Isabel Goicolea , Miguel San Sebastián, and Marianne Wulff
Health and Human Rights 10/2
Published December 2008
Abstract
Despite advances made by Ecuador in developing policies on reproductive and sexual rights, implementation, and oversight remain a challenge, affecting in particular those living in the Amazon basin. This paper reports on an evaluation of sexual and reproductive health and rights (SRHR) in Orellana, Ecuador, the basis of which was the Health Rights of Women Assessment Instrument, which was altered to focus on government obligations, the reality of access and utilization of services, and the inequities and implementation challenges between the two. A community-based cross-sectional survey conducted in 2006 served to document the current status of SRHR. Local female field workers interviewed 2,025 women on three areas of women’s reproductive health: delivery care, family planning, and pregnancy among adolescent girls age 10–19. The results suggest a reality more dismal than that of the official information for the area. Skilled delivery care, modern contraceptive use, and wanted pregnancies were conspicuously lower among indigenous women living in rural areas. Access to reproductive health services varied between rural and urban women. These significant differences in care — amongst others documented — raise concerns over the utility of national-level data for addressing inequities. The gaps evident in the validity of available information for monitoring policies and programs, and between national policy and action reveal that much still needs to be done to realize SRHR for women in the Amazon basin, and that current accountability mechanisms are inadequate.
Introduction
In an address to the Fifth Asian and Pacific Population Conference, held in Bangkok in December 2002, the then-Secretary General of the United Nations, Kofi Annan, remarked that:
the Millennium Development Goals, particularly the eradication of extreme poverty and hunger, cannot be achieved if questions of population and reproductive health are not squarely addressed. And that means stronger efforts to promote women’s rights and greater investment in education and health, including reproductive health and family planning.1
As this often-cited statement emphasizes, reproductive and sexual health is an urgent public health priority among poor and socially marginalized communities, and a matter of human rights. Reproductive hazards do not randomly select individuals; disparities between rich and poor are more evident in reproductive health and preventable maternal deaths than in any other area of health care.2 At the 2005 World Summit, the Millennium Development Goals (MDGs) were expanded, and signatory governments committed to work toward universal access to reproductive and sexual health care by 2015.3 A rights-based approach to reproductive and sexual health indicates that responsibility does not merely fall on individuals to behave safely, but also on governments to ensure the availability, accessibility, acceptability, and high quality of related services.4 Furthermore, a human rights paradigm affirms the freedom of individuals to make choices about their reproductive and sexual lives.5 True universal access will be possible only when the needs of vulnerable groups are prioritized, and when specific interventions to close discrimination-based disparities are implemented.6 This paper reports on the gaps and challenges to sexual and reproductive health and rights (SRHR) that we identified using a model based on the Health Rights of Women Assessment Instrument (HeRWAI) in a study done in 2006 in the province of Orellana in the Amazon basin of Ecuador.
Despite Ecuador’s policy initiatives, access to reproductive and sexual health services throughout the country remains poor, with marked inequities evident. The disempowerment of women often impedes their exercise of reproductive and sexual rights.7 For example, 25% of the country’s deliveries occur without skilled attendants; this indicator rises to 40% for women living in the Amazon basin. Limitations in access to contraceptives are also evident in the fact that, nationally, women identify almost 20% of pregnancies as unwanted; for the Amazon basin this figure rises to 26%.8 The existence of a policy does not ensure its implementation, and these data document the necessity for improvements in government accountability that will allow citizens to identify where and when a signatory state or a treaty progresses (or fails to progress) in achieving its goals, to denounce violations, and to obtain restitution.9
The effectiveness of Ecuador’s health system — including its general policies on reproductive and sexual health — is measured every four years by a demographic and maternal-child health survey, the “Encuesta Demográfica y de Salud Materno Infantil,” or ENDEMAIN, a national survey of women ages 15 to 49. However, ENDEMAIN’s sample for the Amazon basin is small (a total of 542 women, or approximately 0.5% of all women in this age range), and the survey seldom reaches isolated communities.10 It is doubtful that the situation in these areas has been adequately measured by the national government. Accurate information and data are essential in order to address inequities, especially for those places and populations where the exercise of sexual and reproductive health rights is weak and most vulnerable.11
Assessing sexual and reproductive health in Ecuador using HeRWAI
Our study in Orellana gathered data on reproductive health indicators (delivery care, contraceptive use, and adolescent pregnancy) from both a local community-based survey and from official and policy sources for use with the Health Rights of Women Assessment Instrument (HeRWAI).12 HeRWAI is a tool designed to obtain a measurable comparison between what is actually happening and what should be happening according to a country’s human rights obligations. HeRWAI was explicitly developed to enhance lobbying activities for improving the implementation of women’s health rights and is based on the consensus statements of the Conference for Eradication of Discrimination Against Women (CEDAW) and the International Covenant on Economic, Social and Cultural Rights (ICESCR). HeRWAI is structured into six steps:
- Step 1 describes the policy and rights involved;
- Step 2 examines government commitments by looking at national and international agreements, policies, and laws relevant to the studied policy;
- Step 3 describes the capacity to implement the policy (resources, enhancing factors, and barriers);
- Step 4 analyzes the impact of the policy, focusing on women’s health rights;
- Step 5 establishes state obligations; and
- Step 6 develops recommendations and strategies based on analysis of the previous steps.13
We modified HeRWAI to focus on three stages. First, to look at “what should be happening,” we performed a literature review of governmental and international documents, laws, and programs, including Ecuador’s National Policy of SRHR and its stated commitment to this issue. Second, we assessed “what is actually happening” regarding SRHR in Orellana, based on data gathered locally with the community-based cross-sectional survey during 2006, and compared this to the status of SRHR in the Amazon basin depicted by official data from the most recent ENDEMAIN (that of 2004). Third, we highlighted the gaps between national policy commitments and the realities of local communities, with particular attention to the leading implementation challenges for this region of Ecuador.
