Frank V. McMillan, Nicola Browne, Stephanie Green, and Dessie Donnelly
Health and Human Rights 11/1
Published June 2009
Abstract
Due to a recent and dramatic rise in suicide and self-harm rates, mental health services have received a high level of attention in the politics of Northern Ireland, resulting in the implementation of numerous policies and the publication of many public reviews on the subject. Critically, these policies have also emphasized and required the participation of mental health service users in decision making about service design, implementation, and monitoring. This paper analyzes the experience of a group of mental health service users in north and west Belfast, the Public Initiative for the Prevention of Suicide–Greater Shankill Bereaved Families Rights Group supported by the Participation and the Practice of Rights Project, as they campaigned for policy change using a human rights-based approach. It considers, first, the group’s use of a participatory, “bottom-up” approach to set human rights indicators and benchmarks defined by group members themselves as an example of meaningful participation from an affected group. The paper then looks specifically at one of the group’s issues — follow-up care — and reveals how the group was able to bring about policy change on this issue across Northern Ireland. Finally, it discusses how the group’s experience in this campaign has revealed problems with the way that the government currently engages with mental health service users in Northern Ireland. The article closes by identifying key next steps to be taken as the focus of the campaign shifts to ensuring that active, free, and meaningful participation takes place in accordance with international human rights standards.
In the years following the end of conflict in Northern Ireland, north and west Belfast experienced skyrocketing rates of suicide and self-harm. In a longitudinal study across 426 constituencies in the United Kingdom, Brock et al. found significant differences in the suicide rates between 1991–1997 and 1998–2004 in Northern Ireland. The Belfast North parliamentary constituency’s suicide rate rose from 319th to 11th highest in the UK; the increase in suicide in Belfast West led to a similar increase, from 259th to 13th highest.1
As a result of this increased suicide rate — and because of some highly publicized and tragic failures of mental health services — mental health has recently received special emphasis in Northern Irish politics.2 A number of government policies and reports published in recent years have highlighted the commitment to reduce the number of suicides and to improving mental health services of Northern Ireland’s Department of Health, Social Services, and Public Safety (DHSSPSNI).3
Critically, these policies also emphasize the importance of active participation in making decisions related to mental health by mental health service users, carers, and bereaved families. For example, Protect Life, the DHSSPSNI suicide prevention strategy for 2006–2011, came into existence largely as a result of sustained campaigning by families bereaved by suicide; as such, it lists engagement with mental health service users and bereaved families as one of its core principles. Another DHSSPSNI document, the Bamford Review, emphasizes “the importance of service users and carers as partners in service planning, development, delivery and monitoring” of mental health services and policy.4 A number of consultative bodies, including a Families Forum and the Suicide Strategy Implementation Body (SSIB), were set up to foster user participation and to give mental health service users a “powerful voice.”5 These policies and structures represented a specific attempt to go beyond affirming the importance of participation by mental health service users in making decisions related to their treatment to actually ensuring their ability to participate and furthermore encouraging their participation in the overall design, implementation, and monitoring of services.
But has this participation actually been meaningful? Has it enabled mental health service users to influence policy planning, development, delivery, and monitoring as required under international human rights and local policy standards?6
In this paper, we highlight the work of a group of mental health service users, bereaved families, and carers in north and west Belfast. Since 2007, the Public Initiative for the Prevention of Suicide–Greater Shankill Bereaved Families (PIPS-GSBF) Rights Group has been working with the Participation and the Practice of Rights Project (PPR) to improve mental health services in Northern Ireland and to increase service users’ participation in decision making related to their health care.7 This article focuses on one of the group’s recommendations, a “card before you leave” appointment system for mental health patients, which the DHSSPSNI has since adopted. This intervention was initiated to ensure that individuals discharged after receiving mental health treatment (either in-patient or accident and emergency services) receive a card with the date and time of their follow-up appointment before they leave the premises. Even if the appointment were not to take place within one week as required, having a card noting a fixed date and time for their next appointment would ensure that the patient knew that she or he was still connected to services.
This article uses the “card before you leave” example to highlight three points in relation to participation and health policy in Northern Ireland. The points, which we hope will be useful to others, are as follows:
First, the “card before you leave” system illustrates that taking a participatory, “bottom-up” approach to human rights indicators and benchmarks can engender meaningful participation by service users, allowing them to tangibly track the progressive realization of their rights and make reasonable, targeted recommendations in accordance with human rights standards. An important aspect of this approach is that the human rights indicators are defined by service users rather than by governments.
Second, the “card before you leave” system concretely demonstrates the potential of genuine participation to identify and address problems in the delivery of mental health services. Service users themselves can suggest, define, and monitor tangible changes to mental health services, changes that have the potential to save lives.
