Christopher Newdick
Abstract
How should courts supervise health service resource allocation? Although practice varies widely, four broad approaches can be represented on a matrix comparing, on two axes, (a) individual-community rights and (b) substantive-procedural remedies. Examples from each compartment of the matrix are discussed and, although the community-procedural approach is recommended as a general rule, a range of other responses within the matrix may also be desirable.
Introduction
All over the world, public welfare services are struggling as “structural adjustment” reduces the resources available to public authorities.[1] In the past, governments could raise domestic taxes to respond to welfare demand. Now, their revenue-raising capacity is diminishing, especially from the wealthiest and most mobile sources.[2] Instead, governments are turning to international credit to support public services.[3] Today, private investors’ rights to bond repayments compete for priority over public rights to social welfare.[4] As demand for care accelerates, both from older patients living longer with chronic illness and younger ones suffering from our “obesogenic” environment, the tax-state is also becoming the debt-state.[5] While the subject of this article is health care, its context is of mounting pressure on health care systems precisely as demand for care is expanding faster than ever. While we may endorse the World Health Organization’s strong advice for governments to increase public investment in health and health care, the future for public services is more probably of greater austerity.[6] And as competition for limited resources intensifies, judges are more likely to be called upon to resolve the tension. How should they do so? What logic separates the choices before them, and what are the implications for patients and systems as a whole of the judicial policies adopted? In particular, is the “judicialization” of health care a help or a hindrance, friend or foe?[7] We discuss (a) framework issues common to claims made upon public welfare systems everywhere, and (b) a resource allocation rights matrix to assist clarity in the debate.
Framework issues
Before turning to the rights matrix, what are the “framework” issues common to claims arising within public welfare systems generally? Assuming the decision-maker is an authority with duties to serve the public, the following three factors are surely axiomatic.
Opportunity costs engage rights
Because demand for care generally exceeds the public resources available, investment in one part of the system may require disinvestment from another. Judgments about resource allocation are not based on objective equations or immutable logic, but on a balance of ethical, legal, therapeutic, social, and economic values about which reasonable people differ. The term “commissioning” captures the responsibility to promote the interests not just of individuals (the usual priority of bioethics), but of whole communities of people over the longer term. It expresses concern for social citizenship in which we all share common interests with a community of others.[8]
For health care commissioners, this involves decisions about the opportunity costs involved in promoting social and economic rights. For example, how should we allocate resources between neonatal care, pediatric care, orthopedic care, oncology, and cardiology care? Should patients wait for hospital care for 18 days, 18 weeks, or 18 months? Should we focus less on individual patients after illness has struck, or promote community health before people become ill? These are crucial questions in bioethics (although they have been “almost totally ignored”), but they also engage rights.[9] We require responses that recognize social and economic rights as enforceable positive rights yet devise remedies that respect the “public” dimension of the claim in terms of opportunity costs.Positive rights are justiciable
Judges must surely retain supervisory authority over competing claims of this nature. The challenge is to find the proper balance between judicial usurpation of executive authority on the one hand and a complete abdication of judicial responsibility on the other.[10] This suggests that, although positive rights remain within judicial supervision, appropriate remedies must differ from those available for civil and political rights claims. Whereas civil and political rights are enforceable impartially and generally by us all, social and economic rights engage issues of distributive justice between people who may have competing interests, where the needs of the most underprivileged are often prominent. This distinction suggests that whereas civil and political rights are amenable to substantive judicial enforcement, social and economic rights give rise to different concerns. For the latter, procedural remedies are more often appropriate to accommodate the politics inherent in promoting social welfare policy.[11] In the Constitutional Court of South Africa, Justice Albie Sachs explained the difference in a case concerning the allocation of scarce lifesaving kidney dialysis. An individual rights approach was insufficient to solve the problem. When others also have legitimate interests in the same resource, the court must reflect our human interdependence by accommodating the competing rights and interests of other people. This is not to undermine or dilute the notion of rights, rather:
When rights by their very nature are shared and interdependent, striking appropriate balances between equally valid entitlements or expectations of a multitude of claimants should not be seen as imposing limitations on those rights…, but as defining the circumstances in which rights may most fairly and effectively be enjoyed.[12]
Take the European Convention on Human Rights (ECHR). In respect of civil and political rights, the same principles of freedom of speech apply throughout Europe, east and west, irrespective of the differences in gross domestic product (GDP). Thus, despite the differences in national wealth, German and Romanian citizens should enjoy the same rights of freedom of expression, assembly, and religion. However, this is not true of social and economic rights. Inevitably, access to public health, housing, education, and social welfare differs significantly throughout Europe. This is not to say that social and economic rights do not exist in countries with a smaller GDP, or that their courts cannot enforce them. Rather, their legitimacy must be recognized within these constraints, without ignoring the rights of other people. The High Court of Israel refers to them as “budget-dependent rights” in which “the scope and extent of realization of the right to health and medical treatment is subject to the economic capability of the state and the resources at its disposal.”[13] Unless we acknowledge this difference, an individualist approach to social and economic rights will damage precisely the communities and public institutions most in need of protection.[14] The concern is not that social and economic rights are non-justiciable; it is how best to avoid the collision with “negative rights” so as to respond properly to everyone’s needs, rather than the needs of articulate litigants in particular.
Access rights are equality rights
The state treads a delicate line between protecting liberty on the one hand and promoting equality on the other. If the starting point is “individualistic” and premised on the belief that the state is a necessary evil needed only to protect civil and political rights (as with Thomas Hobbes and John Locke), then the conclusion will differ radically from those who believe we are born into communities with social rights, mutual interests, and shared obligations of citizenship (as with Aristotle and Jean-Jacques Rousseau). Take an example that has troubled a number of health care systems. Concern is expressed that the public interest in a fair public health service is undermined if wealthier patients can jump the queue for services by accessing faster or better treatment through private care. Resources otherwise available to the public may be diverted into private practice, and the integrity of public sector care may be diluted. Waiting times in the public system may lengthen, the numbers of doctors and nurses in the wards may shorten, public support for the service may decline, and the ethical commitment to equality may be compromised. Confidence in the system may be undermined so that the service loses credibility.