Study location and population
Orellana is a province with 103,032 inhabitants, containing 22,500 square kilometers of rainforest; its population is primarily rural (there are approximately 450 rural communities), with only 30% of the total population of Orellana living in urban areas. The province is divided into four counties. For this study, two settlements were considered to be urban areas: the capital, Coca, with approximately 20,000 inhabitants, and Sachas, with 7,000 inhabitants. In the rural areas, people usually live in small communities that range, on average, from 300 to 500 people. Houses in these communities are typically separated by some distance, and each community has a small center where the school is based. Thirty percent of Orellana’s population is indigenous, mainly Kichwa. Almost 50% of the population is under age 15, and adolescents (ages 10–19 for this study) make up 27% of the population.14
Responsibility for public health in Orellana lies with the Ministry of Health’s provincial department. There is a small, 20-bed hospital in Coca, three health centers based in the largest towns, and small health facilities in rural areas. Community health workers work on a voluntary basis in approximately 100 of the most remote areas.15 Emergency transport is difficult. When patients cannot be treated at the provincial hospital, they are referred to the capital city, Quito, 350 km away. Some local governments (two of the province’s four counties, Orellana and Sachas) assume transportation costs for patients, but this is not true in every case.16
Our study population consisted of women between 10 and 44 years living in the province of Orellana. The women were identified through an ongoing community-based cross-sectional survey that was conducted in the province between May and December, 2006. The selection of women followed a two-stage cluster sampling procedure.17 The final sample consisted of a total of 2,025 women from 1,631 households: 524 from indigenous communities and 1,107 from non-indigenous communities.
Data for the Orellana survey was collected by female field workers who visited each household in the selected community. Information was obtained using a two-part questionnaire. The first part recorded household socioeconomic and demographic information. For socioeconomic characteristics, an index was constructed using information from the household characteristics (materials used for roof, floor and walls construction, source of water, and sanitation). The index variables were adapted from the Ecuadorian National Census Questionnaire. The second part was administered only to women age 10–44, and obtained information on fertility, all pregnancies each woman had experienced, contraceptive use, infant mortality, delivery care, and pregnancy intention.18 Urban women accounted for 33.6% (679), rural non-indigenous for 35.2% (713), and rural indigenous for 31.4% (633). Because indigenous women living in urban areas represented a minority, we decided not to split urban women into two groups according their ethnic origin.19 Mean age of interviewed women was 23.5 years, with little variation between groups living in different areas. Regarding civil status, 54.4% (1,047) were married or in a formal union and 43.3% (865) were single.
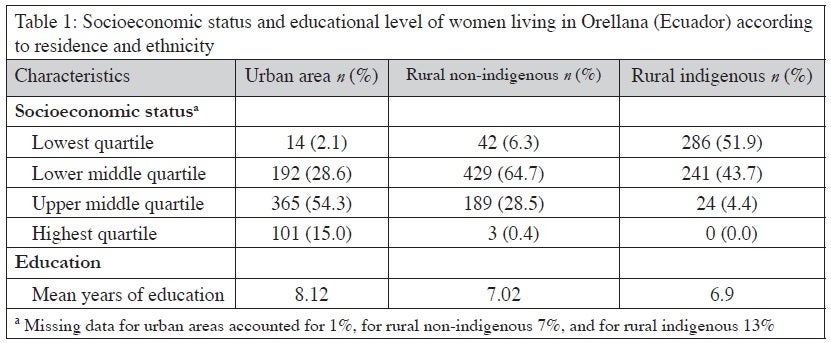
Socioeconomic status and educational level by area are shown in Table 1 (see below). Inequities prominent in Table 1 include those between urban and rural areas and, within the rural areas, between indigenous women and the others.
What should be happening? Sexual and reproductive health policy in Ecuador
Ecuador’s National Constitution of 1998 was the first in Latin America to include reproductive and sexual rights.20 In 2005, the government adopted a National Policy of Sexual and Reproductive Health and Rights (SRHR) [“Política Nacional de Salud y Derechos Sexuales y Reproductivos”] that is rooted in human rights principles.21 The objective of the policy is to encourage and expand the exercise and fulfillment of reproductive and sexual rights. The policy acknowledges concepts such as individual freedom and entitlement to a system of health protection.