Third, the group’s work on the issue of follow-up care both points to the existence of structural obstacles to meaningful participation from service users and highlights the need for research and change if rights-based participation is ever to be mainstreamed into health policy. The final section of the paper considers the experiences of these service users seeking to influence mental health policy in Northern Ireland and outlines the next steps they plan to take. It is our hope that these steps will be applicable to other activists and policymakers who are attempting to increase meaningful participation of other vulnerable groups.
A bottom-up approach to human rights indicators and benchmarks
Human rights indicators and benchmarks, set and monitored by service users themselves, are central to the approach used by the PIPS-GSBF Rights Group and by PPR. This section introduces the indicators and benchmarks used in the group’s approach, as well as the development program that supported them in this process. We then describe some of the specific recommendations made by this group through their work.
Paul Hunt, former UN Special Rapporteur on the Right to Health, has emphasized — both in this journal and elsewhere — the importance of human rights indicators and benchmarks for the effective implementation of economic and social rights.8 By highlighting specific issues that need to be addressed in accordance with human rights standards, and by adopting concrete indicators and benchmarks to measure progress, states can be held accountable for the progressive realization of economic and social rights as required under the International Covenant on Economic, Social and Cultural Rights. This process ensures that progressive realization does not become an abstract “exit” clause for states; rather, the indicators and benchmarks can be used to set definite targets for the fulfillment of states’ duties under international human rights law.
While Hunt makes recommendations for how these indicators and benchmarks can be set by states or by international bodies, PPR and the PIPS-GSBF Rights Group have taken a participatory, bottom-up approach to Hunt’s work.9 In this approach affected groups set and monitor human rights indicators and benchmarks for specific issues related to their own economic and social rights.10
Allowing affected groups to pinpoint such issues is essential for translating international human rights standards into action. As Profesor Tara Melish points out:
At the international level there are enshrined values — principles. Those values and principals in the abstract need to be given substantive content and they can only be given substantive content on the ground by people who are interacting with the rights and who understand what they mean to their daily lives. And, they can ensure that the policies and programmes which are put into effect at the local level are responsive to local problems. That is what the human rights struggle is about — how to make those values that we all understand as universally applicable to everybody meaningful in our lives at the local level. That’s why [the PIPS-GSBF Rights Group] is so important.11
Integral to this approach has been the development program undertaken by the PIPS-GSBF Rights Group in collaboration with PPR. Since October 2006, PPR has been working with a number of individuals from the Public Initiative for the Prevention of Suicide and Greater Shankill Bereaved Families (formerly “Reaching Across to reduce Your risk of Suicide” [RAYS]) as well as individuals from other suicide/self-harm support groups in north and west Belfast as part of this program. The development program has focused on a broad range of subjects and issues, including confidence building, understanding basic international human rights standards, action research, media training, identification of problems with local mental health service delivery, and preparation for engagement with government.
One member of the group, MG, recounted some of the ways that the development program had initially shifted his thinking about rights in his daily life:
I went to the hospital with a friend who had been asked to attend his daughter’s case conference with his daughter’s consent. At the last minute — when we were about to go into the room — he was told he couldn’t go. He was quoted a lot of stuff about human rights — nothing about his rights as a carer — rights were being used against him. My friend felt very hurt and angry — not just about not being let into the case conference — but about how he was being treated. I took him aside immediately as I felt some of his rights were being violated . . . and helped him make a written complaint. My friend would have otherwise been left there to feel angry and powerless — at least making the complaint was doing something.12
The initial development program with the group focused primarily on developing a participatory process for setting user-defined human rights indicators and benchmarks. The group identified a broad set of problems with mental health services in their community that they thought were in need of improvement. They linked many of these issues to international human rights and local policy standards.13 Through development sessions on action research, the group developed a survey and created focus groups in order to establish an evidential baseline and to assess the extent to which these issues affected other mental health service users in their surrounding communities.
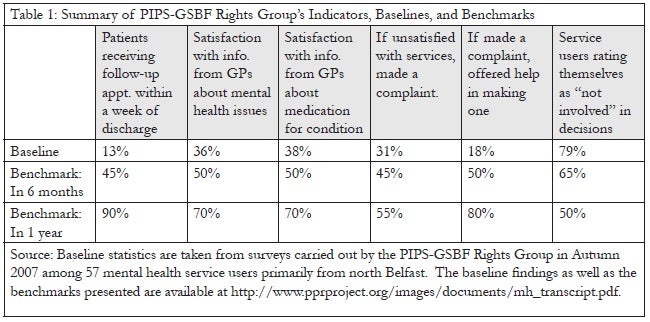
From this foundation, the group chose six human rights indicators around which to set benchmarks or specific timelines for change. Using these indicators and benchmarks, they hoped to make tangible the requirement of the government to progressively realize economic and social rights. By adapting Hunt’s work on human rights indicators and benchmarks, this particularly vulnerable group of service users in Northern Ireland was able to employ a participatory approach to concretize the state’s obligation to ensure that services improve over time.14 The six human rights indicators chosen centered around four issues related to mental health services in Northern Ireland: follow-up appointments, complaints, information from General Practitioners (GPs), and service user participation.
