Everaldo Lamprea and Johnattan García
Abstract
This paper explores Colombia’s road toward universal health care coverage. Using a policy-based approach, we show how, in Colombia, the legal expansion of health coverage is not sufficient and requires the development of appropriate and effective institutions. We distinguish between formal and material health coverage in order to underscore that, despite the rapid legal expansion of health care coverage, a considerable number of Colombians—especially those living in poor regions of the country—still lack material access to health care services. As a result of this gap between formal and material coverage, an individual living in a rich region has a much better chance of accessing basic health care than an inhabitant of a poor region. This gap between formal and material health coverage has also resulted in hundreds of thousands of citizens filing lawsuits—tutelas—demanding access to medications and treatments that are covered by the health system, but that health insurance companies—also known as EPS—refuse to provide. We explore why part of the population that is formally insured is still unable to gain material access to health care and has to litigate in order to access mandatory health services. We conclude by discussing the current policy efforts to reform the health sector in order to achieve material, universal health care coverage.
Introduction
During the period 1991-2016, the growth of health care coverage in Colombia has been remarkable, going from 25% of the population covered in 1992 to approximately 96% today. This rapid surge in health care coverage represents a key dimension of the right to health, because access to health care, previously restricted to a minority of Colombians, has increasingly become a matter of basic rights for the majority of citizens. As the Colombian Constitutional Court stated in opinion T-760 of 2008, if the right to health is to be taken seriously, then the government has to guarantee that all Colombians have access to health care without any type of distinctions.
However, as we will explore in this paper, many regulatory and institutional shortcomings of Colombia’s health sector have impeded the fact that all Colombians’ can ostensibly access the same basket of health services. Many inhabitants of poor regions carry a social security card as identification, yet their access to basic health care is very limited. As a result, despite the rapid growth in coverage, thousands of vulnerable citizens are not able to enjoy their right to health care, which was mandated by the 1991 Constitution and the precedent of the Constitutional Court.
This paper starts with a discussion of the 1993 congressional bill that introduced Health Sector Reform (HSR) in Colombia. Widely known as Law 100 of 1993, the reform bill uprooted a failed health system that covered less than 25% of the population. The main objective of the 1993 reform was to achieve universal health care coverage through a comprehensive and mandatory social insurance system in which private, public, or mixed health insurers and providers competed for patients among themselves, and also with state-owned institutions such as the Social Security Institute (ISS or Instituto de Seguros Sociales, privatized and ceased to exist in 2007 as a state-owned health insurer and provider). The principles that guided the 1993 health reform were universal health coverage, efficiency, quality, and equity, as explicitly stated in Article 2 of Law 100 of 1993.
Colombia’s minister of health at the time coined the term “structured pluralism” to describe the reform. According to this model, governmental regulation was the key mechanism for ensuring that the new private, public, or mixed health insurers and health care providers were guided in the direction of public interest.[1]
Much has been written about the shortcomings of the 1993 health reform.[2] The abrupt implementation of the bill brought unintended effects, such as the poor performance of key governmental and regulatory agencies that were unable to rein in private stakeholders like health insurance and pharmaceutical companies.[3]
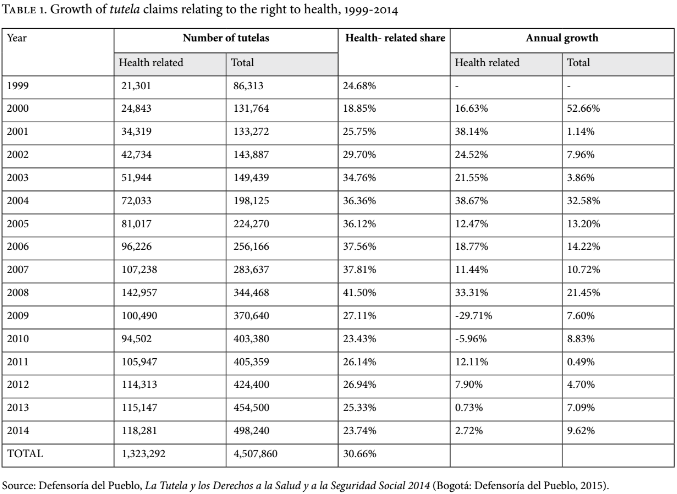
Largely as a result of the regulatory shortcomings in Colombia’s health system, patients who are refused treatments, exams, and pharmaceuticals—whether or not these are included in the baskets of health services—are left with no better alternative than to file a lawsuit using an informal judicial mechanism for the protection of basic rights, widely known as tutela, which was incorporated into the 1991 Constitution.[4] Since the implementation of the 1993 health reform, Colombia has become the most litigious country in Latin America in the area of the right to health.[5] As Table 1 shows, more than 1.3 million lawsuits were filed between 1999-2014 demanding access to health care services, treatments, and pharmaceuticals.[6]
Some authors suggest that the key variable to explain Colombia’s uncommonly high volume of right to health litigation is the institutional arrangement and performance of Colombia’s health system. Yamin et al. argue, for instance, that the “characteristics of the Colombian health system are central to understanding why the volume of litigation has been greater in Colombia than anywhere else.”[7]
Several authors underline that the agenda of international financial institutions like the World Bank was the most important determinant of Colombia’s 1993 health care overhaul.[8] Authors like Yamin stress that the privatization and deregulation of Colombia’s health care system that was unleashed by the 1993 health care reform incentivized health rights litigation. According to Yamin, at the heart of Colombia’s uncommon escalation of right to health litigation lies a clash between the health system’s neoliberal “push toward commodification, commercialization, and privatization [that] undermines both the concept and enjoyment of a right to health” and the reactive role of litigants and courts, which have acted as “bulwarks against the hegemonic onslaught of neoliberalism.”[9]
More concretely, according to this account, Colombia’s implementation of a neoliberal managed competition health care overhaul brought about rapid growth in health care coverage, but also a widespread infringement of patients’ rights, who used the easy access to courts and the highly effective legal mechanisms introduced by the 1991 Constitution to fight off the increased rogue behavior of private health insurance companies. As these companies escalated their infringement of patients’ rights—thanks in great part to the government’s poor regulation of the health system—patients escalated their reliance on health rights litigation. Indeed, patients used litigation consistently as the only effective mechanism to mitigate the harmful effects of privatized/managed competition health care.[10] Furthermore, it was not until 2012 that the government approved integration of the basket of health services for the contributory and subsidized regimes, a change prompted by opinion T-760 of 2008 from the Constitutional Court. From 1993 until 2012, the subsidized population was entitled to fewer health services than the contributory population, which the Constitutional Court ruled an encroachment on the right to equal treatment entrenched in the 1991 Constitution.