Prior to adoption of the National Policy of SRHR, several laws had been passed related to SRHR issues in Ecuador. Among them, the law for free maternity and infant care (“Ley de Maternidad Gratuita y Atención a la infancia,” or LMGYAI) marked a first step toward universal health coverage. The LMGYAI states that in addition to maternal and child health care, all services related to reproductive health should be free of charge, including contraceptive counseling, screening for cervical cancer (but not treatment of cervical cancer or intraepithelial neoplasias), as well as laboratory tests and treatment for sexually transmitted infections.22 The LMGYAI also establishes sources of funding and a mechanism for assigning money to health departments according to the number of patients who attend the health centers and the severity of the conditions in patients seen.23 However, health departments criticize that funds usually arrive very late, and the amount of money they receive is not enough to cover the drugs and supplies used. The law identifies that it is the responsibility of local governments to ensure transport for specific medical emergencies related with obstetric or neonatal emergencies, such as postpartum hemorrhage, eclampsia, puerperal infection, spontaneous abortion, or obstructed labor. Mechanisms are lacking to monitor whether all local governments fulfill their responsibilities or whether the interpretation of this responsibility is most useful in specific situations (for example, providing a car-ambulance in places where a high number of communities are reached by boat).24 Accountability and community participation take place through users committees, which are composed of women who volunteer. Users committees measure quality of services (by applying exit questionnaires to women who attend the hospital for prenatal checkups, and delivery), follow up reported violations, and discuss with health authorities the implementation of the law within their communities. However, the law does not establish mechanisms for funding committee activities, which include, for example, travelling to the hospital to apply the questionnaires, attending meetings with authorities, maintaining an office in which to receive reports of violations, and the time and resources to follow them. In Orellana, local governments and NGOs have devoted resources for such activities, but sustainability is not ensured.25
Currently, SRHR policy implementation is monitored by the National Commission for Reproductive and Sexual Health and Rights, which consists of 17 member institutions including public institutions (e.g. the Ministry of Education, Ministry of Health, and the Women´s Council), representatives of NGOs and non-profit organizations, and representatives of the civil society. The Action Plan for SRHR was elaborated by the National Commission based on the National Policy and it includes nine different programs.26 Three programs are most relevant to our study: prevention of maternal mortality, family planning, and the adolescent program. The maternal mortality reduction program focuses on the provision of Emergency Obstetric Care (EmOC) services, strengthening the LMGYAI, and reducing barriers to skilled delivery care with attention to issues of intercultural sensitivity. The family planning program seeks to reinforce the sexual education program in schools, and to ensure the availability and accessibility of family planning services, focusing on the most vulnerable populations.27 The adolescent program focuses on “adolescent-friendly health services,” emphasizing three issues: sexually-transmitted infections, HIV and AIDS, and adolescent pregnancy. Each program establishes objectives, activities, and indicators for its activities. However, the Action Plan does not set goals or targets, and responsibility for implementation of programs and activities is not clearly established. In addition, the Action Plan document does not discuss resources for policy and program implementation.
What is happening? The reality of sexual and reproductive health in the Amazon Basin
In Orellana, available resources to implement the three programs relevant to our study are limited. Regarding the provision of emergency obstetric care, there is only one facility providing comprehensive emergency obstetric care in the capital city, Coca, and a shortage of beds and blood supplies make referrals to other provinces common.28 The large geographic area and low population density (4.5 inhabitants per square kilometer) of the province, along with the poor communication system (many communities are only accessible by canoe or by foot) make it impossible to ensure that every woman delivers at less than two hours from a facility providing EmOC.
Provision of contraceptive methods is included within the LMGYAI. Health facilities in Orellana, from the provincial hospital to the smallest rural health centers, have contraceptives available. Hormonal methods and condoms are also distributed at the majority of the community health posts served by community health workers. However, pitfalls in the supply distribution system can at times make the absence of some methods common, affecting the quality of the service. Female sterilization is only available at the provincial hospital. Male sterilization is minimal. IUD insertion and removal is only performed at the provincial hospital and, occasionally, at some urban health centers.
There are no youth clinics in Orellana and adolescents’ access to reproductive and sexual health services within the public sector is difficult. A youth center exists in the capital, Coca, where information, condoms and emergency oral contraception are provided by peer educators. The majority of secondary schools are implementing sexual education. However, health services within the schools or partnerships between schools and nearby health centers for offering reproductive health services are lacking. After a strong campaign promoting the right for adolescent students to remain at school, explicitly stated in the Adolescents National Code, it is now rare that schools prohibit a pregnant student from continuing her education.29 However, the majority of schools do not make special arrangements to help pregnant girls continue their education during pregnancy and motherhood.
Delivery care
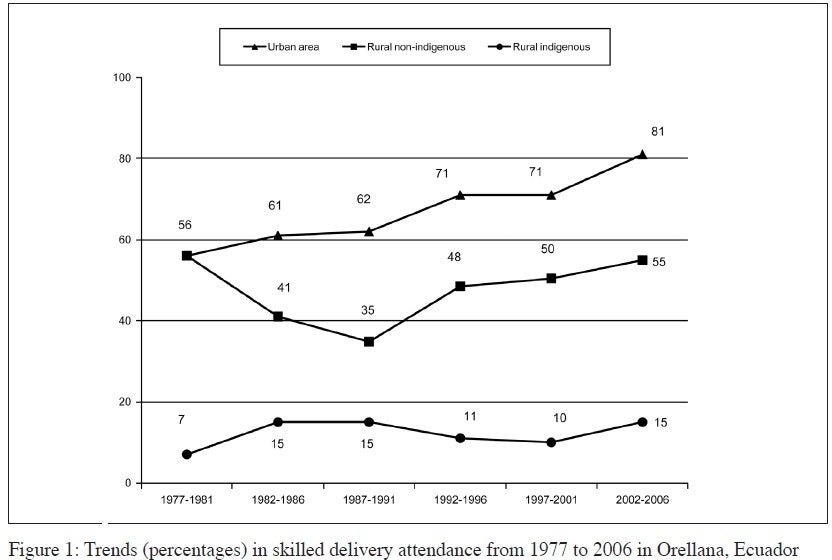
The presence of skilled attendants at delivery, which is essential for the management of obstetric emergencies, is a well-accepted practice to decrease maternal and infant mortality and morbidity.30 Data from Orellana between 1977 and 2006 demonstrates marked discrepancies in skilled delivery attendance between urban, rural non-indigenous, and rural indigenous populations. While skilled delivery attendance in urban areas rose from 56% to 81% between 1977 and 2006, its prevalence in rural non-indigenous women has remained largely unchanged (56% vs. 55%), while that of rural indigenous women is abysmal, even though it rose from 7% to 15% (see Fig. 1 below). The resulting provincial mean during the 2002–2006 period was 47%, which suggests a very different picture of the actual situation than that suggested by the official ENDEMAIN data, which reports 74.2% for the country and 60.9% for the Amazon basin.
