Antenor Hallo de Wolf and Brigit Toebes
Abstract
The goal of universal health coverage is to “ensure that all people obtain the health services they need without suffering financial hardship when paying for them.” There are many connections between this goal and the state’s legal obligation to realize the human right to health. In the context of this goal, it is important to assess private actors’ involvement in the health sector. For example, private actors may not always have the incentives to deal with externalities that affect the availability, accessibility, acceptability, and quality of health care services; they may not be in a position to provide “public goods”; or they may operate under imperfect information. This paper sets out to answer the question, what legal human rights obligations do states have in terms of regulating private sector involvement in health care?
Introduction
There are many connections between the goal of universal health coverage (UHC) and the state’s legal obligation to realize the human right to the highest attainable standard of health. The right-to-health framework provides a set of legally binding standards directing the state to ensure the availability, accessibility, acceptability, and quality of all health-related services for everyone residing on its territory.[1]
This article focuses on the role of the private sector in the direct provision of health care, the supply of health care-related goods, and health care financing. Private sector involvement in the provision of health care encompasses a complex range of activities carried out by various non-state actors. These actors may include (multi)national companies, nongovernmental organizations, and nonprofit entities. It is important to address private actors’ involvement in light of the aim to achieve UHC. For example, private actors may not always have the incentives to deal with externalities that affect the availability, accessibility, acceptability, and quality (AAAQ) of health care services; they may not be in a position to provide “public goods”; or they may operate under imperfect information. In this article, we take a neutral approach toward this phenomenon, meaning that we assume that private sector involvement is a reality that needs to be addressed as appropriately as possible.
Drawing on existing research and evidence, we first discuss some facts and trends regarding the role of private actors in the health sector. Subsequently, we explore the normative overlaps between UHC and the right to health. We then address the tripartite relationship between UHC, private sector involvement, and the right to health. We explain that based on international human rights law, states are free to choose any mix of public and private involvement in the health sector. Nonetheless, they have a legal “obligation to protect,” based on which they must protect individuals from harmful actions by non-state actors, including those in the health sector. This undertaking results in both substantive and procedural obligations for states, and it embraces the state’s duty to ensure the AAAQ criteria, regardless of whether health care services are publicly or privately provided. In relation to all of the above, we stress the importance of effective monitoring, accountability, and participatory mechanisms.
We identify a human rights impact assessment of the consequences of the (further) involvement of private actors in the health sector. While most obligations identified in this article fall on states, there are also several tentative and progressive obligations for non-state actors in the health sector. However, given that such actors do not have formal legal obligations (for human rights treaties such as the International Covenant on Economic, Social and Cultural Rights are aimed at states), an exploration of these potential obligations falls outside of the scope of this article.
Private sector involvement: Definition, trends, and challenges
Definition
Private sector participation in health care is not a new phenomenon. To the contrary, public and governmental concern in health care appears to have come to the fore only relatively recently.[2] This is certainly the case with respect to health care financing.[3] The involvement of private actors in the provision of health care—whether as direct providers of services (e.g., physicians, pharmacies, and hospitals) or as the providers or manufacturers of materials and technologies used in health care provision—has a long history.
There is no concrete legal definition of private sector participation, and it appears that related concepts, such as public-private partnerships and privatization, are used inconsistently.[4] It is therefore somewhat challenging to precisely define private sector involvement in health care. Given that it is not a passive concept but an actual state of affairs, it seems more reasonable to describe what private sector participation in health care may entail. Such involvement encompasses participation in the health care sector and would thus cover a complex range of activities performed by various types of non-state actors in the health sector.[5] These actors include (multi)national corporations, nongovernmental organizations, private institutions (including charitable bodies and other nonprofit entities), and private individuals, such as general practitioners and consultants. Their roles and activities may include the direct provision of health care, the management of health care institutions, the manufacturing of health care goods and services (e.g., medicines, pharmaceutical products, and rehabilitation), and the financing of health care products and services. These roles and activities may also be carried out within a publicly run health care system. This is the case in the United Kingdom, where private actors have a role in nursing homes for persons with disabilities under the National Health System.[6] They may also take place through public-private partnerships, or in privatized contexts (as discussed below).[7]
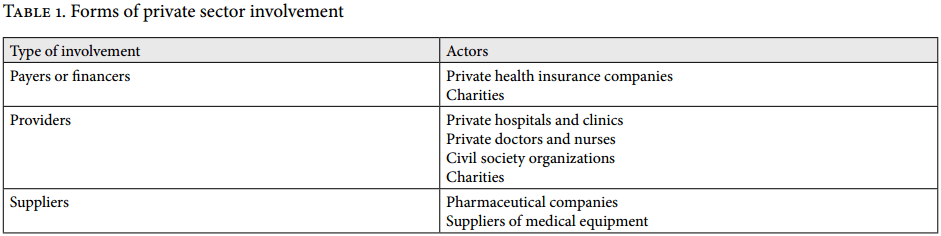
Given the multitude of potential roles and players in the health care sector, this article will focus on only a few of them—the ones we consider to pose relevant challenges with respect to the realization and implementation of the right to health. Thus, our focus will be on the role of (multi)national companies, nongovernmental organizations, and nonprofit entities involved in the direct provision of health care, the supply of health care related goods, and health care financing (see Table 1). These roles may be the result of historical developments (e.g., private actors already operating in health care provision prior to the introduction of a public health care system), privatization, or an increased reliance on public-private relationships. Here it is also important to acknowledge the role of nongovernmental organizations, such as Médicins Sans Frontièrs and religious organizations, in providing health care services within the development or humanitarian contexts in situations in which states are incapable of or unwilling to provide those services. Due to space constraints, however, we will not discuss those contexts here.