- Follow-up appointments: The group was concerned with the health service’s failure to provide timely follow-up care for mental health patients, especially for those at risk of suicide and self-harm. Through focus groups and surveys, it became clear that patients and carers viewed follow-up appointments as a “lifeline” to mental health services.15
- Complaints: The group was concerned with the inaccessibility of the health system’s complaints procedure and with the lack of help available to navigate this system once a complaint had been made. They were also aware that the complaints system for the health service was undergoing revision.16
- Information from GPs: Training of GPs in depression awareness had not materialized despite calls from service users and the commitment reflected in the Promoting Mental Health 2003–2008 strategy.17 The training was finally delivered under the Protect Life Strategy, but there were reports of low uptake among GPs and of dissatisfaction with the course content. Because GPs are often the first port of call for those suffering from mental health problems, the group believed that it was paramount to ensure that patients receive appropriate support from GPs.18
- Service user participation: The group noted the central importance accorded to service user participation in the flurry of mental health policies and reviews initiated by the government in recent years. A number of group members had themselves been involved in government-designed participation structures intended to give a voice to service users and their carers. However, they wanted to measure the extent to which these structures actually promoted meaningful participation of mental health service users.19
The baseline for the indicators and their benchmarks for change are presented in Table 1.
The group presented these human rights indicators and benchmarks as well as the results of their surveys to an international panel of human rights and mental health experts in November 2007.20 The panel validated the human rights benchmarks advocated by the group as a reasonable and necessary timeline for change in accordance with human rights standards.
Professor Melish, a member of the panel, commented on the work of the group:
This model of holding government accountable to human rights mechanisms hasn’t been used in other parts of the world. That is, in most places we talk about governments identifying their own indicators…[I]n the US we have a government who defines indicators. With respect to poverty for example, we have indicators that are showing wonderful progress while poverty is increasing because they are not measuring the right things. That’s why it is so important that communities are the ones who themselves define what the indicators are.21
Importantly, as Melish makes clear, user-defined human rights indicators and benchmarks — as well as other forms of bottom-up, participatory, democratic accountability — are not uniquely applicable to mental health, or even to the right to health more generally. In fact, each of the groups with which PPR works has applied a similar methodology to different economic and social rights issues. In the case of the right to adequate housing, for example, residents identified indicators such as pigeon waste on each floor’s communal landings, as well as drainage and sewage problems. They then set specific, measurable benchmarks for the government to meet over time.
Human rights indicators and benchmarks identified through bottom-up, participatory processes offer an opportunity to maximize the benefits of vulnerable groups’ expertise. This expertise is derived from rights holders’ personal experiences with how government policies and systems may fail to meet their needs on a daily basis. These tools, we believe, can be used by others, for example, by activists adopting a similar approach with other affected groups, and by policymakers putting structures in place to ensure service users’ benchmarks are met and that real change is achieved on the ground.
The next two sections highlight the usefulness of this approach as well as how existing structures have not been effective at allowing this to occur thus far.
Breaking the mold: Achieving change in follow-up care
Early in their development program, the group highlighted timely follow-up appointments for mental health service users as an important issue on which to work. Many group members or their families had direct experience with this issue — waiting months for a follow-up appointment that sometimes never occurred. In one case, a group member’s son attempted suicide while his mother and a voluntary support worker actively sought information from the hospital on when his follow-up appointment would be. The group felt that the distress experienced by patients and families, resulting from not knowing when or whether further treatment would be received, could be prevented by implementing an efficient and responsive appointment system. This section highlights the group’s campaign and recommendations concerning follow-up care for mental health service users, specifically their campaign to implement a “card before you leave” appointment system for mental health patients across Northern Ireland. We have chosen to focus on a particular case study because we believe it better illustrates both the successes the group has achieved and the challenges it has faced. The case study also reveals some of the reasons behind the group’s decision to act outside of the existing government consultative structures to use more explicitly participatory methods to bring about policy change. For the purposes of this article, we define “existing consultative structures” as those structures, bodies, and forums designed and led by the government, which include mental health service users as members and which have the express purpose of increasing “user involvement” in policy processes.