Family planning
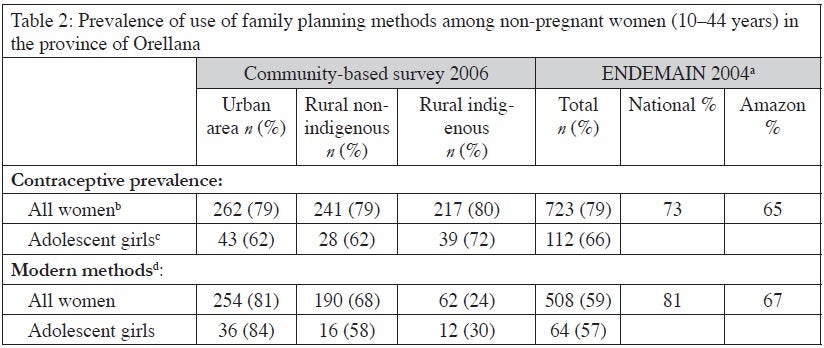
The percentage of women who use contraceptives are similar in all groups (79% for urban women, 79% for rural non-indigenous and 80% for rural indigenous) and even higher than ENDEMAIN´s data (73% for the country and 65% for the Amazon). However, use of modern methods shows wide differences, both between local data (59%) and ENDEMAIN´s data (81% for the country and 67% for the Amazon) and, locally, between different groups. Indigenous women are more likely to use the rhythm method (65%) and herbal remedies (9%) as contraceptives, while non-indigenous women preferred methods such as hormonal contraceptives (53% for urban women and 43% for rural non-indigenous). Condom use is very low (1.3% for all women and 2.7% for adolescent girls) (see Table 2 below). Not surprisingly, the highest proportion of unwanted pregnancies was found among rural indigenous women (43.6%), compared with 30.6% for rural non-indigenous women and 29% among urban women. Again, these findings differ starkly from the “official” ENDEMAIN findings in 2004, of 18.7% unwanted pregnancies nationally, and 25.9% for the Amazon.
Pregnancy among adolescents
Of the 2,025 women in the sample, 41% (828) were adolescents. Half of them belonged to the 10–14 age group and half to the 15–19 age group. Thirty-two percent (266) were urban, 37.1% (308) were rural non-indigenous, and 30.8% (256) were rural indigenous. Measuring civil status, 19.8% (162) were married or in a formal union. For the youngest girls (10–14) only 2.2% (9) were in a formal union, while for those 15–19 years of age, 37.4% (155) were in formal unions.
Of all the adolescents, 19.7% (164) have experienced pregnancy: 2.2% (9) of those ages 10–14 and 37.4% (155) of those ages 15–19. In the urban area, 26.7% (71) of all adolescents were or had been pregnant, while this proportion was lower in the rural area: 16.4% (50) among non-indigenous and 16.8% (43) among indigenous girls. For the oldest adolescents (15–19) proportions rose especially in the urban area, where 45.5% (69) had experienced pregnancy, while in rural non-indigenous communities numbers drop to 31.3% (46), and among rural indigenous the prevalence was 35.1% (40). Information regarding contraceptive use among adolescent girls is shown in Table 1.
The adolescent group accounted for the highest proportion of wanted pregnancies (44.9%) among all age groups of women surveyed. When disaggregated by residence-ethnicity, the proportion of wanted pregnancies among urban adolescent girls was slightly lower (40%) than among their adult counterparts (42%). Numbers were the opposite among women living in rural communities. For non-indigenous: 56% of pregnancies among adolescents vs. 40% for adults; for indigenous: 50% for adolescents vs. 28% for adults. Adolescent girls reported a higher proportion of deliveries attended by skilled professionals than their adult counterparts (59% for adolescents vs. 47% for all women). Yet the survey findings show that even these statistics remain well below that of the ENDEMAIN report of 2004 (77.8% for adolescents and 74.2% for all women).
Discussion of inequities and disparities
Results of the survey showed that women in Orellana face poorer reproductive health indicators (expressed by lower proportions of wanted pregnancies and skilled delivery attendance) than women living in other areas of the country. There were wide inequities within the province: urban women had higher proportions of skilled delivery attendance, wanted pregnancies, and modern contraceptive use compared with rural women. Among rural women, indigenous women had the lowest proportion of skilled delivery care and the highest proportion of unwanted pregnancies. These provincial discrepancies, as well as those notable in the differences between official data and locally gathered information, merit further attention; accurate and relevant data are essential in order to monitor implementation of the National Policy on sexual and reproductive health and rights.
Delivery care
In Orellana, less than 50% of deliveries between 2002 and 2006 were attended by skilled personnel. It was encouraging to see an improvement since the 1970s, especially among women living in urban areas (55.6% in the 1977–1981 period versus 81% in the most recent data). Yet the gaps between urban and rural women remain wide, as do differences between indigenous and non-indigenous women living in the same rural areas (55% for rural non-indigenous and 15% for rural indigenous). Disparities between urban and rural care might reflect inequity in access to services, which remain concentrated in the largest towns. Access may also be complicated by distance, transportation difficulties, and the availability of hospital beds, professionals, or supplies once women actually reach health facilities.31 Yet the accessibility barriers among rural women, indigenous women, those with the least skilled attendance at delivery, may be related not only to distance (since non-indigenous and indigenous communities are found in similar geographical locations), but also to cultural issues.