For this article, we consider privatization to entail the transfer of the direct provision of health care services or health care financing from public authorities to private actors. This description is based on the definition of privatization provided by the Committee of Ministers of the Council of Europe, which defines it as
- the total or partial transfer from public ownership or control of a public undertaking so that it ceases to be a public undertaking; ii. the transfer to a private person of an activity previously carried on by a public undertaking or public authority, whether or not accompanied by a transfer of property.[8]
There are mixed experiences with privatization from the perspective of the realization of the right to health. In the Netherlands, where a single compulsory health insurance scheme has replaced the dual system of public and private insurance, the now private health insurance companies are obligated to accept every resident in their area of activity and to provide a basic health insurance package that has been designed by the government.[9] While this transition has been moderately positive, in other countries the experience is less so. China, for example, has had to overcome difficulties as a result of its transition to a market economy. In 1984, it reduced the government’s role in the health sector, which caused many health care professionals to lose their public subsidies, while the government exerted little control over the behavior of health care organizations.[10] Many health care workers became “private entrepreneurs,” and the vast majority of the population remained uninsured. Because of these problems, in 2009 the government decided to abandon a market-led health care system and launched a new round of health care reform.[11] By 2011, a government-subsidized insurance system provided modest health coverage to 95% of the population, and an effort to create a primary care system was introduced.[12]
Public-private partnerships in health care, which are distinct from privatization, are another way in which private sector participation can take place. As with privatization, there is no single legal definition of public-private partnerships. The World Health Organization (WHO) and its Legal Counsel describe these partnerships as covering a “wide variety of ventures involving a diversity of arrangements, varying with regard to participants, legal status, governance, management, policy-setting prerogatives, contributions and operational roles.”[13]
Trends and Challenges
Given that private sector participation in health care takes many shapes and involves various kinds of actors, the academic literature on the subject is not conclusive as to whether this participation has a positive or negative impact.[14] There seems to be an increasing reliance on private actors to provide, finance, and supply health care goods and services. In Africa, for example, the International Finance Corporation has found that “the private sector already delivers about half of Africa’s health products and services.”[15] There are various reasons for this: the perceived lack of inefficiency and quality in the provision of public health care, increased costs and reduced budgets for health care due to the 2007–2008 financial crisis, and encouragement by international financial institutions to rely on private actors to decrease the burden on national budgets.[16]Trends and challenges
Some recent studies suggest positive outcomes in terms of private sector participation. For example, with respect to access to health care facilities for childbirth and the treatment of acute respiratory illness, private sector participation in a number of sub-Saharan African countries appears to have led to improved performance in terms of access and equity.[17] However, that particular study notes that its findings were limited since it was unable to measure two very relevant aspects related to health care and the right to health: how much did individuals have to pay to access these facilities, and what was the quality of the care provided?[18] Other studies are more cautious and cannot find overwhelming evidence in favor of or against increased private sector participation.[19] Nonetheless, in health care,[20] there is no consistent manner for measuring the contribution of private actors. In some cases, private sector participation has led to increased costs for patients—for example, through higher out-of-pocket expenses when governments do not cover these costs through subsidies or taxes, or through public insurance coverage—and not necessarily to a more efficient provision of health care.[21] Weak regulatory frameworks appear to be an important problem in this regard.[22]
In terms of the private sector’s involvement in promoting UHC, there is a lot of discussion on what precisely this sector can contribute, given the varying functions it can perform.[23] On the one hand, we should recognize that the private sector may be better placed than the government to deliver certain services and that it is able to make a contribution to health financing. On the other, there is an urgency to uphold the state’s ultimate responsibility for the health of its citizens. Our human rights analysis below offers some suggestions in this regard.
Conceptual overlap between universal health coverage and the right to health
The goal of UHC is to “ensure that all people obtain the health services they need without suffering financial hardship when paying for them.”[24] According to WHO, UHC is a “practical expression of the concern for health equity and the right to health.”[25] This leads us to ask how UHC and the right to health are connected. An identification of the various components of UHC, on the one hand, and the right-to-health framework, on the other, reveals many dense connections between the two.[26] For example, while affordability is a key components of the right to health, it also underpins UHC.[27] In addition, the inclusion of a specific target related to UHC in the Sustainable Development Goals, which emphasizes the provision of quality UHC that is also financially accessible, reinforces the link between UHC and the right to health.[28] Table 2 maps a number of key components of UHC and shows their connection to the right-to-health framework.