Both the province of Quebec and the state of Israel responded to this problem in broadly similar ways. In Quebec, regulations made the market for private health insurance unlawful so as to protect the integrity of the public health care system. In Israel, since 1996, patients had been permitted to make extra payments to public hospitals to purchase the right to see the doctor of their choice. As in Quebec, this created a conflict between a right to buy care in a free market on the one hand and the principle that patients should be treated equally according to their need, by the staff best qualified to do so, on the other. So the attorney general of Israel declared the practice illegal in 2002.[15] Both of these social policy responses were challenged. The difference in judicial reaction is illuminating. In Chaoulli v Attorney Generals of Quebec and Canada, the Canadian Supreme Court held that individual rights effectively “trump” public policy concerns, at least until there was cogent evidence that substantial harm would be done otherwise.[16] It struck down the Quebec regulation for infringing the private rights of individuals to enter the market for health insurance by obliging people to wait longer for treatment in the public system. By contrast, in Kiryati v. Attorney General, the Supreme Court of Israel was troubled by a scheme which permitted public health services to be supplemented by private payments. Public hospitals should treat patients equally, according to their need rather than their ability to pay.[17] Yet permitting wealthier patients to divert doctors from other, more needy patients undermined this ideal. Thus, the court upheld the attorney general’s decision as a legitimate measure promoting the fundamental principles of the public health care system in Israel.[18]
Tushnet says of the Canadian decision that it is based on “an unstated assumption that the default remedy is always reversion to the institutions of the private market economy.”[19] Hutchinson criticizes the decision in similar fashion:
Chaoulli… is energised by a political ideology which encompasses, amongst other things, that individual entitlements are more important than social responsibilities, that negative liberty is to be promoted at the expense of positive liberty, that people’s capacity to exercise their rights is a matter of choice rather than circumstance and that legislatures… are the breeding grounds of capricious and arbitrary decision-making… This political vision… is highly individualistic and anti-state…[20]
Courts more comfortable protecting individual liberty will be challenged by policies that constrain economic rights in order to promote equality and social citizenship. Nevertheless, it is surely axiomatic that public health systems should promote everyone’s interests equally, and we need to be candid that these matters of distributive ethics often involve political compromises.[21] The commitment to equality should have regard for the needs of particular patients today, but also to the sustainability of the system for those who need treatment in the future. It is to the balance between political priorities and legal rights that we now turn.
A priority-setting rights matrix
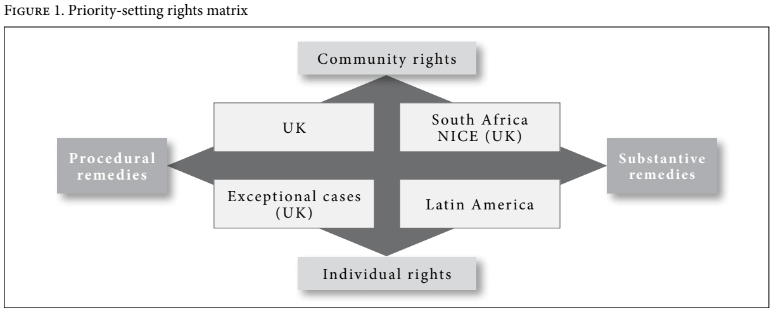
With these framework issues in mind, how should fair and equitable systems of health care resource allocation be designed? Ways of answering this question can be visualized on a rights matrix created from two axes contrasting: (a) on the vertical axis, the distinction between individual and community rights and (b) on the horizontal axis, the distinction between procedural and substantive remedies. This produces four conceptions of rights inherent in claims to public welfare. In its report on universal health coverage, WHO invites us to create “a vision for the future… because the paths countries choose towards universal coverage will necessarily differ.”[22] The matrix responds to that invitation by identifying the logic of the fundamental choices that confront us, the crucial differences between them, and the broad range of merits, or otherwise, of each. Some systems favor one compartment of the matrix rather than another, but many (including the UK system) comfortably occupy more than one compartment, depending on the circumstances of the individual case. The matrix is created as follows and we examine each compartment in turn.
Community-procedural rights and remedies 
Rights in the community-procedural segment of the matrix are concerned to scrutinize the “reasonableness” of decision-making and, if successful, to refer the decision back to public authorities to be reconsidered in the light of the court’s guidance. This describes the accountability for reasonableness (“A4R”) approach to priority setting.[23] The “right” is a guarantee of a fair and reasonable procedure. It is not a right to treatment itself. As the South African Constitutional Court has said, “Courts are ill-suited to adjudicate upon issues where court orders could have multiple social and economic consequences for the community” and impact adversely upon others whose interests are not known to the court.[24] Recognizing the opportunity costs inherent in public health promotion, the objective is to ensure that fair procedures have identified relevant matters and weighed and balanced them properly.
Procedural rights must be more than mere promises of good intentions. For example, Thames Valley National Health Service (NHS) commissioners have had a procedure in place for almost 20 years to balance these claims within a non-statutory “priorities committee,” by means of policy recommendations to local health care commissioners. The committee is subject to standing procedures on membership, regularity of meetings, cross-section of expertise, quoracy, voting rights, submission of evidence, and so on. The committee of 30 people includes NHS clinicians and managers as well as a lay chair, legal advisor, and ethical advisor, and reviews treatments that local stakeholders submit for consideration.[25] The committee is guided by a clinical effectiveness team, which produces a meta-analysis of the clinical research available in respect of treatments under consideration. This health technology appraisal is paid for by contributions from the Thames Valley commissioners, although the priorities committee’s work is unpaid.