Although the National Policy brings attention to issues of interculturality, health facilities and health personnel might not receive training in these issues, or may not regard them with respect and sensitivity.32 The intercultural approach that the National Policy articulates is based on communication between cultures, not only non-indigenous vs. indigenous, but also health professional vs. patient, and the hegemonic biomedical model vs. the folk-traditional model of delivery.33 Language might be one barrier. In addition, it is possible that health facilities may not accommodate for other issues that women value as “good quality of care,” such as the possibility of choosing the position for giving birth, the choice not to use enemas, and the presence of family members during delivery. Past research has highlighted the patronizing attitudes of health providers, who blame women for not attending health services and reprimand them in efforts to change their behavior.34 We suggest that rather than encouraging indigenous women to deliver at facilities they experience as unpleasant, efforts to secure reproductive rights should focus on challenging the health systems to engage in an intercultural dialogue to improve the quality of care within a user-centered approach.
Family planning
The reported prevalence of use of family planning methods in Orellana was high, 79.3% among women who were married or in a formal union, and differences between urban, rural, and indigenous women were minimal. Disparities were nonetheless evident in the type of method used. For indigenous women the most prevalent was the rhythm method, and we can expect that many of these women will have difficulties in timing the safe periods (with still unknown effectiveness when used correctly), while modern methods were preferred by rural and especially urban non-indigenous women.35 The percentage of unwanted pregnancies was also much higher among indigenous women. The fact that indigenous women identified nearly half of all pregnancies as unwanted debunks common perceptions that indigenous women “want to have children” and that family planning is “outside their culture.”36 These results call into question the cultural relativism that deems some reproductive and sexual rights as imposed and antagonistic to indigenous cultures. The survey data suggests, rather, that the right of indigenous women to decide upon the number of children they want is being violated.
Others have described the intersection between gender inequity and ethnicity that places indigenous women in the most disempowered position.37 It remains the state’s responsibility to address this issue; such responsibility is not adequately addressed by the mere presence of a national policy that includes family planning as an objective. Nor is a “one size fits all” approach sufficient. The Ministry of Health and related departments must develop interventions to ensure that women have access to quality family planning services that are adapted to the needs of different sectors of the population.38 Stakeholders from the indigenous and non-indigenous populations also have the responsibility to challenge the gender inequities that are evident in socio-cultural norms and interactions.
Pregnancy among adolescent girls
Contraceptive use by adolescent girls in Orellana is slightly lower than that of adult women. The differences are slight between indigenous and non-indigenous adolescent girls. Condom use is very low, which may also have implications for health interventions in HIV/AIDS transmission.39 Further research is needed to explore the differences between urban and rural girls regarding pregnancy intention compared with their adult counterparts. The higher proportion of wanted pregnancies among rural girls might reflect different life expectations among this population or fewer opportunities, perhaps leading to the perception that motherhood is their only feasible option.
The high proportions of adolescents experiencing pregnancy might also reflect barriers to reproductive services. Confidentiality at health services may be subordinated to parental consent. Even if confidentiality is assured, young girls seeking access to reproductive and health services may experience other barriers, such as scheduling issues, health center requirements, or providers’ attitudes.40 Elevated adolescent pregnancy rates may also be a consequence of the poorer social and economic situation of women living in this area. Finally, adolescent pregnancies have been correlated with lower decision-making capacity, which may be due to age or gender inequities.41 In Latin America, for example, the culture of “machismo-marianismo” encourages women to play a submissive role that focuses on sacrificing for others, diminishing their ability for decision-making.42
Monitoring for accountability
Our study’s methodology of data disaggregation by residence-ethnicity and age enabled us to locate inequities easily. The residence-ethnic disaggregation data demonstrated the wide differences between urban and rural women and, within the rural group, between indigenous and non-indigenous women. Age disaggregation yielded information on the prevalence of unwanted pregnancies, with the proportion of unwanted pregnancies rising with women’s age, and also identified differences between rural and urban adolescents.
Such information is a necessary tool for planning and monitoring. Thus, the collection of data and the response to any revealed inequities must not be separated. Our findings suggest that Ecuador’s ENDEMAIN, despite its national breadth, may not be an optimal tool for monitoring how effectively the National Policy on SRHR is being implemented in places such as Orellana that are regionally isolated.43 The survey results emphasize that locally collected data can be a useful tool for monitoring how well the National Policy is being implemented and for highlighting inequities that justify differentiated interventions. Using such findings establishes a foundation for accountability, a cornerstone of human rights and an essential principle in their realization.
The National Commission for Reproductive and Sexual Health and Rights of Ecuador is now initiating the implementation of an “Observatorio de los Derechos Sexuales y Reproductivos” [Observatory for Reproductive and Sexual Rights] to monitor the implementation of the National Policy.44 We suggest that use of HeRWAI, as it was applied in this study in Orellana, could be a valuable tool for the “Observatorio.” The authors are further disseminating the findings presented here through meetings in both Orellana and Quito to local and national authorities. Studies such as this one are most effective when they serve not only academic purposes, but also serve as tools to advocate the need for specific measures that address identified inequities in the exercise of sexual and reproductive rights.