Private sector involvement and the right to health
The state’s “obligation to protect” and the AAAQ
Based on the right to health as framed under international and domestic law, states are obliged to ensure timely access to good-quality care for their residents.[30] Governments, as the primary duty bearers, have a responsibility to ensure that health care services (even if privately provided) are available, accessible, acceptable, and of good quality. They must ensure that mechanisms are in place for patients to seek legal redress if they have received inadequate or untimely care. These obligations do not necessarily mean that the state must be the actual provider of health care or that it must maintain a public health system. General Comment No. 3 of the United Nations Committee on Economic, Social and Cultural Rights, adopted in 1990, states that “the undertaking ‘to take steps … by all appropriate means including particularly the adoption of legislative measures’ neither requires nor precludes any particular form of government or economic system” (emphasis added).[31] And it concludes that “the Covenant is neutral and … the rights recognized in the Covenant are susceptible of realization within the context of a wide variety of economic and political systems” (emphasis added.)[32] This indicates that based on the right-to-health framework, governments are free to choose any mix of public and private involvement in the health sector that they consider suitable.
According to the World Bank’s 2004 World Development Report, governments may not necessarily play the role of direct provider of health care services; however, the possibility of market failure calls for governments to play a role in financing, regulation, and information dissemination.[33] In this light, it is necessary to identify the most relevant legal obligations pertaining to the right to health as they relate to the involvement of the private sector. These obligations apply to states regardless of the type or organization of their health care system, and they mean that states must ensure that all actors in the health sector, whether public or private, respect the right to health.[34]
Human rights treaties impose three levels of legal obligations on states: the obligations to respect, to protect, and to fulfill. The obligation to respect requires states to refrain from interfering directly or indirectly with the enjoyment of the right to health; the obligation to protect requires states to take measures that prevent third parties from interfering with guarantees under the right to health; and the obligation to fulfill requires states to adopt appropriate measures toward the full realization of the right to health.[35] The obligation to protect is of particular significance in this context since it requires active monitoring of the activities of third parties. When certain services fall into private hands, there is a shift from the state “respecting” and “fulfilling” the right to a state’s obligation to “protect.”[36] The state is no longer the provider of the service, but now needs to oversee third parties to ensure that they provide this service in an adequate fashion in conformity with the AAAQ framework.
The obligation to protect has also been emphasized by international courts. For example, the Inter-American Court of Human Rights singled it out in Ximenes-Lopes v. Brazil, which concerned the regulation of a private psychiatric clinic in Brazil that participated in the public health scheme set up by the government.[37] The court asserted that under the American Convention on Human Rights, international liability comprises acts performed by private entities acting in a state capacity. In this context, the court referred to the Brazilian Constitution, which recognizes that health care is open to private actors but also identifies the state’s duty to regulate, supervise, and control health programs and services, whether carried out directly or through third parties.[38] The court found that:
States must regulate and supervise all activities related to the health care given to the individuals under the jurisdiction thereof, as a special duty to protect life and personal integrity, regardless of the public or private nature of the entity giving such health care.[39] (emphasis added)
The obligation to protect falls into a number of interlinked duties on the part of the state.[40] It entails four key components: the obligation to regulate all actors in the health sector through the adoption of legislation, regulations, and policies; the obligation to monitor, through independent mechanisms, the behavior of these actors; the obligation to ensure that there is accountability for violations committed by public and private actors; and the obligation to ensure the population’s participation in health care decision-making.[41]
As observed above, the state’s obligation to protect is closely connected to regulation and the AAAQ criteria. As stated in General Comment No. 14, this obligation requires the state to guarantee that private actor involvement in the health sector (referred to as “privatization”) does not negatively affect the AAAQ:
[T]o ensure that privatization of the health sector does not constitute a threat to the availability, accessibility, acceptability and quality of health facilities, goods and services … States should also ensure that third parties do not limit people’s access to health-related information and services.[42]
When it comes to private actor involvement, the question must be addressed whether this involvement negatively affects enjoyment of the AAAQ. For example, in terms of geographic accessibility, the operation of private hospitals should not mean that health services are available only in affluent areas. Table 3 defines a set of questions that can be asked when determining how private actors might be affecting the AAAQ criteria (which also apply to all public actors in the health sector).
Regulation of the private sector as an element of the obligation to protect
As mentioned, regulation is a key tool for dealing with the conduct of actors operating in the health care arena, and it may take various forms, depending on the desired goals.[43] One author’s definition of regulation, which we like due to its resemblance to what the obligation to protect requires in the context of UHC, describes it as “the sustained and focused attempt to alter the behavior of others according to defined standards or purposes with the intention of producing a broadly identified outcome or outcomes, which may involve mechanisms of standard-setting, information gathering and behavior modification.”[44] According to the literature on the subject, many of the rationales for regulation can be ascribed to instances of “market failure”[45]—that is, situations in which “[m]arket imperfections make it impossible for market forces to achieve an efficient allocation of resources.”[46] Since regulation is adopted for various reasons, including compensating for market failure, for the purposes of this article, we will briefly mention two general types of regulation: economic regulation and social regulation.[47] Economic regulation deals with the regulation of monopoly and competition. Social regulation, on the other hand, is concerned with the promotion of social objectives. Christopher Foster provides some examples of objectives that may be served by social regulation, including achieving fairness between various interest groups, redistributing income, and providing a service deemed important by the government, such as health care.[48] For our purposes, it is precisely social regulation that may be of interest in relation to the human rights obligation to protect in the context of health care.