Much less has been written about the achievements of the 1993 health reform.[11] Arguably, the most remarkable accomplishment of the reform was the abrupt rise in health care insurance coverage. Over 20 years (1993-2013), coverage jumped from 21% of the population to 96%.[12] This dramatic expansion awarded to most Colombians social security entitlements that were previously restricted to a privileged minority, along with a substantial increase in equity in access and strengthened financial protection for the most vulnerable population.
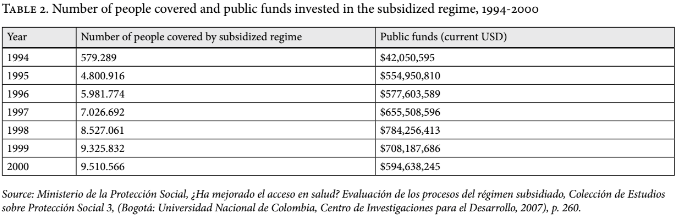
This rapid growth came at great cost to the government. Over the two years that followed the 1993 reform, 4.6 million people were included in the subsidized regime.[13] Public funds committed to subsidize the most vulnerable groups went from US$42 million in 1994 to US$550 million in 1995.[14] Furthermore, although coverage rose rapidly across the country, there were marked inequalities between poor and rich departments in terms of health outputs and access to basic health care.
The dramatic surge in right to health litigation in a context of an abrupt rise in health care coverage indicates that despite the formal or legal expansion of coverage, private insurance companies and public hospitals have denied health care services to hundreds of thousands of Colombians. In the following sections, we explore this gap between formal and material health care coverage and attempt to uncover the main variables driving this phenomenon. We also look at the policies put forward by Colombia’s government to deliver not only formal health care coverage, but also material access to health care to all Colombians. The regulatory reform mandated by opinion T-760 was ultimately crystallized in a statute passed by Congress in 2015 (Law 1751).
Evolution of health care coverage in Colombia, 1991-2013
Setting the foundations, 1991-2003
In 1991, the National Constituent Assembly, a democratically elected assembly in charge of drafting a new Constitution, opened the path for the 1993 health care reform, which introduced from scratch a social insurance scheme for the provision of health services. Colombia’s social insurance model, as outlined by the 1991 Constitution and by Law 100 of 1993, encouraged the regulated competition of private, public, and mixed health providers as a means to accomplish universal health coverage. Yet it was a model that required active governmental intervention and regulation.[15]
As displayed in Figure 1, the Colombian health care system experienced a late and abrupt expansion during the 1990s. By 1993, the social security systems in Costa Rica and Chile offered coverage to approximately 90% of the population, whereas Colombia’s social security system offered coverage to less than 25%. Over a period of 20 years (1993-2013) health care coverage jumped from 21% of the population to 96%.[16]
In 1993—the year health reform was implemented—76% of the Colombian population was uninsured (See Figure 2). By 2015, the percentage covered by the contributory regime, composed of the households of pensioners and citizens who are formally employed and who contributed to the social security system with 12.5% of their salaries, amounted to 45% of the population. The percentage of the population covered by the subsidized regime, composed of the households of the unemployed and informally employed, represented 48% of the population. As a result, only 3% of the population was uninsured by 2015.
As previously mentioned, the touchstone of the 1993 health reform was the creation of two different insurance regimes: the contributive and the subsidized regimes. The contributive regime is funded, primarily, by payroll taxes from formal employees and employers; independent workers who earn more than twice the minimum monthly income; pensioners; and corporate income tax known as the income tax for equality (CREE). Funding for the health insurance companies (EPS) that insure the contributive population and its households comes from the following sources: formally employed Colombians contribute 12.5% of their salaries, retirees contribute 12% of their pensions, and those earning less than 10 minimum monthly wages (approximately US$2,300) contribute 4% of their wages. Members of the contributive regime also help fund the plan through copayments.