Conclusions
This paper identified and discussed gaps in access to services which must be addressed in order to fulfill the sexual and reproductive rights and health of women living in the province of Orellana in the Amazon basin of Ecuador. Using a modified version of the Health Rights of Woman Assessment Instrument, we evaluated government obligations related to reproductive and sexual health (“what should be happening”), conducted a cross-sectional community-based survey to establish actual access to services (“what is happening”), and discussed the evident discrepancies between the two. An accessibility gap was evident in the wide differences in access to reproductive health between rural and urban women. Ethnic inequities were evident in poorer reproductive health indicators for indigenous women compared to non-indigenous women. These ethnic inequities may reflect accessibility barriers as well as cultural issues that shape women’s reproductive decisions. Ethnic inequities also intersect with gender inequities, age, and residence to increase the vulnerability for specific groups of women. Results of the community-based study also call into question the validity of available data used to monitor policies and programs. Ecuador’s official data, collected using the ENDEMAIN survey, do not accurately represent isolated areas such as Orellana. The use of national-level data for monitoring functionally prevents the disclosure of inequities; this limitation makes it inadequate for justifying and designing the differentiated interventions that would redress such inequities. The community-based study demonstrates that local initiatives for data collection are feasible and may yield data more suitable for monitoring and designing interventions. Cumulatively, these data indicate a significant gap between national policy and action, obligation, and reality. The weakness of Ecuador’s National Policy lies in its lack of targets and its inadequate discussion of resources and responsibilities of the involved parties on whom effective monitoring and intervention depends. Accountability for sexual and reproductive health and rights in isolated, impoverished areas like Orellana depends on meaningful, accurate, and disaggregated information, and the development of mechanisms to ensure that citizens (especially those most vulnerable) can demand that their governments honor stated commitments.
Acknowledgments
Funding for the field work was provided by the “Consejo Provincial de Orellana” within its ongoing Demographic and Health Surveillance System. The authors are grateful to Fundación Salud Amazónica (FUSA) and UNFPA Ecuador for allowing Isabel Goicolea to carry out this research while working in Orellana, and to Ann-Britt Coe for reviewing this article and giving her comments.
References
1. K. Annan, Address to the Fifth Asian and Pacific Population Conference in Bangkok, Thailand, 2002. Available at http://www.unis.unvienna.org/unis/pressrels/2002/sgsm8562.html.
2. L. P. Freedman, “Using Human Rights in Maternal Mortality Programs: From Analysis to Strategy,” International Journal of Gynaecology and Obstetrics 75/1 (2001), pp. 51–60; U. M. Project, Investing in Development: A Practical Plan to Achieve the Millenium Development Goals (London: Millenium Project, 2005); “Towards Evidence to Secure Reproductive Rights” [editorial], The Lancet 363/9402 (2004), p. 1; A. Germain, “Reproductive Health and Human Rights,” The Lancet 363/9402 (2004), pp. 65–66; M. F. Fathalla, S. W. Sinding, A. Rosenfield, and M. M. Fathalla, “Sexual and Reproductive Health For All: A Call For Action,” The Lancet 368/9552 (2006), pp. 2095–2100; S. W. Sinding, “Health and Hope, Rights and Responsibilities: Action Agenda, Global Roundtable: Countdown 2015,” Reproductive Health Matters 12/24 (2004), pp. 154–159.
3. A. Glasier, A. M. Gulmezoglu, G. P. Schmid, et al., “Sexual and Reproductive Health: A Matter of Life and Death,” The Lancet 368/9547 (2006), pp. 1595–1607; D. Shaw, “Women’s Right to Health and the Millennium Development Goals: Promoting Partnerships to Improve Access,” International Journal of Gynaecology and Obstetrics 94/3 (2006), pp. 207–215; A. Langer, “Cairo After 12 Years: Successes, Setbacks, and Challenges,” The Lancet 368/9547 (2006), pp. 1552–1554.
4. Sinding (see note 2); R. P. Petchesky, “Rights and Needs: Rethinking the Connections in Debates Over Reproductive and Sexual Rights,” Health and Human Rights: An International Journal 4/2 (2000), pp. 17–29; A. Germain, R. Dixon-Mueller, “Reproductive Health and the MDGs: Is the Glass Half Full or Half Empty?” Studies in Family Planning 36/2 (2005), pp. 137–140; A. E. Burke, and W. C. Shields, “Millennium Development Goals: Slow Movement Threatens Women’s Health in Developing Countries,” Contraception 72/4 (2005), 247–249; P. Hunt, and J. Bueno de Mesquita, The Rights to Sexual and Reproductive Health (Essex, UK: University of Essex, 2006); J. Asher, The Right to Health: A Resource Manual for NGOs (London: Commonwealth Medical Trust; 2004); B. Dean, E. E. Valdeavellano, M. McKinley, and R. Saul, “The Amazonian Peoples’ Resources Initiative: Promoting Reproductive Rights and Community Development in the Peruvian Amazon,” Health and Human Rights: An International Journal 4/2 (2000), pp. 219–226.
5. “Towards Evidence to Secure Reproductive Rights” (See note 4).
6. Sinding (see note 2); Hunt and Bueno de Mesquita (see note 4); Asher (see note 4); S. Bakker, and P. Hansje, Health Rights of Women Assessment Instrument (Utrecht: Aim for Human Rights, 2006).
7. I. Goicolea, “Exploring Women’s Needs in an Amazon Region of Ecuador,” Reproductive Health Matters 9/17 (2001), pp. 193–202.
8. CEPAR, ENDEMAIN, 2004: Encuesta Nacional de Demografía y Salud Materno Infantil, 2004. [National Demographic and Maternal Health Survey, 2004] (Quito; 2005).
9. Langer (see note 3); Fathalla et al. (see note 2); Hunt and Bueno de Mesquita (see note 4); Asher (see note 4); L. Bambas, “Integrating Equity into Health Information Systems: A Human Rights Approach to Health and Information,” PLoS Medicine 2/4 (2005), p. e102; P. Braveman and S. Gruskin, “Poverty, Equity, Human Rights and Health,” Bulletin of the World Health Organization 81/7 (2003), pp. 539–545.
10. CEPAR (see note 8).
11. Langer (see note 3).
12. Bakker and Hansje (see note 6); HeRWAI was developed by “Aim for Human Rights” (a Dutch human rights organization founded in 1981) with the participation of organizations of four continents and has been tested in Bangladesh, Pakistan, Kenya, and the Netherlands.