As stated in the definition above, regulation encompasses a “sustained and focused attempt to alter the behavior of others.” Arguably, a proper realization of the obligation to protect also requires a sustained effort by the state to alter or guide the behavior of private entities involved in the health care sector in order to protect human rights, which is one of the main outcomes of social regulation. This requires the fulfillment of certain substantive, institutional, and procedural elements to make social regulation usable as a tool for the implementation of the right to health.[49]
Substantive elements of regulation
Regulatory measures that aim to steer or alter the behavior of private actors operating in this sector should embody the AAAQ framework (see Table 3 above). Thus, with respect to availability, if the state is going to increasingly rely on private actors to provide health care services, regulations should ensure that there are sufficient numbers of providers in the geographical areas where they operate. Regulations should also ensure that private actors do not retreat from particular areas just because they are not, or no longer, financially rewarding.
With regard to accessibility, regulations must guarantee non-discriminating access to private health care facilities. They must further ensure that health care is physically accessible—in other words, that health care facilities are within safe physical reach for all sections of the population. Financial accessibility is also a matter that should be subjected to regulation—for example (and this is related to the issue of financing), by ensuring that private insurance companies offer affordable policies or by providing subsidies to people who would otherwise be unable to obtain indispensable treatment that may be offered by private clinics. When it comes to substantive regulation of the private health insurance market, for example, Neelam Sekhri et al. mention the need for a robust regulatory framework, especially in developing countries where private coverage may be the only form of financial protection available to the population.[50] The authors refer to some countries’ practice of conscripting private insurance to serve the public goal of equitable access.[51] However, they also stress that regulation should not be so restrictive that it “strangle[s] the market.”[52]
Substantive regulation also plays a role in securing the acceptability and quality of health care services provided by private actors. Regulations dealing with medical ethics should be present for both private and public health care providers. Regulations should also require private actors to provide services that are mindful of the different cultures of their patients. National regulatory measures must also aim to ensure that private and public health care providers alike abide by the necessary quality requirements and that their personnel have the required training and certificates.
Arguably, these concerns about substantive regulation also apply to nonprofit organizations. Nongovernmental organizations have increasingly been involved in the delivery of health care, especially in developing countries. Lucy Gilson et al. argue that there should be a strong government presence in coordinating and regulating health care provision by these actors.[53]
Institutional and procedural elements of regulation
Institutional and procedural regulation entail regulatory bodies and procedural rules that allow the state to control and monitor the activities of private actors in the health care sector, thus helping it alter their conduct. This type of regulation requires the establishment of independent regulatory bodies and a venue where those affected by the conduct of health care providers can seek redress.[54] The latter usually includes courts of law, where victims can bring claims against the providers. Given that human rights obligations, as they currently stand, do not directly apply to non-state actors, having an effective avenue for seeking redress for the harmful effects of conduct committed by private entities is of great importance.
Insofar as these regulatory efforts relate to the provision and financing of health care, as well as the manufacturing of health care goods, they must strike a balance between, on the one hand, ensuring the economic efficiency of services and the production of these goods and, on the other, ensuring the protection of the right to health.[55] A World Bank study has identified a number of institutional criteria based on the findings of several studies in order to assess the effectiveness of regulation and regulators for privatized infrastructure and essential services.[56] Arguably, the same approach can be used for the institutional and procedural regulation of private sector participation in health care. First, regulation must be coherent, entailing agreement between the different laws guiding regulation and the elimination of inconsistencies. Coherence with regard to regulators aims at ensuring that the latter have clearly defined responsibilities, and it should require them to publish their goals and reasons for adopting decisions.
Second, effective institutional and procedural regulation requires the regulatory body to be free from political influence; this can be achieved, for example, by establishing a statutory basis for the regulator, free from any ministerial control. It also requires the appointment of regulatory bodies on the basis of professional criteria through open processes involving the participation of key stakeholders, such as health care consumers and patients. Additionally, in order to maintain a regulatory body’s independence, the central government should not be able to easily overturn its decisions. Equally, private sector entities involved should not be able to influence the regulator or its decisions. Third, the regulator must be accountable. Stakeholders should be able to question the reasoning behind the regulator’s decisions, and the latter should be subject to review by courts and other independent, nonpolitical bodies. Inspiration for the creation of independent regulatory bodies in the health care sector could be drawn from the Paris Principles on national human rights institutions.[57]
Obliging the regulator to publish an annual report documenting its activities can also contribute to its accountability, help monitor its efficiency, and guard against corruption. Fourth, transparency is essential for the effective work of the regulator. Its regulatory rules and decisions need to be made public and accessible to all actors with a vested interest: health care providers, financers, the producers of health care goods, and patients. Fifth, the regulator needs to be predictable. This means following the rule of law and basing its decisions on durable rules and procedures. Finally, the regulatory body should be endowed with sufficient financial resources, and its personnel must have relevant expertise.[58] Having stated this, it is important to recognize the difficulties in establishing a proper regulatory framework in practice. Low-income countries with varying degrees of development and respect for the rule of law may face challenges in coming up with proper independent and effective regulatory bodies and procedural regulations. The following section dedicates more attention to the operationalization of such regulation.