After identifying the importance of improving follow-up care, the group, supported by PPR, conducted research to learn more of the larger context. In government reports, they discovered that post-discharge suicides reached their peak in the first 1–2 weeks following discharge and that 66% of post-discharge suicides in Northern Ireland occurred before the first follow-up appointment.22 In policy documents, they discovered that UK-wide guidelines on follow-up care for mental health service users set specific standards for the timeliness of follow-up appointments, stating that:
All discharged in-patients who have severe mental illness or recent (less than three months) history of deliberate self-harm should be followed up within one week.23
This specific guideline had itself been incorporated into the discharge protocol for the local hospital in north Belfast. It had also been incorporated into the discharge protocol of the local health trusts through which most patients surveyed had received their care. One such discharge protocols states, for example:
While the timing of follow-up is an issue to be decided by local clinicians, they should be aware of national guidance: within one week of all discharges.24
Finally, these local and national standards are supported by international human rights standards concerning access to health services. For example, General Comment 14 of the Committee on Economic, Social and Cultural Rights, commenting on Article 12.2 (d), calls for
[t]he creation of conditions which would assure to all medical service and medical attention in the event of sickness
. . . both physical and mental, includes the provision of equal and timely access to . . . appropriate mental health treatment and care.25
And Paul Hunt’s 2008 Report of the Special Rapporteur on the Right to Health explicitly highlights the need for effective referral systems:
The [health] system also needs an effective process when a health worker assesses that a client may benefit from additional services and the client is referred from one facility to another. The absence of an effective referral system is inconsistent with the right to the highest attainable standard of health.26
The conceptual foundation provided by the group’s research on government reports and policy documents, combined with its action research documenting that only 13% of mental health patients actually received a follow-up appointment within one week, made clear to the group the importance of setting one of their human rights indicators around follow-up care. In accordance with international and local policy standards, the PIPS-GSBF Rights Group then tracked the percentage of mental health patients receiving a follow-up appointment within one week of discharge.
On the basis of repeated discussions during their development program and in focus groups, the group recommended that a “card before you leave” appointment system be introduced as a first step toward the goal of ensuring that all patients with severe mental illness and a recent history of self harm receive a follow-up appointment within one week. Such a system would provide patients discharged after receiving mental health treatment with the date and time of their follow-up appointment before they left the premises. This focus on providing each individual with a “card before you leave” would ensure that the patient knew she or he was still connected to services.
After hearing this and other recommendations from the group in November 2007, the international panel of human rights and mental health experts endorsed the human rights indicators and benchmarks set by the group and made the following recommendation to the government in February 2008:
The panel strongly urges the Minister to work with the group to ensure that mental health patients discharged from hospital receive an appointment before they leave in order to fulfil their right to access health care. This is a low-cost and simple requirement but one which would be of considerable benefit to vulnerable individuals.27
On this foundation, provided by the human rights and mental health experts, the PIPS-GSBF Rights Group launched the campaign for a “card before you leave” appointment system to be implemented across Northern Ireland. Such a change, they believed, offered both an effective and efficient use of public resources and constituted a policy change that could immediately save lives.
Notably, this was not the first time that mental health service users had suggested implementing a “card before you leave” appointment system to the DHSSPSNI. In fact, prior to PPR’s involvement, the issue had been repeatedly raised through various existing participatory structures; these included an independent review panel whose agenda included follow-up appointments for mental health patients.28 Despite these recommendations, no movement had taken place on the issue as a result of those processes. Progress was made, however, after a concerted campaign was undertaken during the months following the group’s presentation to the international panel of experts in November 2007. Following the campaign, the Minister of Health, Michael McGimpsey, announced both the Northern Ireland-wide adoption of a “card before you leave” appointment system and the decision to make follow-up care for mental health patients within one week a “Priority for Action” for 2009–2010 (one of 12–15 annual priorities for his department that are monitored by the Minister and his office).29
To achieve these policy changes, the group made strategic choices about how best to pursue their campaign. While the next section highlights some remaining challenges facing the group, the remainder of this section details three decisions made by the PIPS-GSBF Rights Group to ensure that their voices remained the driving force behind the policy changes achieved. They wanted to avoid the challenges and obstacles that service users had met in the past when seeking change through government-run consultations.
First, in line with the recommendations of the international panel, the group made a decision to hold the Minister of Health directly responsible for the human rights indicators and benchmarks they had set. They recognized that while both the Minister and the Belfast Health and Social Care Trust had a responsibility under human rights law to ensure the progressive realization of a person’s right to the highest attainable standard of health, the ultimate (and political) responsibility lay with the Health Minister as the individual directly accountable for all agencies delivering health services in Northern Ireland.30
The group sought to include a formal meeting with the Minister of Health as part of the campaign in order to secure the Minister’s commitment to advancing issues related to their newly defined human rights indicators. In committing to this advancement, the Minister’s department would be in a position to prioritize issues, allocate resources, and amend existing practices to meet the benchmarks set by the group.