13. Ibid.
14. C. P. Orellana, Sistema de Información en Demografía, Salud y Ambiente en la Provincia de Orellana. Línea de Base 2006 [Information System on Demography, Health and Environment in the Province of Orellana. Baseline 2006] (Orellana, Ecuador: Consejo Provincial de Orellana, 2007).
15. Alba Peralta, activist working with Users Committees in Orellana, personal communication, December 2008.
16. Alba Peralta, activist working with Users Committees in Orellana, personal communication, January 2008.
17. The cluster sample selection meant that first a list of communities and urban sectors was developed using data from the local governments, including approximate information on the number of inhabitants (women). Clusters with a similar number of inhabitants were constructed by gathering small communities into a cluster or by splitting big communities into several clusters of the same size. After constructing the clusters, a number were randomly selected until reaching the sample size that was needed. Selected communities were visited and all the houses within the community were included for applying the questionnaires.
18. The questionnaire was based on Nicaragua’s “Encuesta Sobre Salud Infantil y Salud Reproductiva, León.” Ethical issues were addressed in advance; prior to the study, provincial authorities had approved its development; community leaders were consulted and permission requested; and verbal consent was asked of all potential participants at the household visits. For delivery care, the proportion of deliveries attended by skilled professional was calculated following the WHO definition, with the attendant defined as skilled if she/he was a doctor, a midwife, or a nurse (UNFPA, University of Aberdeen, Maternal Mortality Update, 2004: Delivering into Good Hands (New York: UNFPA, 2004). For access to family planning, two indicators were measured: prevalence of contraceptive use and pregnancy intention, ascertaining whether it was wanted, mistimed, or unwanted. For pregnancy among adolescent women, contraceptive use, pregnancy intention, proportion of adolescents experiencing pregnancy, and skilled delivery care among adolescents were calculated. Data were entered and analyzed using EpiInfo Windows 3.4. The variable residence-ethnicity was split into three categories: urban areas, rural non-indigenous communities, and rural indigenous communities. Prevalences were calculated according to place of residence. Retrospective information about pregnancies was used to develop trends on skilled delivery care from the 1970s to the present.
19. Here urban areas refer to very small towns with less than 20,000 inhabitants, and where indigenous populations are still a minority. This is quite different from the particularly vulnerable situation of indigenous women who migrated to very big cities such as Quito or Lima.
20. Constitución Politica del Ecuador 1998 [Ecuador´s Political Constitution 1998] (Quito; 1998). While this article was undergoing revision, a new Constitution was passed in Ecuador, in September, 2008 (Constitución Política del Ecuador 2008 [Ecuador´s Political Constitution 2008] [Quito; 2008]). The new Constitution includes more articles related to reproductive and sexual rights and gender equity; for example, article 32, that the state must warrant access to reproductive and sexual health care and promotion; article 43 referring to the rights of women during pregnancy and breastfeeding; statements that gender equity policies and programs must be implemented by the state at all levels; assertions about the state´s responsibility in fighting gender-based violence; and sexual education as the state’s responsibility. The new Constitution also includes more articles regarding the rights of the indigenous populations, for example recognizing the state as multinational (giving the status of nations to indigenous groups); in addition, the indigenous value of “good living” (sumak kawsay) is included in the Constitution as a model for sustainable development.
21. Ecuador Ministry of Health, Política Nacional de Salud y Derechos Sexuales y Reproductivos [National Policy for Sexual and Reproductive Rights and Health] (Quito; 2005).
22. Ley de Maternidad Gratuita y Atención a la Infancia [Free Maternity Law] (Quito; 1998).
23. Funds for the law go directly from the Ministry of Finances to a special unit called Unidad de Gestión de la LMGYAI [Management Unit of the Free Maternity Law]. This unit delivers funds directly to each health departments geographically distributed throughout the country. The amount of money sent to each health department depends on the number and kind of health services they provide, based on a reimbursement list that establishes how much money should be sent per each normal delivery attended, family planning consultation, management of spontaneous abortions, etc.
24. Alba Peralta, activist working with users committees in Orellana, personal communication, January 2008.
25. During the last months of 2008, the coverage of the Free Maternity Law was increased to include other populations (men, health services not related to reproductive and maternal health), and the budget for health was increased. However, gratuity is still not fully achieved in Orellana’s public health services because on many occasions patients must buy drugs or supplies outside the hospital (Alba Peralta, activist working with users committees in Orellana, personal communication, December 2008).
26. Maritza Segura, member of the National Commission for Reproductive and Sexual Health and Rights, personal communication, December 2008; National Health Council, Plan de Acción de la Política de Salud y Derechos Sexuales y Reproductivos 2006-2008 [Action Plan for the Policy for Sexual and Reproductive Rights and Health 2006–2008] (Quito; 2007).
27. The Plan does not state what populations are considered “most vulnerable;” however national statistics reveals the gaps on access to family planning between urban and rural women, non-indigenous and indigenous, with higher levels of education and illiterate and within the lowest socioeconomic quintiles and the highest.
28. Basic emergency obstetric care (EmOC) signal functions include administration of parenteral antibiotics, parenteral oxytocin and parenteral anticonvulsants, manual removal of placenta, removal of retained products, and assisted vaginal delivery. Comprehensive EmOC includes all of the above in addition to surgery (e.g., caesarean section) and blood transfusion. UNFPA, Maternal Mortality Update, 2002: A Focus on Emergency Obstetric Care (New York: UNFPA, 2003).