Operationalizing the obligation to protect through monitoring, accountability, and participation
Monitoring, which is closely connected to institutional regulation and accountability, means consistently analyzing and overseeing the process of realizing health-related rights. Monitoring can be done both by the state (through independent regulatory bodies and health care inspectorates) and by civil society organizations. The aim of monitoring is to obtain the information that governments need to track their progress toward health-related targets. Quite often, governments and civil society organizations use indicators to measure this progress.[59]
Given the connection between monitoring and institutional regulation, some observations and developments are worth mentioning. A recent trend under international human rights law involves the creation of mandatory national bodies designed to monitor the implementation of human rights treaty obligations. One example includes the national preventive mechanisms (NPMs) that states must establish under the Optional Protocol to the Convention against Torture. These mechanisms are charged with conducting inspections of detention facilities, including psychiatric institutions and hospital wards in which persons are deprived of their liberty. Another example can be seen in the national framework mechanisms that states have to establish under the Convention on the Rights of Persons with Disabilities, which are of great interest to our discussion: states must maintain, strengthen, designate, or establish “a framework, including one or more independent mechanisms, as appropriate, to promote, protect and monitor implementation” of the disabilities convention.[60] These bodies, whether already existing or newly created, are charged with monitoring how states abide by their obligations under this treaty. Arguably, they can fulfill a role in monitoring the conduct of private sector participants in health care.
Again, it is important to acknowledge the difficulty of guaranteeing independent, transparent, and effective regulatory bodies, particularly in low-income countries. At the same time, there are ways to strengthen and improve states’ institutional frameworks to face these challenges. For example, the United Nations Subcommittee on the Prevention of Torture, the international supervisory body established under the Optional Protocol to the Convention against Torture to complement the work of the NPMs, has taken upon itself to help improve NPMs’ mandates, working methods, and awareness of the importance of independence and transparency by offering consultations, cooperation, and advice.[61]
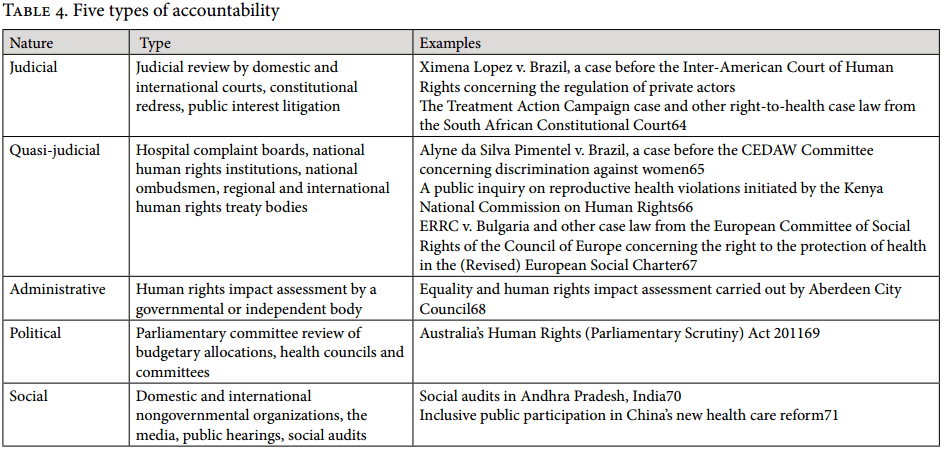
Accountability has also been described as “the process which requires government to show, explain and justify how it has discharged its obligations regarding the right to the highest attainable standard of health.”[62] While the accountability process, to some extent, is about monitoring and evaluating the state’s own actions, the responsibility to provide health care is partly in the hands of other actors, such as private health care providers, private insurance companies, and pharmaceutical companies. In such cases, the state must oversee the actions of these actors. Given the complexity of health systems, a wide variety of accountability mechanisms is required to ensure that the right to health is properly overseen. Based on a comprehensive overview by Potts, Table 4 distinguishes between five different accountability mechanisms and provides examples of ones that can be adopted for ensuring health sector accountability.[63]
The state’s obligations to protect and fulfill in relation to public and private health care financing
As observed above, the private sector can also play an important role with respect to the financing of health care. According to a WHO study, financing plays a threefold role: (i) raising the required resources for health and health care, (ii) removing financial barriers to health care and minimizing the financial risks implied by illness, and (iii) making better use of resources.[72] Although the financing of health care takes place primarily through taxation, private actors also have a role to play. For example, with regard to the first task, private companies or charities can provide financial support to help run the health care system. With respect to the second, private insurance companies can be engaged by the state to facilitate or complement existing public insurance systems. At the same time, however, they could also be an obstacle to this aim if, for example, their insurance premiums are far above what low-income families can afford or if their coverage is insufficient for reducing the financial burdens incurred by persons using the insurance. Here, the obligation to protect plays an important role through the duty to regulate the conduct of private actors involved in or hindering the proper financing of health care systems.
While our focus is on the state’s duty to regulate private actors in the health sector, closely related to this is governments’ responsibility to secure sufficient (public) funding in order to remove financial risks and barriers to access.[73] Financing is also arguably an element of the state’s positive obligation to fulfill in terms of a duty to facilitate the enjoyment of the right to health. The obligation to fulfill is further operationalized when governmental financing is used to directly aid individuals who are unable to enjoy the right themselves due to economic circumstances. Here, for example, one of the state’s roles is to minimize high out-of-pocket payments to public and private providers (which are regarded as an important reason for the lack of proper access to health care) by establishing prepaid and pooling systems of financing.[74] This would also enhance UHC, which, according to WHO, is most closely achieved through “current pooled funds.”[75] Of course, this may depend on an efficient taxation system that helps bolster public finances to feed these funds. A failure to provide adequate financing to health care would imply a violation of the right to health under the International Covenant on Economic, Social and Cultural Rights.