The involvement of the Health Minister proved decisive in relation to the group’s recommendation of a “card before you leave” appointment system for mental health patients. While both the Belfast Trust and the Health Minister expressed excitement about the group’s idea, the Belfast Trust focused on obstacles to the proposed system, stating that the multiple information systems and software in use made it simply impossible. On the other hand, as the primary duty-bearer, the Minister of Health was able to exercise his political authority to ensure that such obstacles were overcome. Minister McGimpsey stated in a letter to the group, dated August 8, 2008, that the “card before you leave” appointment system was to be made a reality across Northern Ireland, including the area administered by the Belfast Trust.31
Second, the group made a decision not to engage during their campaign with existing, government-designed consultative structures for mental health service users. These existing structures included government-designed patient advocacy groups and consultative forums on policy, to which they were directed by the Belfast Health and Social Care Trust.32 The group believed that such structures had yet to deliver change on the ground, and focus groups with other mental health service users as recently as January 2009 have supported this conclusion. The group emphasized that these issues had been previously discussed in such forums and raised by advocacy groups with no change perceived as resulting from the discussions.
Instead, the group sought the appointment of a ministerial liaison to follow-up on the group’s campaign. Minister McGimpsey appointed a senior civil servant to fulfill this role. The ministerial liaison was tasked with following up with service delivery bodies, such as the Belfast Trust and the Health Promotion Agency, to ensure that certain tasks were accomplished and that problems were addressed. The civil servant’s appointment played a significant role in the adoption of the “card before you leave” appointment system.
Third and finally, the group did not rely solely on ministerial pressure or their liaison to ensure that their goal to implement a “card before you leave” appointment system was achieved. Throughout the process, the group used external pressure to encourage change. They launched media campaigns highlighting government failures in follow-up care for mental health patients, and they developed broad-based alliances in support of their recommendations. These alliances included community-based service delivery organizations, international advocacy organizations like Mental Disability Rights International, trade unions for health workers, and human rights groups. The PIPS-GSBF Rights Group also made a formal submission to, and directly lobbied, the Northern Ireland Assembly Health Committee about a “card before you leave” appointment system, resulting in its adoption as one of the committee’s 25 recommendations to the Department of Health from their Inquiry into the Prevention of Suicide and Self Harm. This recommendation provided further leverage when meeting with the Health Minister to discuss the group’s human rights indicators and benchmarks.
Finding and changing the patterns of nonparticipation
While the group’s work and public pressure has brought about mental health policy change for Northern Ireland — in both the adoption of a “card before you leave” appointment system and in the Minister’s decision to make follow-up care a Priority for Action for 2009–2010 — it did not result from using existing government-designed consultative structures. The group made a strategic decision not to engage with existing structures because they did not see these structures as having been able to deliver change on follow-up care in the past. This section provides further context to the group’s decision not to seek redress or change through these existing structures. It explores some of the concrete obstacles to meaningful public participation that service users have experienced and outlines next steps for the group. Our hope is that these steps will be transferable to other activists and policymakers who are trying to improve the way that participation takes place in public services that hold obligations under international human rights covenants.
In July 2007, a bereaved family member gave evidence to the Northern Ireland Assembly’s Health Committee during their Inquiry into the Prevention of Suicide and Self Harm. She commented on decisions being made outside the participation structure set up to inform the Protect Life suicide strategy — the Families Forum:
There was a very well publicized mental health programme rolled out in February. We are not against it, nor would we say anything about it. However, approximately £380,000 was spent on that campaign yet not one member of our forum was involved in the programme. The [Families Forum] was set up in September 2006, and it was well known that we were representing people across the Province as best we could. Therefore it was embarrassing not to have had more involvement in the campaign.33
The statement of this individual resembles feelings expressed by members of the PIPS-GSBF Rights Group: that service user participation in existing structures has not always been meaningful, nor has it always involved service users at every stage of the decision-making process on mental health policies and programs.
These experiences and feelings were expressed most clearly during the group’s development program, in which they identified obstacles to their own meaningful participation in public decision making. The list below identifies some of the specific barriers experienced during their interactions with existing government consultation mechanisms. It represents part of a module that the group completed on what meaningful participation, in accordance with human rights standards, should be like. While this list is neither exhaustive nor final, it does point toward the need for further research and analysis, including determining whether the group’s experiences are representative of other participants’ experiences in these structures. Barriers identified included the following:
- “Meetings were draining,” participants mainly spent time “repeating our stories and other people’s stories over and over.”
- Government representatives “spoke in double Dutch,” participants felt “talked down to” because of the language that was used.
- There was “too much waffle and not enough focus on the purpose of the meeting” from the government.
- Money and staff issues were used as excuses, but proof or explanation of this was not usually provided.
- Important decisions were made “without us.”
- Government “always had the chair” and “controlled the agenda.”
- Some service users had confidence during meetings, but it was often a “matter of luck” that they did (for example, past experience with the consultative process).