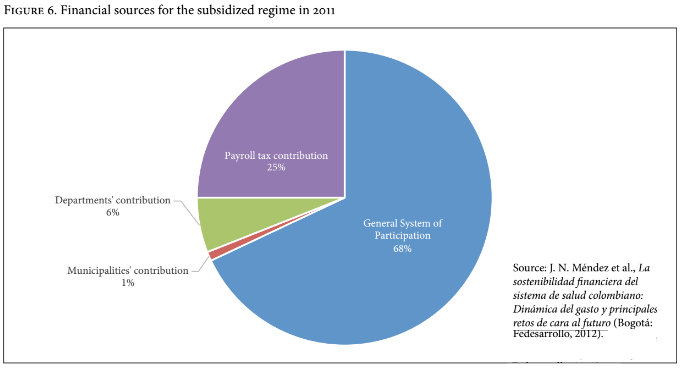
The subsidized regime is financed by public funds, which the national government transfers to municipalities and departments. Once municipalities and departments receive the funds from the national government, they transfer the money to insurance companies that provide health care to the subsidized population. These transfers from the national to local governments are known as General System of Participation (SGP or Sistema General de Participación). Additionally, formal employees, employers, and independent workers contribute 1.5% of their monthly salaries to the subsidized regime through the “solidarity” mechanism of Law 100 of 1993. Finally, municipalities and departments provide funding by means of regional taxes on liquor, tobacco, and gambling, among others.
The early expansion of health care coverage among the subsidized population was bolstered by a 1994 presidential decree (Decree 2491 of 1994), which ordered the national government, municipalities, and departments to create specific subsidies in order to incorporate their poorest citizens into the subsidized regime. A nationally established but locally applied survey, SISBEN, classifies Colombians according to financial need, with the poorest Colombians categorized as SISBEN 1. Those classified as SISBEN 3, although poor, are not as destitute as individuals and families classified as SISBEN 1 and SISBEN 2.
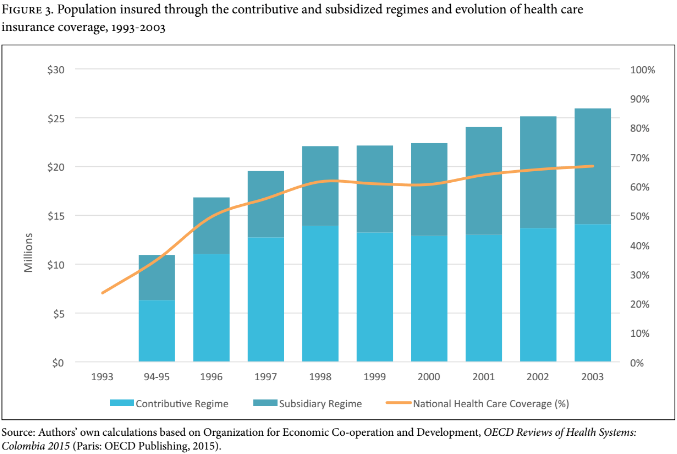
Decree 2491 ordered municipalities and departments to incorporate into the subsidized regime only the population classified as SISBEN 1 and SISBEN 2. As a result of the subsidies created by Decree 2491, more than 5.8 million individuals joined the subsidized regime between 1994 and 1996 (see Figure 3).
However, one of the most important assumptions of the technocrats who designed Law 100 of 1993 was that unemployment and informal labor would decrease over the following decade, resulting in the contributive population growing faster than the subsidized population. Under this assumption, it was expected that the “solidarity mechanism,” whereby the formally employed contribute with 1.5% of their salary, would become the financial bedrock of the subsidized regime. This forecast proved to be wrong, and informal labor and unemployment rose.[17] Over the next 20 years (1993-2013), the subsidized population grew faster than the contributory population (see Figure 3), and as a result, the government had to invest heavily to finance the expansion of health care coverage among the subsidized population.
While in 1994 only 579,289 individuals were part of the subsidized regime, in 2000 the subsidized regime covered more than 9.5 million beneficiaries.[18] As previously mentioned, this expansion cost the government dearly: whereas in 1994 they spent US$42 million financing the subsidized regime, in 2000 they spent US$594 million (see Table 2).
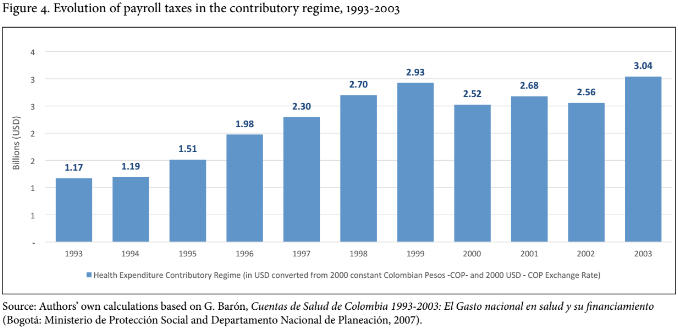
The cost of expanding coverage among the contributive population was also high. However, in this case it was the workforce—formal employees and employers—that shouldered the cost of expanding health care coverage among the contributive population. Whereas in 1993, employees and employers contributed US$1.2 billion through payroll taxes, by 2003 that amount had climbed to US$3 billion (see Figure 4).