As a means of generating fair, consistent, and transparent decisions, the committee is guided by the Thames Valley Ethical Framework of eight principles: (1) equity, (2) health care need and the capacity to benefit, (3) evidence of clinical effectiveness, (4) evidence of cost effectiveness, (5) the costs of the treatment and opportunity costs, (6) community needs, (7) national policy directives and guidance, and (8) exceptional cases.[26]The committee has created a suite of policy guidance to assist local health authorities which, in the majority of cases, CCGs adopt without modification. The guidance supplements National Institute for Health and Care Excellence (NICE) technology appraisals and covers a range of treatments from assisted conception to gender reassignment, percutaneous pulmonary valve implantation, lung metastases, bone-anchored hearing aids, and aesthetic/cosmetic surgery.[27] In each case, local clinicians are invited to submit evidence to the committee in writing and in person. This generates productive dialogue between decision-makers at the patient and community levels and broad cooperation between clinicians and resource allocators. Applying the ethical framework, the committee may recommend that commissioners purchase treatment for the community or decide that the treatment is low priority because, for example, it is too expensive, the clinical evidence is poor, or better treatments are already available. A low-priority treatment is not normally funded unless individual patients will derive significant clinical benefit (see below). The current Thames Valley Priorities Committee commenced work in 2013 and has developed around 70 policy recommendations. Its predecessor, the South Central Priorities Committee, developed more than 100. Policy recommendations are constantly reviewed and updated. Because NHS commissioners must follow NICE’s guidance (as discussed below), the priorities committee does not consider topics previously appraised there. The Thames Valley system is less sophisticated (and less expensive) than a NICE technology appraisal, but it is based on the same logic and purpose.[28] Systems like this confer community-procedural rights and remedies to the extent that their recommendations and processes command respect and recognition in judicial review.
Judicial review in the UK often favors this community-procedural approach. It acknowledges the constraints on the judiciary in terms of accountability and technical capacity, yet subjects the decision-making process to proper scrutiny in respect of the factors considered and the transparency of the process. In England, the NHS Constitution has codified the “hard-look” judicial review principles developed by the courts so they are binding throughout the NHS. Today, the NHS Constitution describes patients’ procedural rights to transparent and accountable decision making.[29] This is a good example of “destabilisation rights” in which judicial intervention provokes a reconsideration of long-standing policies which have never been subject to critical re-evaluation.[30] As Tushnet says, recognizing strong social rights but enforcing them only through weak (that is, non-substantive) remedies may be attractive for developing “human capital” in social welfare rights and a constructive relationship with public authorities.[31] This defers to reasonable systems for decision making. The High Court of Israel took the same view in a challenge to a decision-making tool applied to assist decisions about expensive cancer treatment where the clinical evidence was incomplete. Conceding the breadth of reasonable views surrounding these questions, it said:
It is not up to us to recommend the adoption of one system of prioritization over another, as long as the current criteria comply with the provisions of the National Health Insurance Law, and are based on relevant and reasonable considerations.[32]
Importantly, however, procedural review is complicated at the extremes. At one extreme, “hard look” scrutiny could be so intense as to browbeat decision-makers into conceding every claim. If every case is referred back to be reconsidered, then public authorities may be so intimidated by the courts that they concede every challenge. Clearly, this would be a sham; it would be in effect a substantive-rights response. The proper balance in UK law has been shaped by the case of R v North West Lancashire Health Authority, ex parte A, D & G, in which applicants for sex reassignment surgery succeeded in judicial review because the public authority failed to demonstrate that its refusal to fund the treatment had considered all the relevant circumstances fairly.[33] For example, it had demanded clinical evidence of effectiveness from randomized controlled trials when none were likely to be available for such a small cohort of patients, and it had failed to take into account the patients’ own particular needs. Instead, it introduced a blanket ban on sex reassignment surgery. The court overturned the ban because a rational decision-making framework should have considered such questions.[34] Crucially, recognizing the nature of the treatment, it did not order that treatment be funded. Rather, it insisted upon fair and transparent systems for decision making.
At the other extreme, some jurisdictions prefer procedural review so weak as to render decision making unchallengeable. For example, the Supreme Court of Ireland has refused to go beyond a declaratory remedy. In TD v Minister for Education, education and health authorities had given specific undertakings to the High Court that particular children’s health and education services would be provided. However, the undertakings were not performed for many years and the matter was returned to the court for a mandatory remedy.[35] The trial court found that the timetable for implementation had been subject to “culpable slippage” through “manifest inefficiency,” which led to “the quite scandalous situation which has now obtained for years.”[36] The court ordered that the minister “lives up to his word and carries it into effect… within the time scale specified…” It stated that it was not making or influencing policy; rather it was requiring the public authorities to adhere to policy of its own making. However, the Supreme Court of Ireland emphatically rejected this response and set aside the mandatory order. Chief Justice Keane said “the granting of an order of this nature is inconsistent with the distribution of powers between the legislative, executive and judicial arms of Government mandated by the Constitution.” Even though the order simply enforced the executive’s own policy, it was unacceptable for precluding its right to vary and flex the policy without judicial approval. Justice Murray said the consequence of a mandatory declaration “would be to undermine the answerability of the Executive” with the danger that a minister “would be bound to respond that his hands were tied by an Order of the High Court…” Democratic judicial review, he said
does not… give the Courts jurisdiction to exercise rather than review Executive or legislative functions. Judicial review permits the Courts to place limits on the exercise of Executive or legislative power not to exercise it themselves. It deals with the limits of policy, not its substance.[37]
But this declaratory-only response may be so ineffective as to rob the right of any meaning.[38] Although it exposes the authority to public opprobrium and may lead to better administrative standards in the long run, it does nothing for the litigants in question and may appear to render pointless the considerable time and expense of litigation. Clearly, then, application of the community/procedural response must be alive to these dangers at the extremes.