- Participants were “afraid of feeling stupid.”
Finally, the group also expressed concerns about the meetings they held with the DHSSPSNI and the Belfast Health and Social Care Trust since they began working with PPR. They often felt they were being “pushed from pillar to post” by the DHSSPSNI — going from meeting to meeting — without seeing concrete action from the government as a result of those meetings.
Next steps and conclusion
The work of the PIPS-GSBF Rights Group illustrates the potential of affected groups to effect beneficial change using a participatory, bottom-up approach to set human rights indicators and benchmarks. Human rights indicators and benchmarks developed by affected groups can improve mental health services through tangible and targeted recommendations that are in accordance with international and local standards. They also provide a participatory framework for affected groups to continually monitor and measure the success or failure of service delivery.
The group’s experience also reveals that a human rights-based approach demands focus both on the outcomes achieved — like the implementation of a “card before you leave” appointment system — and on the processes used to achieve them. Without addressing patterns of nonparticipation and the lopsided power relationships between rights holders and governments, many of the underlying causes of problems in service delivery will remain unresolved.
As a result of these experiences, the group has worked with PPR to determine three next steps to help determine the next stage of their campaign. They hope to ensure that future groups of service users can avoid frustration and benefit from an effective, human rights-compliant participation structure rather than having to work outside of existing structures to achieve change. We believe these steps can be useful to both activists and policymakers who aim to improve the participation of affected groups in public decision making as required by international human rights and local policy standards.
First, the PIPS-GSBF Rights Group will research existing consultative and participatory structures set up by the government and focus groups and case studies with mental health service users around participation. This additional context can help determine whether the group’s own experiences are representative of others’ experiences as well. It will also ensure that a broader range of views is included in the group’s analysis.
Second, based on their research, the group will work to expand their current human rights indicators regarding participation into a series of process-based indicators that will identify and add substantive content to the right to participate. In this way, the group will be able to concretize the components of and requirements for a participatory structure that facilitates the progressive realization of the highest attainable standard of health. This, they hope, will be based both on international human rights and local policy standards, as well as on the best practices they have researched and gathered.
Finally, using the indicators described above, the PIPS-GSBF Rights Group plans to monitor (and make continuing recommendations on) the “card before you leave” process by means of a newly formed “card before you leave” implementation group. They also aim to work toward assisting other mental health service users in applying a similar approach to monitor the effectiveness of the participation structures within which they work. The implementation group is a government structure designed to “oversee and support the implementation of a Card before you leave scheme.”34 Through this practical example, the group hopes to show how such process-based human rights indicators can be put into practice and how government practice might be improved by using these indicators as guides.
Throughout this and other work, it is critical that service users themselves find their own participation in public decision making to be meaningful. It must speak to their everyday experience and meet their needs. As Anne Cullen, a parent of a disabled child in Northern Ireland, summarized perfectly:
What I am saying is very simple: do not let user involvement become the next in-thing, like partnership working, empowerment, capacity building or, God forbid, the subject of a university degree. If that happens we will have lost what it is all about.
It is about my son, my daughter, and our lives. It is about how we treat others and how they treat us. It is about mutual respect, it is about hard work. There is room for everyone, particularly those whose life experiences have educated them far more than books ever could.
. . . I now know that my son, my daughter, my family and myself have the right to a decent quality of life. We have a right to be heard, a right to be respected. It is our present and our future. And if user involvement means that we all should be directly involved in sorting this out, then I am all for it.35
The work of the PIPS-GSBF Rights Group offers important insights into how rights-based accountability through the participation of affected groups can positively impact mental health services. And yet, the changes achieved thus far have not yet succeeded in establishing the institutional improvements necessary to meet the human rights obligations for services. Nor has the group’s work significantly improved the decision-making processes used for them. This is particularly true for the most vulnerable in the community. It does, however, offer lessons for how a participatory approach to economic and social rights can deepen our understanding of what rights mean to local communities and of how they can best be implemented to meet the needs of vulnerable groups. As we search for examples of how to integrate economic and social rights standards into national and regional policy, core lessons for the future are emerging from this local group of families and carers.
Frank V. McMillan, MA, is Local Development Worker and Researcher at the Participation and the Practice of Rights Project.
Nicola Browne, LLB, LLM, is Research and Policy Officer at the Participation and the Practice of Rights Project.
Stephanie Green, LLB, is Local Development Worker at the Participation and the Practice of Rights Project.
Dessie Donnelly, MA, is Local Development Worker at the Participation and the Practice of Rights Project.
Please address correspondence to the authors, c/o Participation and the Practice of Rights Project, 54 York Street, Belfast, BT15 1AS, United Kingdom, email: frank@pprproject.org.
