umeå University, 2012).
[8] E. Mundel and G. E. Chapman, “A decolonizing approach to health promotion in Canada: The case of the Urban Aboriginal Community Kitchen Garden Project,” Health Promotion International 25/2 (2010), pp. 166-173.
[9] Y. Pringle, Psychiatry and decolonisation in Uganda (United Kingdom: Palgrave Macmillan, 2019).
[10] World Health Organization, Everybody’s business: Strengthening health systems to improve health outcomes (Geneva: World Health Organization, 2007).
[11] A. S. W. Beavis, A. Hojjati, A. Kassam, et al., “What all students in healthcare training programs should learn to increase health equity: Perspectives on postcolonialism and the health of Aboriginal peoples in Canada,” BMC Medical Education 15/155 (2015), pp.166-173.
[12] J. Habermas, “Democracy: A paradoxical union of contradictory principles,” Political Theory 29 (2001), pp. 766–781.
[13] M. Gladwell, David and Goliath: Underdogs, misfits, and the art of battling giants (United Kingdom: Back Bay Books, 2013).
[14] Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4 (2000), para. 54.
[15] B. M. Meier, L. Gable, J. E. Getgen, et al., “Rights based approaches to the public health system,” in E. Beracochea, C. Corey, and D. Evans (eds), Rights-based approaches to public health (New York: Springer Publishing Company, 2010), pp. 19–30.
[16] A. Stilz, “Decolonization and self-determination,” Social Philosophy and Policy Foundation 32/1 (2015), pp. 1-24.
[17] D. Butt, “Colonialism and post-colonialism,” International Encyclopaedia of Ethics (2013), pp. 892–898.
[18] Republic of Uganda, Health facilities inventory (Kampala: Ministry of Health, 2012).
[19] M. M. Widdersheim, “Historical case study: A research strategy for diachronic analysis,” Library and Information Science Research 40/2 (2018), pp. 144–152.
[20] R. M. Byrnes (ed), Uganda: A country study (Washington, DC: Library of Congress, 1990).
[21] Ibid.
[22] S. Neema, Community participation in essential national health research process: Uganda’s experience (Kampala: Makerere Institute of Social Research, 1999).
[23] M. S. M. Kiwanuka, A history of Buganda from foundation of the kingdom to 1900 (New York: Africana Publishing Corporation, 1972).
[24] World Bank, “Traditional medicine in Uganda: Historical perspective, challenges and advances,” Indigenous Knowledge Notes No. 64 (2004).
[25] World Bank, “Traditional medicine practice in contemporary Uganda,” Indigenous Knowledge Notes No. 54 (2003).
[26] J. Habermas, Between facts and norms, contributions to a discourse theory of law and democracy (Cambridge, MA: MIT Press, 1984).
[27] K. Ingham, The making of modern Uganda (Sydney: Allen and Unwin, 1958). See also R. Oliver and G. Mathew (eds), History of East Africa (Oxford: Clarendon Press, 1963).
[28] B. J. Odoki, “The challenge of constitution-making and implementation in Uganda,” in J. O. Onyango (ed), Constitutionalism in Africa: Creating opportunities, facing challenges (Kampala: Foundation Publishers, 2001).
[29] K. S. Rubaraza, A political history of Uganda (Nairobi: Heinemann Educational Books, 1980).
[30] D. A. Law, Fabrication of empire: the British and Uganda’s kingdoms 1890–1902 (Cambridge: Cambridge University Press, 2009).
[31] Ibid.
[32] The Uganda Agreement of 1900. Available at http://www.buganda.com/buga1900.htm.
[33] Mulumba et al. (2018, see note 1).
[34] Uganda Protectorate, Ordinances under the Uganda Order in Council (Entebbe: Uganda National Government Publications, 1915).
[35] P. Mutibwa, Uganda since independence: A story of unfulfilled hopes (New Jersey: Africa World Press, 1992).
[36] Nyali Ltd. v. Attorney General [1955] ALL ER 646.
[37] Center for Health, Human Rights and Development (CEHURD), Prof. Ben Twinomugisha, Rhoda Kukiriza and Inziku Valente v. Attorney General [2011] UGCC 16.
[38] Centre for Health, Human Rights and Development and Anor. v. Attorney General (Constitutional Petition-2011/64) [2015] UGCC 14 (30 October 2015).
[39] K. Asante, “The right to participate: An under-utilised component of the right to the highest attainable standard health,” BMJ Opinion (February 16, 2021).
[40] K. A. Hoppe, “Lords of the fly: Colonial visions and revisions of African sleeping-sickness environments on Ugandan Lake Victoria, 1906–61,” Journal of the International African Institute 67/1 (1997), pp. 86–105.
[41] C. Summers, “Intimate Colonialism: The Imperial Production of Reproduction in Uganda, 1907-1925.” Signs 16, no. 4 (1991), pp. 787-807.
[42] Ibid.
[43] Ibid; Republic of Uganda, The Venereal Diseases Act (2000).
[44] Salvatori Abuki and Richard Abuga v. Attorney General, Constitutional Case No. 2 of 1997.
[45] Hoppe (see note 40), p. 247.
[46] E. Kasimbazi, M. Mulumba, and R. Loewenson, “A review of Kenyan, Ugandan and Tanzanian public health law relevant to equity in health,” EQUINET Discussion Paper Series 63 (2008).
[47] M. Mulumba, J. Nassimbwa, C. Kiggundi, et al., “Access to safe abortion in Uganda: Leveraging opportunities through the harm reduction model,” International Journal of Gynaecology and Obstetrics (2017), pp. 231-236.
[48] C. Abbo, “Profiles and outcome of traditional healing practices for severe mental illnesses in two districts of Eastern Uganda,” Global Health Action 4/1 (2011), pp. 1-18.
[49] Mulumba et al. (2017, see note 47).
[50] R. Sundararajan, J. M. Amumpaire, R. King, et al., “Conceptual model for pluralistic healthcare behaviour: Results from a qualitative study in southwestern Uganda,” BMJ 10/4 (2020).
[51] Republic of Uganda, Uganda Independence Act (1962).
[52] Constitution of Uganda (1962).
[53] L. E. Miller and L. Aucoin, Framing the state in times of transition: Case studies in constitution making (Washington, DC: United States Institute of Peace, 2010).
[54] B. B. Bakamanume, “Political instability and health services in Uganda, 1972–1997,” East African Geographical Review 58 (1998), pp. 58-71.
[55] C. Dodge and P. Wiebe, Crisis in Uganda: The breakdown of health services (Oxford: Pergamon Press, 1985).
[56] S. Scheyer and D. Dunlop, “Health services and development in Uganda,” Rural Africana 11/37 (1981), pp. 37-57.
[57] Ibid.
[58] Republic of Uganda, Uganda plan three: The third five-year development plan 1971–76 (1972).
[59] C. K. Tashobya, F. Ssengooba, and V. O. Cruze, Health systems reforms in Uganda: Processes and outputs (Kampala: Institute of Public Health, Makerere University, 2006).
[60] World Bank (see note 25).
[61] Centre for Health, Human Rights and Development and Anor. v. Attorney General (see note 38).
[62] P. Uwimbabazi, An analysis of Umuganda: The policy and practice of community work in Rwanda (unpublished doctoral thesis, University of KwaZulu-Natal, 2012).