Paying the price of universalization, 2003-2013
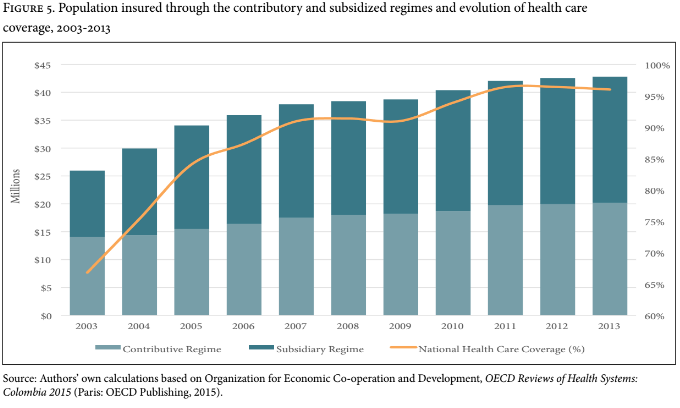
In 2003, health care coverage received an additional boost thanks to an executive order from the health regulatory agency, Consejo Nacional de Seguridad Social en Salud or CNSSS.[19] The order created new governmental subsidies geared towards the incorporation into the subsidized regime of individuals who were classified as SISBEN 2 and SISBEN 3. Starting in 2004, not only the poorest and most vulnerable Colombians—that is, people classified as SISBEN 1—were able to join the subsidized regime, but also individuals who were not as poor and vulnerable. In 2011, the Ministry of Health issued an executive order (Resolution 3778) that reverted the CNSSS 2004 decision, allowing only SISBEN 1 and 2 populations to join the subsidized regime. But as a result of the CNSSS executive order, more than 3.5 million individuals classified as SISBEN 2 and 3 joined the subsidized regime in 2004.[20] As shown in Figure 5, the subsidized population surpassed the contributory population in 2005, a trend that remained constant from 2005 to 2013.
The rapid growth of the subsidized population placed massive pressure on the government’s health budget. In 2011, for example, 68% of the funds used to finance the subsidized regime were public (transfers from the national to the local government through the General System of Participation). Only 25% of the funding came from payroll taxes. Furthermore, municipalities and departments contributed with only 1 and 6% of the funding for the subsidized regime, respectively. (See Figure 6)
From 2003-2009, the average yearly health expenditure for the subsidized regime represented 1.1% of Colombia’s GDP, whereas payroll taxes paid by employees and employers amounted to 2.2%.[21]
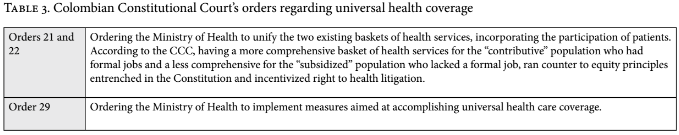
Given these figures, why did the government push forward with the universalization of health care coverage? The answer is not straightforward. One could argue that the government expanded health care coverage among the subsidized population because the 1991 Constitution and Law 100 1993 ordered Congress and the executive branch to achieve universalization. Additionally, in 2008 the Colombian Constitutional Court (CCC) handed down Opinion T-760 of 2008, a 400-page ruling that instantly captured the attention of experts, civil society organizations, patients’ groups, and the media.[22] In Opinion T-760, the CCC reviewed its own vast jurisprudence on the right to health, showing how the evolution of the Court’s precedent led to the conclusion that health care was a basic right which could be autonomously enforced—that is, not only when the right to life of the plaintiff was threatened. Additionally, the CCC concluded that although the right to health created programmatic duties that the government had to comply with gradually, it also created immediate duties for the government.
Opinion T-760/08 contained 32 orders. The first 16 commanded health insurance companies (EPS) to deliver the health care services demanded by the 22 individual plaintiffs who filed the lawsuits. The remaining 16 were addressed to the Ministry of Health and other regulatory agencies, such as the Regulatory Health Commission (CRES) or the National Superintendence of Health. These “structural” orders cover regulatory measures that the CCC considered the government should implement to protect Colombian patients’ right to health. Some deal with the government’s duty to reach universal health coverage and provide a unified basket of health services to both the contributive and the subsidized regimes. (See Table 3)
Although the CCC’s orders may have persuaded the government to strengthen its commitment to universal health care coverage despite mounting fiscal costs, it must also be acknowledged that in previous decades, the Colombian government used health and social subsidies as a populist mechanism to gain votes among the poorest and most vulnerable citizens.[23] Additionally, members of congress and local politicians pressed the executive branch to expand the SGP. According to some researchers, the transfers of public funds from the national to the municipal and department levels transformed the financing mechanisms of the subsidized regime into a source of political grafting and rent-seeking.[24]
Finally, there are indications that part of the population insured by both the contributive and the subsidized regimes have limited or no access to health care. While most of these individuals are formally covered by the health system—that is, they carry a social security card—they often lack material access to health care. In the final section of this paper we explore the gap between formal and material health care coverage, and also discuss policymakers’ efforts to close that gap.
Closing the gap between formal and material health care coverage in Colombia
Uninsured poor population (UPP)
The government has conceded that part of Colombia’s population is still uninsured. More significantly, the Ministry of Health has classified this population as the Uninsured Poor Population (UPP).
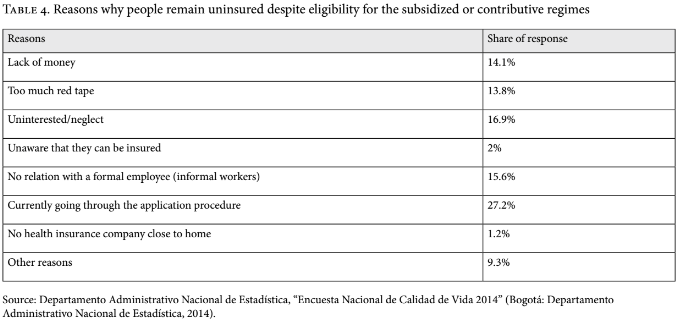
According to recent estimates from the Ministry of Health, 46.4 million people are insured by either the contributive or the subsidized regimes. Official estimates from the government’s statistics agency, DANE, put Colombia’s population at approximately 48.7 million. Thus, according to the Ministry’s data, approximately 2.3 million remain uninsured. However, DANE’s 2014 Quality of Life Survey (Encuesta de Calidad de Vida) suggests that the number of uninsured is larger—approximately 2.7 million people. According to this survey, there are multiple reasons why eligible individuals remain uninsured (See Table 4). Some of the UPP have not been included in the government’s SISBEN. Some people who are in the process of applying for insurance are also part of the UPP. And those individuals who are still uninsured despite being poor enough to qualify for the subsidized regime make up another part of the identified UPP.