Also, many courts hesitate as the political and financial dimensions of the complaint expand. We have noted how health care systems are struggling from austerity driven by the politics of neoliberalism. In an English case, for example, a public authority challenged the sufficiency of its annual financial allocation from the central government treasury. The House of Lords rejected its claim. The challenge was to the exercise of political judgment. Deferring to the authority of Parliament, the Law Lords said that it was constitutionally inappropriate to quash financial planning guidance by the secretary of state, implicitly approved by Parliament: “these are matters of political judgment for him and for the House of Commons. They are not matters for judges.”[39] Even with this procedural review, therefore, courts struggle to adjudicate between the “polycentric” claims of competing government departments.[40]
Individual-procedural rights and remedies 
A comprehensive resource allocation system must also be capable of reassuring individual patients as to its competence and, essentially, its compassion and humanity. A necessary consequence is that a general policy not to fund a treatment must be supplemented by a procedure for reviewing individual patients who possess plausible evidence that their circumstances merit an exceptional response. This is an individual-procedural right in the sense that it cannot guarantee access to treatment irrespective of cost. Yet it can reassure individuals that their individual circumstances have been considered properly in a way that is not possible when decisions are made at the community level. The argument is not that the patient has an exceptional illness. Rather, it is that the patient’s circumstances are such that they will derive significant benefit from a treatment not normally visible under the assessment made within the community-procedural approach.
Individual-procedural rights applications should be exceptional. Exceptional cases have opportunity costs of their own: inescapably, “exceptionality” procedures require considerable commitment from doctors and managers with other demands on their time. For this reason, the patient and doctor present evidence that this patient is likely to derive significant clinical benefit from this treatment. For example, principle 8 of the Thames Valley Ethical Framework promises that:
There will be no blanket bans on treatments since there may be cases in which a patient has special circumstances which present an exceptional need for treatment. Individual cases are considered by each respective CCG [Clinical Commissioning Group]. Each case will be considered on its own merits in light of the clinical evidence. CCGs have procedures in place to consider such exceptional cases through their Individual Funding Request Process [IFR].
This is supported by a system in which exceptional funding applications are submitted as Individual Funding Requests, together with supporting clinical evidence, to an IFR panel. This system was challenged in AC v. West Berkshire Primary Care Trust.[41] The applicant was a male-to-female transgender patient who had received the treatment recommended locally. The patient had received hormone therapy intended to develop breast tissue, but remained dissatisfied with her body shape. Accordingly, she applied for prosthetic breast enlargement. However, the IFR panel rejected the application because this treatment is not available to women generally and it would be unfair and inconsistent to offer it to this patient as an exceptional case. Was it fair to compare this patient’s rights with those of the general community of women with similar concerns or, as she argued, should her position be compared to the much smaller number of transgender women undergoing male-to-female transition? There is merit on both sides, but the court found for the health authority and endorsed the reasonableness of its refusal to fund this treatment in fairness to the larger community of “natal” women (as the court described this group).
By contrast, in Otley v Barking and Dagenham PCT,[42] the applicant was a lung cancer patient who had not responded well to the normal treatments. She had paid for experimental treatment with Avastin, more with a view to extending her survival by a matter of months than in expectation of a cure. Otley argued that she should have access to Avastin paid for by the NHS on evidence that her biochemical markers following treatment indicated that it might extend her life and that she was young compared to other lung cancer patients. The court said that her response was sufficiently exceptional and the experimental treatment was preferable. Similarly, in SB v. NHS England,[43] the patient was a boy suffering from phenylketonuria (PKU) and autism. Untreated PKU damages intellectual development, and for most children it is effectively managed through a low-protein diet. However, the patient’s autism made a consistent dietary regime impossible and he argued that this made him an exceptional case (of about 0.03 percent of the population). The court agreed that NHS England was duty-bound to consider whether the patient should have exceptional access to sapropterin dihydrochloride (Kuvan), and referred the case back for reconsideration. Although this remedy is strictly procedural, its substantive implications for the defendants are obvious.[44]
These cases illuminate also how UK courts generally accept that exceptionality should rest on clinical evidence, rather than personal or social circumstances. For example, in R (on app Longstaff) v Newcastle NHS PCT, the patient suffered from hemophilia and had an understandable distrust of human blood products following his brother’s death from contaminated blood. However, with the improvement in techniques for removing blood viruses, his request to be treated with more expensive, genetically modified blood products was rejected because it was not clinically necessary.[45] Similar “exceptionality” discussions have occurred in cases of terminally-ill mothers who have requested treatment to extend their lives so that they might spend as much time as possible resettling their young children.[46] These troubling cases obviously cause considerable concern.
Community-substantive rights and remedies 
NICE provides an example of community-substantive rights. The institute was introduced as a political expedient to encourage greater consistency among health authority commissioners in England who were otherwise free to differ from one another. This created disquiet because it could give rise to different policies governing access to treatment between health authorities. Consistency has improved after regulations were introduced requiring commissioners to purchase all the treatments NICE recommends in its technology appraisal guidance (TAG).[47] NICE has published over 300 TAGs, and patients may seek judicial review to enforce entitlement to the listed medicines.[48] This political initiative is having increasing community impact as NICE expands its work. NICE also publishes non-mandatory recommendations and these too may have a substantive impact on community rights. In Rose v. Thanet CCG, NICE published non-binding recommendations concerning the freezing of human reproductive material for patients undergoing chemotherapy.[49] The defendant health authority failed to adopt the guidance because it disagreed with it, although it could not present persuasive reasons why. The court held this to be irrational. NICE is an internationally recognized authority; if a health authority intends to depart from its non-mandatory guidelines, it is entitled to do so if it can advance cogent reasons for its decision. The case was referred back to be reconsidered. Here too, although a procedural response, the community-substantive implications for the defendants are obvious because evidence of the quality the court demanded was unlikely to be available.