References
1. A. Brock, A. Baker, C. Griffiths, G. Jackson, G. Fegan, and D. Marshall, “Suicide trends and geographical variations in the UK, 1991–2004,” Health Statistics Quarterly 31 (2006), p. 15. Available at http://www.statistics.gov.uk/articles/hsq/HSQ31suicide_trends.pdf.
2. For one highly publicized BBC story, see http://news.bbc.co.uk/2/hi/uk_news/northern_ireland
/6765873.stm. On the government’s response to the growing concerns, for example, the Northern Ireland Executive’s Programme for Government 2008–2011 included specific targets to reduce suicide across the states by 15% by 2011; See Northern Ireland Executive, Programme for Government 2008–2011 (Belfast: Northern Ireland Executive, 2008), p. 13. Available at http://www.pfgbudgetni.gov.uk/finalpfg.pdf.
3. See, for example, Promoting Mental Health: Strategy & Action Plan 2003–2008 (Belfast: Department of Health, Social Services and Public Safety, 2003). Available at http://www.dhsspsni.gov.uk/menhealth.pdf; Northern Ireland Department of Health, Social Services and Public Safety, “A Strategic Framework for Adult Mental Health Services,” Bamford Review of Mental Health and Learning Disability (Belfast: Department of Health, Social Services and Public Safety, 2005); Investing for Health Strategy (Belfast: Office of the Minister and Deputy First Minister of Northern Ireland, Department of Health, Social Services, and Public Safety, 2002). Available at http://www.ofmdfmni.gov.uk/investing-for-health-strategy-2.pdf; Northern Ireland Department of Health, Social Services and Public Safety, Protect Life: A Shared Vision 2006–2011 (Belfast: Department of Health, Social Services and Public Safety, 2006).
4. Northern Ireland Department of Health, Social Services and Public Safety, Bamford Review (see note 3), p. 13.
5. Northern Ireland Department of Health, Social Services and Public Safety, Protect Life (see note 3), p. 39.
6. See Committee on Economic, Social and Cultural Rights (CESCR), General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. No. E/C.12/2000/4 (2000), para. 54.
7. The Participation and the Practice of Rights Project (PPR) is a coalition of groups and organizations working on social justice issues on the island of Ireland with emphasis on north Belfast. It aims to give individuals, groups, and communities the tools and support they need to actively assert and campaign for their social and economic rights. Currently PPR works with four groups on economic and social rights issues: the PIPS-GSBF Rights Group on the right to the highest attainable standard of mental health, the Seven Towers Monitoring Group on the right to adequate housing, the Residents’ Jury on the Regeneration of Girdwood Barracks & Crumlin Road Gaol on the right to participate in decisions about regeneration, and the Lower Shankill Residents’ Voice on the right to play. More information and resources available at http://www.pprproject.org or see PPR’s YouTube Station at http://www.youtube.com/PPRProject. As all authors are employed by PPR, this paper is written from an advocate’s perspective and as a case study of that experience.
8. See P. Hunt, UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health. Available at http://www2.ohchr.org/english/issues/health/right/.
9. Paul Hunt spoke at a PPR conference “Making and Measuring Change: A Human Rights Based Approach to Health” in November 2006 in the Carrickdale Hotel, Co. Louth, in his capacity as UN Special Rapporteur on the Right to Health, putting his expertise at the service of community groups from north Belfast and north Dublin as they worked on issues related to local health services. Hunt led a discussion on how human rights indicators can be used to measure the realization of the right to health in local communities. This dialog between local community members and international human rights leaders marked the start of PPR’s work in supporting communities and groups to select and measure human rights indicators to assess whether their human rights are being progressively realized in some of the most disadvantaged communities in Northern Ireland; see Participation and the Practice of Rights Project, Making and Measuring Change: A Human Rights Based Approach to Health (Belfast: Participation and the Practice of Rights Project, 2007). Available at http://www.pprproject.org/images/documents/making%20and%20measuring%20change%20hrba%20to%20health%20nov%2006.pdf.
10. Presently, PPR works across four issues in north and west Belfast — the right to adequate housing in high-rise housing blocks in New Lodge Ward, the right to the highest attainable standard of mental health throughout north and west Belfast, the right to play and leisure in the Lower Shankill, and the right to participate in urban regeneration plans for a 26-acre former jail and army barracks in north Belfast.
11. Participation and the Practice of Rights Project, Rights in Action: Changing Mental Health Service, 28th November 2007, Mental Health Forum Report (Belfast: Participation and the Practice of Rights Project, 2007), p. 6. Available at http://www.pprproject.org/images/documents/mh_transcript.pdf.