Perhaps the most worrying category of UPP is “sandwiched” individuals. The first type of “sandwiched” UPP are those who switch jobs frequently or are short-term contract workers. When they are formally employed, they are insured by the contributory regime, but when they become temporarily unemployed, they abandon it. They cannot be incorporated into the subsidized regime because their changing working status makes them difficult to classify as permanently unemployed or as vulnerable individuals (SISBEN 1 and 2).
Another category of “sandwiched” UPP was created in 2011 when the Ministry of Health issued an executive order (Resolution 3778) excluding SISBEN 3 individuals from the subsidized regime. The Ministry reasoned that SISBEN 3 individuals were not as poor and vulnerable as those classified SISBEN 1 and 2. On the contrary, many had enough income to join the contributory regime as independent workers earning more than two minimum monthly incomes, but they were getting a free ride in the subsidized regime. It is unclear, though, whether the government had solid data on the socioeconomic composition of SISBEN 3 population. Some individuals are currently uninsured because they are considered to be above the poverty line and therefore are expected to join the contributory regime as independent workers. Yet it is possible that the real incomes of these individuals are lower than expected, and thus they are unable to pay taxes as independent workers. As a result, the “sandwiched” population is in a lose-lose situation: excluded from the subsidized regime because they are not poor enough, and unable to join the contributory regime as independent workers because they are not wealthy enough.
Unequal access to health care across departments and regions
Although health care coverage in Colombia is high and equally distributed among departments, there are strong indications that health outcomes and actual access to health services vary dramatically.
Consider, for instance, the performance of health care coverage in the four wealthiest departments vis-à-vis the five poorest departments. According to DANE, Bogotá, Antioquia, Valle del Cauca, and Atlántico have the largest participation in the country’s GDP. La Guajira, Chocó, Amazonas, Vichada, and Guainía are the poorest departments in terms of their participation in the country’s GDP. As Figure 7 shows, the variation of health care coverage among poor and wealthy departments is not marked. On the contrary, a poor department like Guainía has better health care insurance coverage than the two richest Colombian departments.
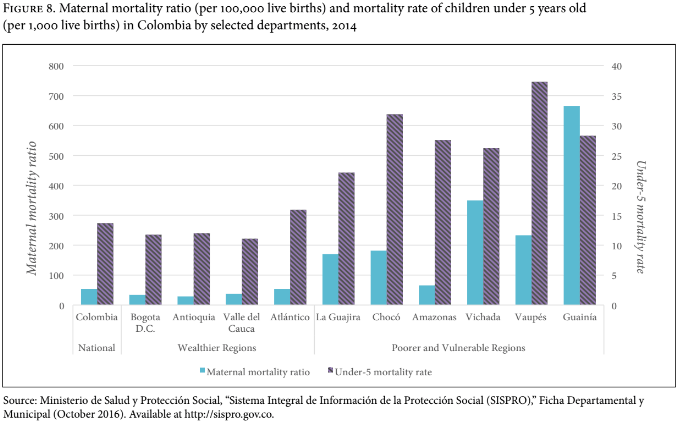
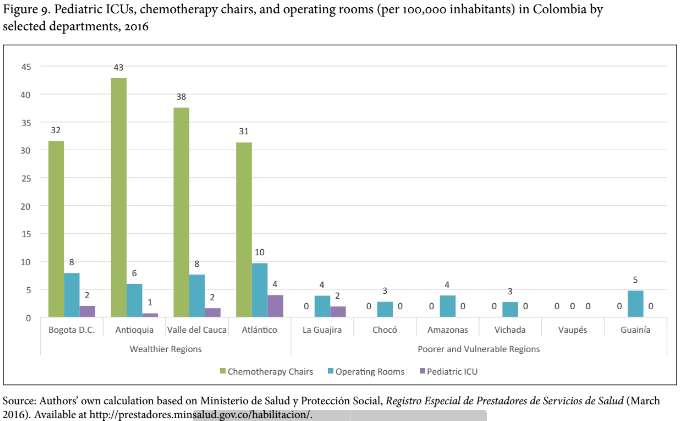
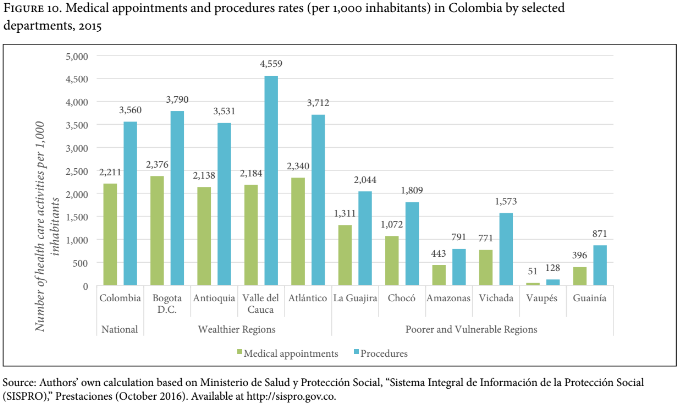
One way to assess the gap between coverage and actual access to health care is by comparing health outcomes and health services between rich and poor departments. We can assess health outcomes, like maternal and child mortality, and health services, such as per capita numbers of health facilities, pediatric intensive care units, operation rooms, chemotherapy units, and ambulances, among others.