Judges may also create community-substantive remedies on their own initiative. For example, in Minister of Health v Treatment Action Campaign, the Constitutional Court of South Africa ordered the state to remove restrictions on patients’ access to the drug nevirapine, a treatment to reduce the risk of mother-to-child transmission of HIV, but left to government discretion how best to make it available.[50] So too, in a case involving large numbers of homeless people claiming constitutional rights to housing and shelter, the court ordered, without prescribing specific standards, that the defendants:
within four months of the date of this order to deliver a report or reports under oath, stating what steps it has taken to comply with its constitutional and statutory obligations as declared in this order, what future steps it will take in that regard, and when such future steps will be taken.[51]
Recognizing the political challenge raised by opportunity costs, this returns the matter to legislative policy-makers for a solution.
Similarly, the German Constitutional Court in the Asylum Seekers’ Benefits case of 2012 considered the levels of welfare available to support asylum seekers. Welfare levels had not increased since 1993, and the court noted that inflation had eroded the real terms value of those benefits by 30%, rendering the level of subsistence incompatible with a “dignified minimum existence.”[52] Although the court imposed a constitutional duty upon government to recalculate the benefits, it expressly left the ways and means of doing so to the discretion of parliament. The judges recognized the substantive rights of an entire class represented by these litigants and insisted on a response equally available to the entire group. In this way, it encouraged policies which grappled properly with the public dimension of the challenge. So too in the UK in the asylum seeker case of Limbuela. Government passed regulations which made it impossible for those who delayed their application for asylum to work or to obtain social welfare. The case involved an applicant for asylum who applied outside the time limits, without access to food, or shelter and who often slept rough, outside at night in the cold and wet. The House of Lords found that the action of the state amounted to degrading treatment in breach of Article 3 of the European Convention on Human Rights. It decided that substantive social welfare had to be provided to everyone in these circumstances pending the resolution of their application for asylum.[53]
Perhaps the most ambitious attempt to introduce community-substantive rights has been from the Colombian Constitutional Court in a case that sought to set up new structures around the health care system, emphasizing the role of equality, accountability and participation.[54] Public Interest Litigation (PIL) in India promotes a similar community-substantive approach.[55] Judicial commissioners may be appointed to collect evidence and make recommendations to the court, but this too, while successful in some areas, is confronted by challenges.[56] For example, in PIL to reduce female infanticide and feticide the Supreme Court of India observed that “neither the State Governments nor the Central Government has taken appropriate actions for its implementation” (despite robust statutory regulations banning the practice).[57] Public authorities were ordered to implement the regulations, monitor their implementation, make quarterly returns of progress, take appropriate action, conduct public awareness campaigns, and introduce and enforce a code of conduct for public authorities. The public authorities were required to return to the court within three months to report on their progress. Similar action has been taken in respect of enforcing rights to education, health, and freedom from sexual harassment. Entering into collaboration to enforce existing regulations of significant public interest, based on reason and transparency, provides a good example of the power of PIL to encourage change.[58] On the other hand, the substantive-community response of PIL has not improved the systemic under-investment in health care by successive Indian governments.[59]
Individual-substantive rights and remedies 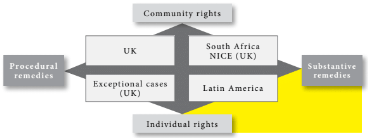
Latin American jurisdictions are often cited as the paradigm example of individual-substantive rights. Within this logic, public rights are enforceable as if they are private contractual rights arising within a contract for private health insurance. Community interests are not foremost. In Brazil, for example, it is reported that 97% of the rapidly increasing claims for access to health care are made by individual litigants requesting particular treatment.[60] In one case, the Supreme Federal Tribunal determined that drug eculizumab (Soliris), should be funded for an orphan disease at an annual cost per patient of more than US$400,000.[61] But Latin America is not alone. The European Court of Justice has developed similar, individualized rights to publicly funded health care from the principles governing the free movement of services in the European Union. In a series of decisions, the court has promoted the idea that, as a general rule, patients are entitled to obtain treatment away from their own member state when (i) the treatment is included within the basket of services available and regarded as “normal in the professional circles concerned” and (ii) it cannot be obtained at home “without undue delay.”[62] As it said in R (Watts) v. Bedfordshire PCT, although resourcing restraints are relevant in the extreme event of a “risk of seriously undermining the financial balance of a social security system,” a refusal to authorize treatment in the EU was not justified by waiting lists based on clinical priorities without carrying out, in the individual case in question, an objective medical assessment of the patient’s medical condition.[63] The court continued,
where the delay arising from such waiting lists appears to exceed in the individual case concerned an acceptable period having regard to an objective medical assessment of all the circumstances of the situation and the clinical needs of the person concerned, the competent institution may not refuse the authorisation sought on the grounds of the existence of those waiting lists, [or] an alleged distortion of the normal order of priorities linked to the relative urgency of the cases to be treated.[64]
Here too, by disregarding those not represented before the court, the court blinds itself to the opportunity costs upon the community of patients generally.[65]
The challenge of “individual-substantive” remedies is most sensitive in applications for expensive, “last chance, life-saving,” pharmaceuticals where evidence of efficacy is disputed. Measured on the quality-adjusted life year (QALY) scale, drugs of this nature may do no harm and may even assist a small proportion of patients for a limited time, yet absorb disproportionate resources otherwise available for other patients. Some might defend this as protecting an “existential minimum” commensurate with human dignity. Such an approach may be extended to patients with potentially fatal conditions by permitting substantive rights of access to treatments even when there is incomplete clinical evidence it will be effective. In Nikolaus,[66] the patient suffered Duchenne muscular dystrophy, a progressive and fatal disease for which there is no cure. The German Constitutional Court found that the constitution guaranteed those suffering a life-threatening disease for which there was no generally accepted treatment, access to medically approved treatment, even if a positive influence on the disease was unlikely. However, a single-minded “rule of rescue” which ignores finite public budgets exposes the community to considerable risk.[67] Unrestricted individual-substantive responses are poor examples of Sabel and Simon’s “destabilisation rights,” which encourage a more secure and constructive platform upon which to exercise public duties.[68] The danger is obvious. Lack of restraint over individual-substantive rights, far from encouraging constructive “destabilisation,” could be destructive of the rights of the many.