A right-to-health impact assessment for private sector involvement in the health sector
How can the state ensure that private actors in the health sector take the AAAQ framework into account? Several authors have suggested that states should conduct human rights impact assessments prior to the introduction of private sector involvement.[76] These assessments enable states and international and national organizations to assess the possible human rights implications of a certain policy, trend, or development. They are increasingly being used in the context of privatization, new business plans, and trade agreements.[77] For example, Paul Hunt, the former United Nations Special Rapporteur on the right to health, has suggested undertaking a human rights impact assessment of trade-related policies. He argues that such assessments should be conducted at both the international and national level.[78] With regard to health care privatization, he notes that it “should be preceded by an independent, objective and publicly available assessment of the impact on the respective right.”[79]
Drawing from Simon Walker’s study on human rights impact assessments for trade agreements, which in turn is partially inspired by Hunt’s work, we recommend the following steps in order to assess the impact of private sector involvement on the right to health in a given country:[80]
- Step 1 – Identify the relevant legal, economic, social, and regulatory contexts with regard to the right to health; identify the people who will most likely be affected by private sector involvement in health care provision, health care financing, or UHC (e.g., patients in general, vulnerable groups, doctors, medical researchers, providers of ambulance services); and inventory the available goods and services within the health system, including those provided by the private sector.
- Step 2 – Narrow down the various manifestations of private sector involvement in health care and UHC that could have the most significant impact on the enjoyment of the right to health care in terms of availability, accessibility, acceptability, and quality.
- Step 3 – Determine the scope of the assessment by identifying different/future scenarios of private sector participation in the measures to be assessed, and identify the relevant indicators and stakeholders to be consulted.[81] In the context of low-income countries, seek international assistance to address the scope of the assessment and the identification of indicators and stakeholders to be consulted.
- Step 4 – Collect and analyze data to verify the potential impact of private sector involvement in health care and UHC; evaluate the results and determine which of the already identified stakeholders are the most likely to be affected by it; determine whether the accessibility of health care is compromised (Does private sector involvement private sector involvement result in discrimination? Do they maintain a certain affordability in health care?).
- Step 5 – Recommend measures that would lead to or enhance the positive impacts of private sector participation, as well as measures to reduce, ameliorate, or eliminate negative impacts, taking care to consider the acceptability and quality elements of the AAAQ framework.
- Step 6 – Evaluate the general assessment to see if the objectives of the assessment have been met and to examine the extent to which the stakeholders have been consulted. According to Walker,[82] at this stage, a monitoring plan should be adopted in consultation with those stakeholders to keep an eye on actual impacts once the measures regarding private sector involvement in health care, financing, and UHC have been adopted. Arguably, this monitoring plan should consider the AAAQ framework.
- Step 7 – Compile and adopt a report of the assessment that includes an overview of the preceding steps.
Conclusion
The aim of UHC—which is closely connected to the right to health—is for everyone to have access to a full range of good-quality and affordable health services. Countries around the globe have had mixed experiences with regard to private actor involvement in the health sector. The consequences of such involvement should be monitored very carefully.
Human rights law does not interfere with the state’s choice of its health care system—that is, whether it is public, private, or mixed. However, it provides an authoritative set of legal tools for assessing the consequences of private sector involvement. Based on human rights law, governments have an obligation “to protect” the right to health. This means a duty to adopt regulations and other measures to regulate all actors in the health sector. Such regulation should reflect the state’s duty to ensure that health services are available, accessible, acceptable, and of good quality. As we have suggested in this article, governments can be encouraged to conduct human rights impact assessments to assess the consequences of privatization prior to its introduction. We have also briefly asserted that states’ duty to fulfill entails, among other things, an obligation to secure the financing of their health system, such as through taxation and in collaboration with the private sector.
Antenor Hallo de Wolf is Assistant Professor of International Law and International Human Rights Law at the University of Groningen, the Netherlands.
Brigit Toebes is Professor of Human Rights and Health Law at the University of Groningen, the Netherlands.
Please address correspondence to Antenor Hallo de Wolf or Brigit Toebes. Email: a.g.hallo.de.wolf@rug.nl and b.c.a.toebes@rug.nl.
Competing interests: None declared.
Copyright © 2016 Hallo de Wolf and Toebes. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
[1]. Inter alia, UN Committee on Economic, Social and Cultural Rights, General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4 (2000).
[2]. See B. H. Sheingold and J. A. Hahn, “The history of healthcare quality: The first 100 years 1860–1960,” International Journal of Africa Nursing Sciences 1 (2014), pp. 18–22.
[3]. Ibid., pp. 20–21 .
[4]. See L. Clarke, Public-private partnerships and responsibility under international law: A global health perspective (Abingdon: Routledge, 2014), p. 4; A. Hallo de Wolf, Reconciling privatization with human rights (Antwerp: Intersentia, 2011), pp. 19–21.
[5]. For an example of the complex relationships between various actors involved in the provision, reception, and funding of health care in one particular country, the United States, see H. Moses III, D. H. M. Matheson, E. Ray Dorsey, et al., “The anatomy of health care in the United States,” Journal of the American Medical Association 310 (2013), pp. 1947–1964.
[6]. See E. Palmer, “Should public health be a private concern? Developing a public service paradigm in English law,” Oxford Journal of Legal Studies 22 (2002), pp. 663–686.