Figure 8 shows the different patterns of maternal and child mortality in poor and rich departments. In rich departments, the number of women who die from pregnancy-related causes is, on average, 40 per 100,000 births, whereas in poor departments the figure is 205. Similarly, the number of children younger than 5 years who die per 1,000 live births is, on average, 2.8 times greater in poor departments than in rich ones.
Furthermore, Figure 9 shows major disparities between rich and poor departments in terms of operating rooms (OR). Whereas in rich departments there are on average 8 ORs per 100,000 individuals, poor departments have only 3 per 100,000. The disparities are even greater when it comes to pediatric intensive care units (ICU). La Guajira is the only poor department that has an ICU. Finally, whereas rich departments have, on average, 35 chemotherapy chairs per 100,000 individuals, poor departments do not offer such health services.
Figure 10 shows two health care activity rates (medical appointments and procedures) in each selected department during 2015 (per 1,000 inhabitants). This rate is approximately three times higher in the four richest departments (1,171) than in the six poorest departments (382). Similarly, whereas in the four richest departments 2,254 procedures were performed in 2014 per 1,000 inhabitants, the poorest departments only registered 782 medical procedures per 1,000 inhabitants. The procedure rate in 2015 was three times lower in the poorest departments compared to the richest.
The health disparities illustrated in Figures 8, 9, and 10 suggest a profound gap between formal and material health care coverage in poor departments. In other words, in Guainía most people are formally insured but lack access to basic health services such as operating rooms, pediatric ICUs, and chemotherapy units. Similarly, basic health outcomes like maternal and child mortality are much worse in a poor state like Guainía than in rich departments like Bogotá and Antioquia. In Vaupés, the lack of health service infrastructure and poor health care outcomes collide with the lowest medical appointment and procedures rates in the country.
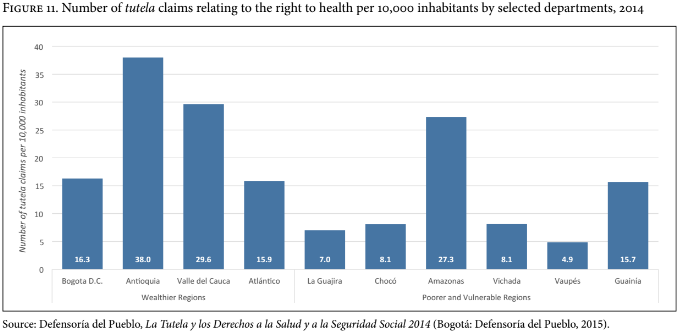
It could be expected that in poor states with low health outcomes levels of health rights litigations would be higher. However, as shown in Figure 11, departments in both wealthy and poor regions share near the same rate of tutela claims relating to the right to health.
Remaining challenges
There are several factors that could account for the great divide in terms of health services and outcomes across the country. Corruption, inefficiency, mismanagement, and institutional weakness seem to be more prevalent in poor departments than in rich ones. The Comptroller General’s office notes that the national government transferred more than $US242 million to 17 departments between 2011 and 2013, to be invested in the improvement of health facilities and hospitals, but the departments only spent $US97 million. Between 2011 and 2013, poor departments like Amazonas, Guainía, and Vaupés received more than $US4 million from the central government to improve their hospitals and health facilities, but for unknown reasons, none of those departments actually used the money.[25]
In 2015, the General Attorney’s office conducted 49 investigations on grafting and widespread corruption in Chocó’s health system. They found that myriad health services were never delivered in Chocó, despite having been paid by local authorities using public funds.[26]
Additionally, weak institutions can also explain why health care is so deficient in departments like Guainía. For instance, in 2014, the Ministry of Health concluded that in poor and distant departments like Guainía, the institutional arrangement for the provision of health care should follow a different blueprint than in the rest of the country.[27] More particularly, providing health care in Guainía, where the population is scarce and dispersed compared to the rest of the country (.56 inhabitants per square kilometer versus 43 inhabitants per square kilometer in the rest of the country), demanded a new health care model capable of achieving five main goals: 1) provision of primary care services adjusted to the real needs of the inhabitants of Guainía; 2) an intercultural model in a region where traditional indigenous knowledge can be incorporated into the local health system; (3) the monopoly of a single health insurer with knowledge and experience in the field, capable of administering scarce resources in a depopulated and vast territory; (4) improvement of existing medical facilities, and creation of new, extramural, and mobile facilities; (5) participation of indigenous communities in the decision-making process.[28] This plan has not been fully implemented in Guainía and it seems there is no course of action for the remaining poor departments. During the past two years, the CCC has exerted pressure on the government regarding the state of Chocó, one of the poorest in the country. According to the CCC, the Ministry of Health has failed to create and implement a policy plan aimed at solving the dire health situation in Chocó. The CCC argued that the government lacks an overarching policy plan to bring health care coverage to the poorest and most vulnerable regions of Colombia.[29]
Conclusions
As some authors have argued, the legacy of Colombia’s 1993 health reform can be summarized in a single phrase: “from few to many.”[30] Undoubtedly, the rapid growth of health care coverage is one of the greatest successes of the 1991 Constitution and of Law 100 of 1993. However, the road toward universal health care coverage over the past 20 years has been uneven, especially for individuals who are formally insured but who lack material access to health care.