12. Unpublished transcribed comments from personal interview, 2008.
13. During this process, the group focused primarily on local and national health policies as well as on policy standards found in the International Covenant on Economic, Social and Cultural Rights. In its work, the group has not used the new Convention on the Rights of Persons with Disabilities or its Optional Protocol. These have not yet been ratified by the UK government. However, it is important to note that it offers potential for others working in different countries. Both Article 26 and Article 29 of the Optional Protocol may be particularly noteworthy. Additionally, the group has thus far not used national human rights legislation, such as the Human Rights Act in the UK. There are, however, specific provisions in the Bill of Rights for Northern Ireland that relate to mental health and other economic and social rights. This has not yet been passed, however, by the Northern Ireland Assembly. Policy analysis was carried out with support from PPR’s policy and research staff.
14. This bottom-up approach to human rights indicators and benchmarks could be used with the right to adequate housing or with other social and economic rights because each of these rights imposes a duty on states to progressively realize them.
15. CESCR, General Comment No. 14 (see note 6), para. 12(b), 17. The term ‘lifeline’ was originally used by the service users in the PIPS-GSBF Rights Group during discussion about the importance of follow-up care.
16. CESCR,General Comment No. 9, The Domestic Application of the Covenant, UN Doc. No. E/C. 12/1998/24 (1998), para. 9. This states that the right to an effective remedy need not be judicial.
17. Promoting Mental Health: Strategy & Action Plan 2003–2008 (see note 3).
18. In CESCR, General Comment No. 14 (see note 6), para. 11, 37, 44(d) underline the importance of providing health related information. In the UK, family doctors are referred to as GPs.
19. CESCR General Comment No. 14 (see note 6). This general comment focuses on participation of affected groups in decisions, including the statement, “Effective provision of health services can only be assured if people’s participation is secured by States.”
20. The six human rights indicators were chosen based on the baseline survey and on the focus groups held with three different groups of mental health service users in north and west Belfast around the issues above.
21. Participation and the Practice of Rights Project (see note 11), p. 56.
22. United Kingdom Department of Health, Safety First: Five Year Report of the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (London: Department of Health, 2001), p. 4.
23. Ibid., p. 8.
24. Emphasis in original. Joint Mater Hospital and North and West Belfast Health and Personal Social Services Trusts, Discharge Protocol (2007).
25. Committee on Economic, Social and Cultural Rights, General Comment No. 14 (see note 6), para. 17.
26. Paul Hunt, report of the UN Special Rapporteur on the right of everyone to the enjoyment of the highest attainable standard of physical and mental health, UN Doc. No. A/HRC/7/11, January 31, 2008. Available at http://daccessdds.un.org/doc/UNDOC/GEN/G08/105/03/PDF/G0810503.pdf.
27. Participation and the Practice of Rights Project, Rights in Action: Changing Mental Health Services, Findings of the International Panel (Belfast: Participation and the Practice of Rights Project, 2007), p. 15. Available at http://www.pprproject.org/images/documents/findings_mh.pdf.
28. G. Hyland, M. Brady and J. Rogers, Final Report of an Independent Review Panel of the Eastern Health and Social Services Board Complaint Made by Mr and Mrs McCartan Concerning the Mater Hospital Trust and North and West Belfast Trust and South and East Belfast Trust (2007).
29. The implementation of the “card before you leave” appointment system was explained in a letter to the PIPS-GSBF Rights Group dated August 8, 2008 and reiterated by the Minister in an article about the work of the PIPS-GSBF Rights Group. C. O’Carroll, “Anti-suicide group seeks urgent action over mental health,” Belfast News Letter (October 21, 2008). The decision to make timely follow-up care (within a week) a Priority for Action was confirmed by a letter to the PIPS-GSBF Rights Group on January 30, 2009.
30. These are not the only bodies with this responsibility. Belfast Trust, however, has direct responsibility for service delivery of appointment systems in the hospitals concerned and for the implementation of any new appointment system.
31. In the letter, Minister McGimpsey stated, “During our meeting on 17th June, you suggested that a ‘card before you leave’ appointment system could be implemented by the end of July. I indicated at the meeting that the Department was working on a response to the Health Committee’s recommendation on this issue. . . . The aim is to have a system in place by the end of April 2009.”
32. The Belfast Health and Social Care Trust is the health service delivery body with responsibility for Belfast. They implement the recommendations of the Department for Health.
33. Official Report of the Northern Ireland Assembly, Committee for Health, Social Services and Public Safety, Families Bereaved by Suicide (July 5, 2007). Available at http://www.niassembly.gov.uk/health/2007mandate/moe/070705b.htm.
34. Northern Ireland Department of Health, Social Services and Public Safety. Draft Terms of Reference: Card Before You Leave (2009).
35. A. Cullen, “Try, Try, Try Again!” in B. McKeever (ed), The Way I See It: Personal Views on User Involvement, Partnership Working, Inclusion and Real Life (Derry: Family Information Group, 2008), pp. 30–32.