[7]. See Clarke (see note 4).
[8]. See Council of Europe, Privatisation of Public Undertakings and Activities, Recommendation No. R(93) 7 and explanatory memorandum adopted by the Committee of Ministers of the Council of Europe (October 18, 1993), p. 5. See also Hallo de Wolf (2011, see note 4), p. 21.
[9]. See also W. Schäfer, M. Kroneman, W. Boerma, et al., “The Netherlands: Health system review,” Health systems in transition 12/1 (2010), pp. 1–229.
[10]. D. Blumenthal and W. Hsiao, “Lessons from the East: China’s rapidly evolving health care system,” New England Journal of Medicine 372 (2015), p. 1283.
[11]. Government of the People’s Republic of China, White Paper on Medical and Health Services in China (2012), Part II, “Reform of Medical and Healthcare Systems.” Available at http://www.china.org.cn/government/whitepaper/2012-12/26/content_27520004.htm.
[12]. Blumenthal and Hsiao (see note 10), p. 1283. See also ibid.
[13]. Cited in Clarke (see note 4), p. 5. See also G. L. Burci, “Public/private partnerships in the public health sector,” International Organizations Law Review 6 (2009), p. 361.
[14]. See S. Basu, J. Andrews, S. Kishore, et al., “Comparative performance of private and public healthcare systems in low- and middle-income countries: A systematic review,” PLOS Medicine 9/6 (2012). doi:10.1371/journal.pmed.1001244. See also K. D. Rao, V. Petrosyan, E. Correia Araujoc, et al., “Progress towards universal health coverage in BRICS: Translating economic growth into better health,” Bulletin of the World Health Organization 92 (2014), pp. 429–435.
[15]. See International Finance Corporation, Health care in Africa: IFC report sees demand for investment (December 19, 2007). Available at http://www.ifc.org/wps/wcm/connect/news_ext_content/ifc_external_corporate_site/news+and+events/news/features_health_in_africa.
[16]. Basu et al. (see note 14), p. 2.
[17]. See, for example, J. Yoong, N. Burger, C. Spregn, et al., “Private sector participation and health system performance in sub-Saharan Africa,” PLOS One 5 (2010), p. 2. doi:10.1371/journal.pone.0013243.
[18]. Ibid., p. 8.
[19]. See Basu et al. (see note 14), p. 10.
[20]. Ibid.
[21]. Ibid.
[22]. Ibid. See also K. Hanson, L. Gilson, C. Goodman, et al, “Is private health care the answer to the health problems of the world’s poor?” PLOS Medicine 5 (2008), p. e233. doi:10.1371/journal.pmed.0050233.
[23]. G. Stallworthy, K. Boahene, K. Ohiri, et al., “Roundtable discussion: What is the future role of the private sector in health?” Globalization and Health 10 (2014). doi: 10.1186/1744-8603-10-55.
[24]. WHO, Universal health coverage (UHC): Fact sheet no. 395 (September 2014). Available at http://www.who.int/mediacentre/factsheets/fs395/en.
[25]. WHO, Positioning health in the post-2015 development agenda, WHO Discussion Paper (October 2012), p. 3.
[26]. See also G. Ooms, L. A. Latif, A. Waris, et al., “Is universal health coverage the practical expression of the right to health care?” BMC International Health and Human Rights 14/3 (2014). doi: 10.1186/1472-698X-14-3.
[27]. WHO, Arguing for universal health coverage (Geneva: WHO, 2013), p. 18.
[28]. See target 3.8 of Goal 3 of the Sustainable Development Goals. Available at https://sustainabledevelopment.un.org/sdg3.
[29]. WHO, What is universal health coverage? (December 2014). Available at http://www.who.int/features/qa/universal_health_coverage/en.
[30]. See also J. P. Reading, “Who’s responsible for this? The globalization of healthcare in developing countries,” Indiana Journal of Global Legal Studies 17/2 (2010), p. 386.
[31]. UN Committee on Economic, Social and Cultural Rights, General Comment No. 3, The Nature of States Parties’ Obligations, UN Doc. E/C.12/1991/23 (1990), para. 8.
[32]. Ibid.
[33]. World Bank, World development report 2004: Making services work for poor people, (Washington, DC: International Bank for Reconstruction and Development/World Bank, 2003), p. 33.
[34]. M. San Giorgi, The human right to equal access to healthcare (Antwerp: Intersentia, 2012), p. 44.
[35]. UN Committee on Economic, Social and Cultural Rights (2000, see note 1), paras. 34–37.
[36]. See K. De Feyter and F. Gómez Isa, “Privatisation and human rights: An overview,” in K. De Feyter and F. Gómez Isa (eds), Privatisation and human rights (Antwerp: Intersentia, 2005), p. 3. See also Hallo de Wolf (2011, see note 4).
[37]. Ximenes-Lopes v. Brazil, Inter-American Court of Human Rights, Series C No. 149 (July 4, 2006).
[38]. Constitution of Brazil, arts. 199, 196; ibid., para. 91.
[39]. Ximenes-Lopes v. Brazil (see note 37), para. 85. For an elaborate discussion and other relevant cases, see Hallo de Wolf (2011, see note 4), p. 144.