Although the government has implemented some policies aimed at closing the gap between formal and material health care coverage, much remains to be done. The government has to improve the mechanisms whereby UPP can be identified and studied. This identification process has to be conducted not only at the central level of government, but also at the regional level. The communication between the Ministry of Health, departments, and municipalities is key to understanding why many individuals across the country are still uninsured.
Furthermore, the government should assess the policy mechanisms to “capture” individuals who are eligible to join the subsidized or the contributive regimes but who are currently uninsured. In the case of the “sandwiched” population, the government should reevaluate, using reliable data, whether excluding SISBEN 3 individuals from the subsidized regime is a step backwards in terms of equity and the right to health.
Although the road towards material, universal health care coverage is still long and uncertain, there are indications that the government and Congress are moving in the right direction. Minister of Health Alejandro Gaviria announced major reforms to the system in September 2012, which Congress finally enacted in 2015 (Law 1751 of 2015). One of the most significant changes wrought by Law 1751 of 2015 is the reversal of the system for identifying covered services and medications. The Law requires that, by the beginning of 2017, the government design and implement a new health benefit plan based on a negative list of non-essential medical services. In the future, all services are to be considered essential, and hence covered by the plan, unless they appear on the negative list of excluded services. Article 15 of Law 1751 establishes that the negative list should be composed of the following categories of treatments: (1) cosmetic or aesthetic, (2) experimental, (3) unregulated and (4) those provided overseas. All other treatments—that is, those not on the negative list—should be considered essential, and therefore must be provided by the government to all Colombians, irrespective of cost.
Furthermore, the CCC ruled that Law 1751 of 2015 was constitutional.[31] The Court held that the minimum-core obligations to provide health care and protect the right to health furthered the principles defined by WHO and General Comment 14, issued in 2000 by the United Nations Committee on Economic, Social and Cultural Rights. For the CCC, the latter document has become an important source of interpretation as the Committee attempted to flesh out the ‘minimum core obligations’ of states with respect to the right to health under the International Covenant on Economic, Social and Cultural Rights. These are duties that “a state party cannot, under any circumstances whatsoever, justify its non-compliance.”[32] According to the CCC, Law 1751 places the protection of the right to health at the center of Colombia’s health system.
Law 1751 and the CCC’s ruling C-324 are good indicators that Colombian policymakers and judges are trying to close the gap between formal and material health care coverage. We are particularly optimistic about the convergence between the right to health and health care coverage in Law 1751. However, the challenges ahead are considerable. If the government and Congress are not able to correct the institutional and regulatory dysfunctions that have plagued the Colombian health system since 1993, the efforts to deliver material universal health coverage will have been in vain.
Everaldo Lamprea, LLB, JSD, is Assistant Professor at University of Los Andes Law School, Bogotá, Colombia.
Johnattan García, LLB, is Clinical Instructor at the Environmental and Public Health Law and Policy Clinic at the University of Los Andes, Bogotá, Colombia.
Please address correspondence to the authors c/o Everaldo Lamprea, Facultad de Derecho, Universidad de los Andes, Bogotá, D.C., Colombia. Email: e-lampre@uniandes.edu.co.
Competing interests: None declared.
Copyright: ©Lamprea and García. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- J. L. Londoño and J. Frenk, “Structured pluralism: Towards an innovative model for health system reform in Latin America,” Health Policy 41/1 (1997), pp. 1–36.
[2]. N. Homedes and A. Ugalde, “Why neoliberal health reforms have failed in Latin America,” Health Policy 71/1 (2005), pp. 83–96; A. Yamin, O. Parra-Vera, and C. Gianella, “Colombia: judicial protection of the right to health,” in A. Yamin and S. Gloppen (eds) Litigating health rights: Can courts bring more justice to health? (Cambridge, MA: Harvard Law School, 2011); A. E. Yamin and O. Parra-Vera, “Judicial protection of the right to health in Colombia: From social demands to individual claims to public debates,” Hastings Int’l & Comp. L. Rev. 33/2 (2010), p. 431; E. Lamprea, “Colombia’s right-to-health litigation in a context of health care reform,” in C. M. Flood and A. M. Gross (eds), The right to health at the public/private divide: A global comparative study, (New York, NY: Cambridge University Press, 2014).
[3]. C. Rodriguez-Garavito, “Justicia y salud en Colombia: Retos y oportunidades creadas mediante la intervención de los jueces,” in O. Bernal and C. Gutiérrez (eds), Libro blanco en salud: Logros, retos y recomendaciones (Bogotá: Los Andes Univ. Press, 2012).
[4]. Lamprea (see note 2).
[5]. O. Moestad, O. Ferraz, and L. Rakner, “Assessing the impact of health rights litigation: A comparative analysis of Argentina, Brazil, Colombia, Costa Rica, India and South Africa,” in A. Yamin and S. Gloppen (eds) Litigating health rights: Can courts bring more justice to health? (Cambridge, MA: Harvard Law School, 2011), pp. 273–304.
[6]. Defensoría del Pueblo, La Tutela y los Derechos a la Salud y a la Seguridad Social 2014 (Bogotá: Defensoría del Pueblo, 2015).
[7]. Yamin et al. (2011, see note 2).