29. UNFPA, Código de la Niñez y Adolescencia [Adolescents National Code] (Quito; 2003).
30. UNFPA (2004, see note 18); UNFPA (2003, see note 29); A. Paxton, D. Maine, L. Freedman, et al., “The Evidence for Emergency Obstetric Care,” International Journal of Gynecology and Obstetrics 88 (2005), pp. 181–193.
31. Goicolea (see note 7); UNFPA, (2004, see note 18); UNFPA, 2003 (see note 29); E. Bocaletti, C. Laspina, and G. Orozco, Camino de la Sobrevivencia Materna en Ecuador [Path of Maternal Survival in Ecuador] (Quito: Ministry of Health, UNFPA, OPS/OMS, UNICEF, 2001).
32. We use the term “interculturality” not as a synonym of multiculturalism but to emphasize the “interaction” and mutual influence between cultures, as described by Alsina, who wrote that “Interculturality . . . supposes the existence of a relation between the people who belong to the various cultural groups, it is a concept fuller than the simple fact “multicultural” . . . interculturality implies, by definition, interaction” M. R. Alsina, La Comunicación Intercultural (Barcelona: Anthropos, 1999), p.72.
33. Dean et al. (see note 4); UNFPA (2004, see note 18); A. V. Camacho, M. D. Castro, and R. Kaufman, “Cultural Aspects Related to the Health of Andean Women in Latin America: A Key Issue for Progress Toward the Attainment of the Millennium Development Goals,” International Journal of Gynaecology and Obstetrics 94/3 (2006), pp. 357–363; D. González Guzman, Manual para la Humanización y Adecuación Cultural de la Atención del Parto (Quito: Dirección Provincial de Salud de Tungurahua, Family Care International, Proyecto de Garantía de Calidad; 2007); PAHO, Gender, Equity and Indigenous Women’s Health in the Americas (Washington: Pan-American Health Organization, 2004); M. Hautecoeur, M. V. Zunzunegui, and B. Vissandjee, “Las Barreras de Acceso a los Servicios de Salud en la Población Indígena de Rabinal en Guatemala” [Barriers to Accessing Health Care Services for the Indigenous Population in Rabinal, Guatemala], Salud Pública de México 49/2 (2007), pp. 86–93; J. J. Miranda, and A. E. Yamin, “¿Políticas de Salud y Salud Politizada? Un Análisis de las Políticas de Salud Sexual y Reproductiva en Perú desde la Perspectiva de la Ética Médica, Calidad de Atención y Derechos Humanos” [Health Policies and Politicized Health? An Analysis of Sexual and Reproductive Health Policies in Peru from the Perspective of Medical Ethics, Quality of Care, and Human Rights], Cadernos de Saude Publica 24/1 (2008), pp. 7–15.
34. Goicolea (see note 7).
35. D. Grimes, M. Gallo, V. Grigorieva, et al., “Fertility Awareness-based Methods for Contraception: Systematic Review of Randomized Controlled Trials,” Contraception (2005) 72/2 pp. 85–90.
36. Dean et al. (see note 4); Goicolea (see note 7); UNFPA, Cuerpos, Tambores y Huellas: Sistematización de Proyectos de Salud Sexual y Reproductiva 2000–2003 en Ecuador (Quito: UNFPA, 2004).
37. Camacho et al. (see note 33); PAHO (see note 33); M. de la Cadena, “Las Mujeres son más Indias: Etnicidad y Género en una Comunidad del Cuzco,” Revista Isis Internacional 16 (1992), pp. 25–43; M. Heise, L. Landeo, and A. Bant, Relaciones de Género en la Amazonía Peruana (Lima: Centro Amazónico de Antropología y Aplicación Práctica, 1999).
38. L. Bambas, “Integrating Equity into Health Information Systems: A Human Rights Approach to Health and Information,” PLoS Medicine 2/4 (2005), p. e102; P. Braveman, and S. Gruskin, “Poverty, Equity, Human Rights and Health,” Bulletin of the World Health Organization 81/7 (2003), pp. 539–545; Bruce, “Fundamental Elements of the Quality of Care: A Simple Framework,” Studies in Family Planning 21/2 (1990), pp. 61–91.
39. L. H. Bearinger, R. E. Sieving, J. Ferguson, and V. Sharma, “Global Perspectives on the Sexual and Reproductive Health of Adolescents: Patterns, Prevention, and Potential,” The Lancet 369 (2007), pp. 1220–1231. UNFPA, UNFPA Framework for Action on Adolescents and Youth: Opening Doors with Young People (New York: UNFPA, 2007).
40. Glasier et al. (see note 3); Sinding (see note 2); UNFPA (2007, see note 39); International Women’s Health Coalition, Young Adolescent’s Sexual and Reproductive Health and Rights: Latin America and the Caribbean (New York: International Women’s Health Coalition; 2007); R. Cook, and B. M. Dickens, “Recognizing Adolescents’ ‘Evolving Capacities’ to Exercise Choice in Reproductive Healthcare,” International Journal of Gynaecology and Obstetrics 70/1 (2000), pp. 13–21.
41. Hunt and Bueno de Mesquita (see note 4); Bearinger et al. (see note 39); UNFPA (2007, see note 39); International Women’s Health Coalition (see note 40); WHO, Women’s Health and Human Rights: Monitoring the Implementation of CEDAW (Geneva: WHO, 2007).
42. Goicolea (see note 7); G. A. Galanti, “The Hispanic Family and Male-Female Relationships: An Overview,” Journal of Transcultural Nursing 14/3 (2003), pp. 180–185.
43. CEPAR (see note 8).
44. Maritza Segura, member of the National Commission for Reproductive and Sexual Health and Rights, personal communication, December, 2008.