The European Court of Human Rights (ECtHR) has taken the opposite view in respect of patients seeking life-saving treatment outside their own health system. In N. v. United Kingdom, the ECtHR reconsidered its “individual-substantive” rights approach previously adopted in D. v. United Kingdom.[69] The case concerned an HIV-positive visitor to the UK who was offered full access to NHS treatment while staying in the country. When her visitor visa expired, immigration authorities sought to remove her, knowing she would be unlikely to receive further treatment in her home state. Retreating from their decision in the case of D., the court declined to insist on a substantive remedy. Instead, it referred to the “search for a fair balance between the demands of the general interest of the community and the requirements of the protection of the individual’s fundamental rights…” It continued,
social and economic differences between countries, entail that the level of treatment available in the Contracting State and the country of origin may vary considerably… [However] Article 3 does not place an obligation on the Contracting State to alleviate such disparities through the provision of free and unlimited health care to all aliens without a right to stay within its jurisdiction. A finding to the contrary would place too great a burden on the Contracting States.[70]
This denial of individual-substantive rights is difficult, but it acknowledges the macro-implications to states of unrestricted rights of access. Unattractive as it is from a patient-centered perspective, it clearly locates its analysis within a community-based approach to rights.
Conclusion
Is judicialization a friend or a foe? The rights matrix illuminates the range of approaches available to courts, their costs and benefits. If we accept the framework issues discussed above, that is, that opportunity costs engage everyone’s rights and a central objective of public welfare rights is to mitigate health inequality, then the logic of the community-procedural approach (“A4R”) is the most compelling starting point to preserve legislative political will and promote community rights. Equally, a number of factors may modify this ideal. Community-procedural approaches are most likely to succeed in an environment of trust and dialogue between health managers and judges, supported by satisfactory priority-setting systems. But this approach cannot always dominate all others. First, even within the community-procedural dimension, individual circumstances sometimes merit consideration for exceptional clinical reasons. Second, especially in serious cases of hardship, a substantive approach to community interests may be justified when entire groups of patients have been left behind. Indeed, as NICE demonstrates, community-substantive rights are also recognized as a response to the “politics” of resource allocation.[71] Lastly, in jurisdictions of limited trust between resource allocators and the judiciary, or where patients’ rights are thought to be inadequate, judges may feel justified to take a more robust, individual-substantive approach both for the benefit of individual applicants and, indeed, to attempt to destabilize the system to kick start improvement. However, as the funds available for public welfare continue to erode relative to demand, there is a serious threat to community interests if the individual-substantive approach becomes the predominant response.
Perhaps it would help if judges were more transparent about which approach they were engaging and why. The matrix illuminates the costs and benefits of judicial policy, and transparency would assist and clarify debate. That said, we should not overestimate the capacity of national courts to respond to these challenges alone for two reasons. First, while the primary concern of this discussion has been priority setting in health care, do not forget health status more generally, and the social determinants of health in particular. Yet this engages the polycentric needs of other departments of state with complimentary responsibility for the environment, employment, food, housing, and education, about which, as we have noted, courts find adjudication very difficult.[72] Second, as the “debt-state’s” obligations to private creditors expands and private investment underpins public welfare finances, the forum for dispute resolution will tend to move away from national judges into the less secure (and vastly more expensive) hands of international arbitrators.[73] The matrix is helpful, but for the future, as concern about health and health care escalates, national courts and, indeed, national politics, may have a smaller role to play.
Acknowledgments
With the usual caveats, I thank Professors Alicia Yamin, Ricardo Perlingeiro, and Keith Syrett for their helpful discussions during the preparation of this article.
Christopher Newdick is a professor of health law at the University of Reading, Reading, UK.
Please address correspondence to Christopher Newdick. Email: c.newdick@reading.ac.uk.
Competing interests: Author is a member of the Thames Valley Priorities Committee.
Copyright © 2018 Newdick. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
[1]. See Structural Adjustment Programmes http://www.who.int/trade/glossary/story084/en/. See F. Fall et al, Vulnerability of social institutions (2014, OECD Economics Department Working Papers, No. 1130), paras 39-51. See also K. Farnsworth and Zoe Irving, “Varieties of crisis. Varieties of austerity: Social policy in challenging times,” (2012) 20 J. Poverty and Social Justice 135.
[2]. See R. Avi-Yonah, “Globalization, tax competition, and the fiscal crisis of the welfare state,” (2000) 113 Harvard Law Review 1573. See also F. Alvaredo et al, World Inequality Report (2018, World Inequality Lab).
[3]. General government gross financial liabilities as a percentage of GDP, OECD, 2015 http://www.oecd-ilibrary.org/economics/government-debt_gov-debt-table-en.
[4]. See M. Mazzucato, The enterprise state (Anthem Press, 2013).