[40]. B. Toebes and M. San Giorgi, “Dutch realities: Evaluating the Dutch health care reform from a human rights perspective,” in B. Toebes, R. Ferguson, R. Markovic, et al., The right to health: A multi-country study of law, policy and practice (The Hague: Asser Press, 2014), p. 412.
[41]. Ibid.
[42]. UN Committee on Economic, Social and Cultural Rights (2000, see note 1), para. 35.
[43]. A. Hallo de Wolf, “Human rights and the regulation of privatized essential services,” Netherlands International Law Review 60 (2013), p. 184.
[44]. J. Black, “Critical reflections on regulation,” Australian Journal of Legal Philosophy 27 (2002), p. 26.
[45]. R. Baldwin and M. Cave, Understanding regulation: Theory, strategy and practice (Oxford: Oxford University Press, 1999), p. 9.
[46]. C. D. Foster, Privatization, public ownership and the regulation of natural monopoly (Oxford: Blackwell Publishers, 1992), p. 8.
[47]. Ibid., p. 186.
[48]. Ibid.
[49]. Compare with Hallo de Wolf (2013, see note 43), p. 184.
[50]. N. Skhri, W. Savedoff, and S. Thripathi, Regulating private health insurance to serve the public interest: Policy issues for developing countries, WHO Discussion Paper (2005), p. 2.
[51]. Ibid.
[52]. Ibid., p. 6.
[53]. L. Gilson, P. D. Sen, S. Mohammed, et al., “The potential of health sector non-governmental organizations: Policy options,” Health Policy Plan 9/1 (1994), pp. 14–24.
[54]. See also Hallo de Wolf (2013, see note 43), p. 178.
[55]. Ibid., p. 190.
[56]. I. N. Kessides, Reforming infrastructure: Privatization, regulation, and competition (Washington, DC: International Bank for Reconstruction and Development/World Bank, 2004), pp. 82–88.
[57]. See Principles relating to the Status of National Institutions, G.A. Res. 48/134 (1993).
[58]. Kessides (see note 56), pp. 87–88.
[59]. H. Potts, Accountability and the right to the highest attainable standard of health, (Colchester, UK: University of Essex Human Rights Centre, 2009).
[60]. Convention on the Rights of Persons with Disabilities, G.A. Res. 61/106 (2006), art. 33.
[61]. See Optional Protocol to the Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment, G.A. Res. A/RES/57/199 (2002), art. 11(b). See also Office of the United Nations High Commissioner for Human Rights, Outline of SPT advisory visits to NPMs. Available at http://www.ohchr.org/EN/HRBodies/OPCAT/Pages/NoteSPTAdvisoryvisitstoNPMS.aspx.
[62]. Potts (see note 59), p. 13.
[63]. Potts (see note 59). See also D. Brinkerhof, Accountability and health systems: Overview, framework, and strategies (Bethesda, MD: Partners for Health Reformplus Project, 2003). Available at http://www.who.int/management/partnerships/accountability/AccountabilityHealthSystemsOverview.pdf.
[64]. Minister of Health v. Treatment Action Campaign (TAC), Constitutional Court of South Africa, 2002 5 SA 721 (CC).
[65]. Alyne da Silva Pimentel v. Brazil, Committee on the Elimination of Discrimination Against Women, Communication No. 17/2008, UN Doc. CEDAW/C/49/D/17/2008 (2008).
[66]. Federation of Women Lawyers–Kenya and Center for Reproductive Rights, Failure to deliver: Violations of women’s human rights in Kenyan health facilities (New York: Center for Reproductive Rights, 2007), pp. 40–43.
[67]. ERRC v. Bulgaria, European Committee of Social Rights, Complaint No. 46/2007.
[68]. Available at http://www.aberdeencity.gov.uk/council_government/equality_and_diversity/eqd_ehria.asp.
[69]. United Nations Development Programme, Reflections on social accountability (New York: United Nations Development Programme, 2013), p. 37.
[70]. See also ibid., p. 97.
[71]. M. Changshan, “Gonggongzhengce Hefaxing Gongjijizhiyuzouxiang [The transformation of the legitimacy supply mechanism of public policy],” Faxue Yanjiu [Chinese Journal of Law] 34/2 (2012), p. 20.
[72]. WHO, The world health report 2010: Health systems financing (Geneva: WHO, 2010), p. 3.
[73]. Ibid., p. xiv.
[74]. Ibid., pp. 4–6, 41–44.
[75]. Ibid., p. 12.
[76]. P. Hunt, UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, Report of the Special Rapporteur, Mission to the World Trade Organization, UN Doc. E/CN.4/2004/49/Add.1 (2004), paras. 54–56; B. Toebes, “Taking a human rights approach to health care commercialisation,” in P. Cholewka and M. M. Motlagh (eds), Health capital and sustainable socioeconomic development (Boca Raton, FL: Taylor and Francis, 2008), pp. 441–458.
[77]. See S. Walker, The future of human rights impact assessments of trade agreements (Antwerp: Intersentia, 2009).
[78]. Hunt (2004, see note 76), paras. 54–56.
[79]. P. Hunt, “The international human rights treaty obligations of state parties in the context of service provision,” in Day of general discussion on the private sector as service provider and its role in implementing child rights, UN Doc. CRC/C/121 (2002), pp. 4–5.
[80]. Walker (see note 77), pp. 86–102.
[81]. Ibid., pp. 86, 93.
[82]. Ibid., pp. 86, 101–102.