[8]. Homedes and Ugalde (See note 2); T. Groote and J.P. Unger, “Colombia: In vivo test of health sector privatization in the developing world,” International Journal of Health Services 35/1 (2005), pp. 125–141; M.J. Kurtz and S.M. Brooks, “Embedding neoliberal reform in Latin America,” World Politics 60/2 (2008), 231–280; Yamin et al. (see note 2); A. Yamin, “Power, suffering, and courts: Reflections on promoting health rights through judicialization,” in A. Yamin and S. Gloppen (eds) Litigating health rights: Can courts bring more justice to health? (Cambridge, MA: Harvard Law School, 2011), pp. 333–372.
[9]. Yamin (2011, see note 8).
[10]. Yamin and Parra-Vera (see note 2); Yamin et al. (2011, see note 2); Yamin (2011, see note 8).
[11]. A remarkable exception is A. Glassman, M. L. Escobar, and U. Giedion, From Few to Many: Ten Years of Health Insurance Expansion in Colombia (Inter-American Development Bank, 2009).
[12]. Ibid.; J. N. Méndez et al., La sostenibilidad financiera del sistema de salud colombiano: Dinámica del gasto y principales retos de cara al futuro (Bogotá: Fedesarrollo, 2012); Congreso de la República de Colombia, Ley 1450 de 2011: Por la cual se expide el Plan Nacional de Desarrollo, 2010-2014 (2011). Available at http://www.alcaldiabogota.gov.co/sisjur/normas/Norma1.jsp?i=43101.
[13]. Organization for Economic Co-operation and Development, OECD Reviews of Health Systems: Colombia 2015 (Paris: OECD Publishing, 2015), p. 48.
[14]. Ministerio de la Protección Social, ¿Ha mejorado el acceso en salud?: Evaluación de los procesos del régimen subsidiado., Colección de Estudios sobre Protección Social: 3, (Bogotá: Universidad Nacional de Colombia, Centro de Investigaciones para el Desarrollo, 2007), p. 260.
[15]. Londoño and Frenk (see note 1).
[16]. Glassman et al. (see note 11); Méndez et al. (see note 12); Congreso de la República de Colombia (see note 12).
[17]. See, for example, A. Gaviria and M. Henao, “Comportamiento del desempleo en los últimos años y estrategias de los hogares para enfrentarlo,” Coyuntura Económica de Fedesarrollo, (2001), pp. 23–38.
[18]. Ministerio de la Protección Social, ¿Ha mejorado el acceso en salud?: Evaluación de los procesos del régimen subsidiado, Colección de Estudios sobre Protección Social: 3, (Bogotá: Universidad Nacional de Colombia, Centro de Investigaciones para el Desarrollo, 2007), p. 260.
[19]. Consejo Nacional de Seguridad Social en Salud de la República de Colombia, Acuerdo 267 de 2004 (2004). Available at http://jacevedo.imprenta.gov.co/tempDownloads/45D6231459586083463.pdf.
[20]. Ministerio de la Protección Social, Informe de actividades 2004-2005 al Congreso de la República (Bogotá: Ministerio de la Protección Social, 2005). Available at https://www.minsalud.gov.co/documentos%20y%20publicaciones/iinforme%20de%20actividades%20al%20congreso%202004-2005.pdf.
[21]. Méndez et al. (see note 12).
[22]. Judgment T-760 (Constitutional Court of Colombia, Sentencia T-760 de 2008, July 31, 2008). Available at http://www.corteconstitucional.gov.co/relatoria/2008/T-7609-08.htm.
[23]. H. Alviar-García, “Social Policy and the New Development State: The Case of Colombia,” in D. M. Trubek, H. Alviar- García, D. R. Coutinho, and A. Santos, Law and the new developmental state: The Brazilian experience in Latin American context (New York, NY: Cambridge University Press, 2014), pp. 345-368.
[24]. See, for example, A. Gaviria, C. Medina, and C. Mejía, “Assessing health reform in colombia: from theory to practice,” Economia 7/1 (2006), pp. 29–63.
[25]. Contraloría General de la República, Política Pública de Salud PND 2010-2014, (Bogotá: Contraloría General de la República, 2014). Available at http://www.contraloria.gov.co/documents/10136/188941280/01_Salud.pdf/eb57e224-6fdc-4b8b-839e-f25efde60344?version=1.1.
[26]. Fiscalía General de la Nación, Fiscalía Adelanta 49 Investigaciones Por Corrupción En El Sistema de Salud de Chocó (March 2015). Available at http://www.fiscalia.gov.co/colombia/noticias/destacada/fiscalia-interviene-la-corrupcion-en-el-sistema-de-salud-de-choco/.
[27]. Presidencia de la República de Colombia, Decreto 2561 de 2014, 2014. Available at https://www.minsalud.gov.co/Normatividad_Nuevo/Decreto%202561%20de%202014.pdf.
[28]. Ministerio de Salud y Protección Social, MinSalud Presenta Modelo de Atención En Salud Para El Guainía (June 2014). Available at https://www.minsalud.gov.co/Paginas/MinSalud-presenta-modelo-de-atención-en-salud-para-el-Guain%C3%ADa.aspx.
[29]. Revista Semana, El Estado ‘se raja’ por el sistema de salud del Chocó (February 19, 2016). Available at http://www.semana.com/nacion/articulo/corte-constitucional-sistema-de-salud-del-choco-sigue-en-crisis/461215.
[30]. Glassman et al. (see note 11).
[31]. Judgment C-313 (Constitutional Court of Colombia, Sentencia C-313 de 2014, May 29, 2014). Available at http://www.corteconstitucional.gov.co/relatoria/2014/C-313-14.htm.
[32] Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. No. E/C.12/2000/4 (2000). Available at http://www1.umn.edu/humanrts/gencomm/escgencom14.htm.