[5]. W. Streek, Buying time – the delayed crisis of democratic capitalism (2014, Verso, London) and Sovereign borrowing outlook for OECD countries OECD, 2017. On the conflict emerging between human rights and private international law, see D. Desierto, Public policy in international economic law – the ICESCR in trade, finance and investment (Oxford University Press, 2015); G. Van Harten, Sovereign choices and sovereign constraints – judicial restraint in investment treaty arbitration (Oxford University Press, 2013) and S. Joseph, Blame it on the WTO? – A human rights critique (Oxford University Press, 2013).
[6]. See World Health Report – Financing for Universal Coverage (World Health Organization, 2010) and C. Newdick, “Global Capitalism and the Crisis of the Public Interest,” in S. Breau and K. Samuel (eds), Disasters and International Law (2016, Edward Elgar); L. Haffert and P. Mehretens, “From Austerity to Expansion? Consolidation Budgets, Surpluses and the Decline of Fiscal Capacity,” (2013) MPIfG Discussion Paper 13/16.
[7]. See N. Daniels, S. Charvel, A. Gelpi, T. Porteny and J. Urrita, “Role of the courts in the progressive realization of the rights to health: between the threat and the promise of judicialization in Mexico,” (2015) 1 Health Systems & Reform 229.
[8] C. Newdick, “The European Court of Justice, Trans-National Health Care and Social Citizenship—Accidental Death of a Concept?” (2009) 26 Wisconsin International Law Journal 844 and S. Greer and T. Sokol, “Rules for Rights: European Health Care and Social Citizenship,” (2014) 20 European Law Review 66.
[9]. See N. Daniels, Just health – meeting needs fairly (Cambridge University Press, 2008), p. 81.
[10]. See K. Young, Constituting economic and social rights (Oxford University Press, 2012), ch 5.
[11]. See Eldridge v British Columbia (Attorney General) (1997) 151 DLR (4th) 577 (SCC) on the duty to provide interpreters for hospital patients and R(KB) v Mental Health Review Tribunal and Secretary of State for Health [2002] EWHC 639 on the duty to review the detention of mental health patients. See also K. Noonan, C. Sabel and W. Simon, “Legal Accountability in the Service-Based Welfare State: Lessons from Child Welfare Reform,” (2009) 34 Law & Soc. Inquiry 523, 561.
[12]. Soobramoney v Minister of Health, KwaZulu-Natal (1999) 50 BMLR 224, 239.
[13]. See 3071/05 Gila Luzon, [2006] (2) Isr LR 1, [16]. See generally, A. Gross, “The right to health in Israel between solidarity and neoliberalism,” in (eds) C. Flood and A. Gross, The rights to health at the public/private divide – a comparative global study (Cambridge University Press, 2014).
[14]. See R. Hirschl, Towards juristocracy – the origins and consequences of the new constitutionalism (Harvard University Press, 2007), pp. 154-55.
[15]. See A. Gross in “The right to health in Israel between solidarity and neoliberalism,” in (eds) C. Flood and A. Gross, The right to health at the public/private divide – a comparative global study (Cambridge University Press, 2014), 178-81.
[16]. Chaoulli v Attorney Generals of Quebec and Canada 2005 SCC 35.
[17]. HCJ 4253/02 Kiryati v Attorney General (2009).
[18]. See A. Gross, “Is there a human right to private health care?” (2013) J. Law & Medical Ethics 138.
[19]. M. Tushnet, Weak courts, strong rights – judicial review and social welfare rights in comparative constitutional law (2008, Princeton University Press), p. 260.
[20]. See A. Hutchinson, “Condition critical: the constitution of health care,” in (eds) C. Flood, K. Roach. and L. Sossin, Access to health. access to justice (2005, Toronto University Press), pp. 109-10.
[21]. J. Coggon, What makes health public? (Cambridge University Press, 2012).
[22]. World Health Report – Financing for Universal Coverage (World Health Organization, 2010), p. 91.
[23]. See N. Daniels, Just health – meeting needs fairly (2008, Cambridge University Press).
[24]. Minister of Health v Treatment Action Campaign 2002 (5) SALR 721, 722 (SACC). See also Government of the Republic of South Africa v Grootboom 2000 (11) BCLR 1169 (SACC).
[25]. Thames Valley Priorities Committee Annual Report 2016-17. Available at http://www.fundingrequests.cscsu.nhs.uk/wp-content/uploads/2016/08/TVPC-Annual-Report-2016-2017.pdf. The Committee’s Terms of Reference are at http://www.fundingrequests.cscsu.nhs.uk/wp-content/uploads/2015/08/TVPC-ToR-March-2016-final.pdf.
[26] . See http://www.fundingrequests.cscsu.nhs.uk/wp-content/uploads/2015/08/Ethical-Framework-March-2016-final.pdf.
[27]. Policy Guidance is searchable at http://www.fundingrequests.cscsu.nhs.uk/thames-valley-priorities-committee.
[28]. See C. Newdick, “Accountability for rationing – theory into practice,” (2005) 33, J. Law, Medicine & Ethics 660.
[29]. NHS Constitution, Principle 2a: “You have the right to expect local decisions on funding of drugs and treatments to be made rationally following a proper consideration of the evidence. If the local NHS decides not to fund a drug or treatment you and your doctor feel would be right for you, they will explain that decision to you.”
[30]. C. Sable and W. Simon, “Destabilisation rights: how public law litigation succeeds,” (2004) 117 Harv L Rev 1015. See also, K. Syrett, Law, legitimacy and the rationing of health care, (2007).
[31]. M. Tushnet, Weak courts, strong rights – judicial review and social welfare rights in comparative constitutional law (2008, Princeton University Press), 251.
[32]. 3071/05 Gila Louzon, [2006] (2) Isr LR 1, [28].
[33]. See generally, C. Newdick, Who should we treat? – rights, rationing and resources in the NHS (Oxford University Press, 2005).
[34]. R v North West Lancashire Health Authority, ex p A, D & G (2000) BMLR 148. See also Van Kuck v Germany (2003) App no 35968/97 and against Poland in an abortion case in RR v Poland (2011) App no 27617/04.
[35]. FN v The Minister for Education [1995] IR 409.
[36]. FN v The Minister for Education [1995] IR 409.
[37]. TD v The Minister for Education [2001] I.R. 259, 333.
[38]. Re S (FC) [2002] UKHL 10, [43].
[39]. R v Secretary of State for the Environment, ex p Nottinghamshire CC [1986] AC 240.
[40]. L. Fuller, “The limits and forms of adjudication,” (1978) 92 Harv L Rev 353.
[41]. [2011] EWCA Civ 247.
[42]. Otley v Barking and Dagenham PCT [2007] EWHC Admin 1927.
[43]. [2017] EWHC 2000 (Admin).
[44]. Following the Court’s guidance, NHS England reversed its decision and committed £100 per day to fund this treatment, see: “NHS agrees to fund ‘life-changing’ drug for seven-year-old,”
http://www.bbc.co.uk/news/health-41443330 (29 September 2017).
[45]. R (on app Longstaff) v Newcastle NHS PCT (2004) Lloyds Rep Med 400.
[46]. Rogers v Swindon PCT [2006] EWCA Civ 392 [2006] Lloyds Rep Med 36.
[47]. See now the National Health Service Commissioning Board and Clinical Commissioning Groups (Responsibilities and Standing Rules) Regulations 2012, SI 2996, reg 34.
[48]. See NICE TAG Static List: https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance/technology-appraisal-static-list.
[49]. [2014] EWHC 1182 (Admin).
[50]. Minister of Health v Treatment Action Campaign (no 2) (2002) 5 SA 721 (CC).
[51]. City of Cape Town v Neville Rudolph and Others 2003 (11) BCLR 1236 (C), at 56.
[52]. Asylum Seekers Benefits Case (1 BvL 10/10, 2012), para [69], http://www.bverfg.de/entscheidungen/ls20120718_1bvl001010en.html (English translation).
[53]. R (Limbuela) v Secretary of State for the Home Department [2007] 1 All ER 951.
[54]. See D. Landau, “Political institutions and the judicial role in comparative constitutional law,” (2010) 51 Harv. Int Law J 319.
[55]. See Gupta v Union of India (1981) Supp SCC 87, 210.
[56]. S. Fredman, Human rights transformed – positive rights and positive duties (Oxford University Press, 2009), p. 134 and generally.
[57]. Centre for Enquiry into Health and Allied Themes v Union of India (2001) 5 SCC 577, under the Pre-natal Diagnostic Techniques (Regulation and Prevention of Misuse) Act 1994. The order is available at: http://judis.nic.in/supremecourt/imgs1.aspx?filename=20508.
[58]. See generally, C. Foster and V. Jivan, “Public interest litigation and human rights implementation: The Indian and Australian Experience,” [2008] 3 Asian Journal of Comparative Law 1.
[59]. J. Dreze and A. Sen, An uncertain glory – india and its contradictions (Penguin Books, London, 2014).
[60]. O. Motta Ferraz, “Brazil: Health inequalities and courts: the social impact of the judicialisation of health,” in (eds) A. Yamin and S. Gloppen, Litigating health rights – can courts bring more justice to health? (Cambridge, MA: Harvard University Press, 2011), pp. 87, 94.
[61]. See Noticias STF, www.stf.jus.br/portal/cms/verNoticiaDetelhe.asp?Conteudo+281232. Given its orphan status, NICE in England has also approved the drug within strict treatment guidelines, see Paroxysmal Nocturnal Hemoglobinurua-Eculizumab for atypical uraemic syndrome (Nice, 2015, HST Guidance 1).
[62]. Smits and Peerbooms (1999) C-157/99, para 108. See also Muller-Faure and Van Riet (1999) ECJ, C-385/99, para 108.
[63]. R (Watts) v. Bedfordshire PCT (2006) ECJ, C-372/04, para 53, although it is difficult to think of single cases having such a destabilising impact.
[64]. Ibid., paras 119-20, emphasis added.
[65]. C. Newdick, “Citizenship, free movement and health care: cementing individual rights by corroding social solidarity,” (2006) 43 Common Market Law Review 1645.
[66]. Case BvR 347/98, 6 December 2005.
[67]. A. Yamin and S. Gloppen, litigating health rights – can courts bring more justice to health? (Cambridge, MA: Harvard University Press, 2011), p. 350. In South Africa, Justice Moseneke noted: “Prohibitive pricing of medicine… would in effect equate to a denial of the right of access to health care.” See Minister of Health v New Clicks South Africa (Pty) Ltd 2005 (2) SA 311, para 661 (CC)(S. Afr) discussed by L. Forman and J. Singh, “The Role of Rights Litigation in Assuring More Equitable Access to Health Care in South Africa,” in (eds) C. Flood and A. Gross, The Rights to Health at the Public/Private Divide (Cambridge University Press, 2014).
[68]. C. Sabel and W. Simon, see note (30).
[69]. D. v United Kingdom (1997) 42 BMLR 149.
[70]. N. v United Kingdom (2008) App. No. 26565/05).
[71]. See, for example, Coggon (note 21, above) and T. Marmor and R. Klein, Politics, health and health care: Selected essays (New Haven, CT: Yale University Press, 2012).
[72]. C. Newdick, “Health equality, social justice and the poverty of autonomy,” (2017) 12 Health Economics, Policy and Law 411.
[73]. See, for example, A. Kullick, Global public interest in international investment law (Cambridge University Press, 2012).
