Transforming Policy into Justice: The Role of Health Advocates in Mozambique
Ellie Feinglass, Nadja Gomes, and Vivek Maru
Abstract
Despite expanding policy commitments in many poor countries, health care is often a failure at the point of delivery. Lack of information, poor enforcement, and power dynamics prevent those whose rights have been violated from pursuing redress. In Mozambique, grassroots health advocates work to address this gap between policy and reality by blending approaches known as legal empowerment and social accountability. They raise awareness of health policy, support clients to seek redress for grievances, and facilitate problem-solving dialogues between communities and health facility staff. In three years we have seen communities begin to overcome a culture of silence. Twenty-one advocates and their clients have achieved redress to over a thousand grievances across 27 health facilities. These cases have resulted in improvements to access, infrastructure, and provider performance. Advocates have supported village health committees to transform themselves from collections of names on a list into active agents for change. Advocates should not be trained and left alone—they are most effective when integrated into a vertical team that provides continuous support and supervision, and that can engage higher levels of authority to solve tough cases. Aggregate data from cases handled by health advocates provides unique insight into how health policy is working in practice. We draw on that information to advocate for systemic changes that affect the entire country, like better policies for combatting bribery and stronger procedures for responding to grievances. We have found that legal empowerment and social accountability practices interact synergistically. Our preliminary experience suggests that when people are equipped to exercise their rights to health, even a poorly resourced system can improve.
How health systems fail
Alcina*
Alcina has lived her entire life in an isolated coastal village in Mozambique’s southern region, without access to electricity, running water, or transport. She gave birth to her three children at the local health center—a 17km trek from her home—in 2008, 2012, and 2014. Within moments of each delivery, she was forced to get out of bed and fetch water from the borehole to wash the soiled sheets. “When my daughter was born last year, the nurse and the cleaner didn’t treat me with courtesy. I was treated very badly. I was insulted, and when I complained that I was in pain, the cleaner told me to lie back down, and then she slapped me on the face.” Alcina continues, “Many women didn’t want to go to the health center. They preferred to give birth at home.”
Jorge*
At a bustling health center on the outskirts of Maputo, nearly 8,000 patients living with HIV receive care and treatment. The health facility did not have a CD4 machine on-site (essential for measuring the level of immunosuppression in HIV patients), so blood samples were being transported to a nearby hospital for analysis. Patients’ test results were frequently misplaced and delayed, sometimes for months. In October 2015, one of these patients—Jorge—had to return to the health center three times to repeat his blood draw. Each time, he arrived by 6:30 am and waited in line for more than four hours. A medical technician at the health center recalls: “I felt as though I was doing a real disservice to my patients—that I was unable to provide quality care in the absence of a CD4 history. It was impossible to get results back, even for those who were gravely ill.”
Introduction
Despite expanding policy commitments in many poor countries, health care is often a failure at the point of delivery.1 Practice does not match policy, in part because health facilities are hard to reach and severely understaffed. In addition, stigma, discrimination, fear, and a pervasive lack of information keep people from seeking and receiving care.2 This is particularly true for vulnerable groups such as people living with HIV, women, adolescent girls, orphans and child heads of household, the elderly, and the disabled. Efforts to improve health outcomes around the world primarily focus on the mechanics of delivering care, including clinical training, drugs, and infrastructure. But it is increasingly clear that strengthening the accountability of services to patients is essential if those investments are to succeed.3
In this journal in 2010, one of us (Maru) proposed strengthening the accountability of services to people through a synthesis of two approaches: legal empowerment and social accountability.4 Legal empowerment efforts help people to understand, use, and ultimately shape laws and policies. Legal empowerment organizations often deploy grassroots legal advocates—sometimes known as barefoot lawyers, or community paralegals—who form a creative, problem-solving frontline that can bring law closer to people.5 The term “social accountability” refers to efforts that “inform citizens about their rights and status of service delivery and encourage participation” in pursuit of fairer, better services.6 Despite substantial overlap in mission, these communities of practice have tended not to interact.
In the earlier Health and Human Rights article, Maru observed that some social accountability interventions focus exclusively on pressuring local service providers, without engaging the wider network of state authority. Legal empowerment efforts, meanwhile, specialize in pursuing remedies from a range of institutions. On the other hand, legal empowerment organizations have not typically gathered data to proactively identify systemic failures. This is something social accountability groups are known for. For these reasons, Maru argued that the two approaches could work well in tandem.
Drawing on similar observations, Jonathan Fox and others have recently highlighted integrated approaches to accountability, which span vertical levels of authority (local, provincial, and national) and engage horizontally across public institutions, including not just the executive, but also, for example, the courts, parliaments, human rights commissions, and ombuds offices.7
We reflect here on our experience attempting an integrated approach to the accountability of health services in Mozambique. We work with a group, Namati, that is dedicated to legal empowerment. Namati and its partners deploy grassroots legal advocates who help clients protect community lands, enforce environmental law, and secure basic rights to health care and citizenship. Namati also convenes the Global Legal Empowerment Network, which is made up of more than 700 groups from 150 countries. Namati aims to foster learning and collaboration across that wider community. In Mozambique, Namati is registered as a national NGO recognized by the Ministry of Justice. All but one of its 38 staff members are Mozambican.
The grassroots advocates at the center of the effort in Mozambique are called defensores de saúde, or health advocates. They engage in three kinds of work. First, they raise awareness of health policy—something common to social accountability and legal empowerment. Second, they engage in case work—supporting clients to resolve specific grievances with respect to health services. This approach comes explicitly from the legal empowerment tradition. Third, drawing from the social accountability experience, defensores support dialogue between communities and health facility staff to proactively identify and address system failures.
This essay draws on our own reflections as practitioners and on internal program data. We are currently working with independent researchers to undertake an external evaluation—the researchers will publish those results in a future paper.
We begin with a snapshot of both the reality and the policy of health care in Mozambique. We then describe the three key elements of our approach before returning to the stories of Alcina and Jorge and reflecting on our experience to date. We discuss 1) how we have attempted to overcome a culture of silence about breaches of health rights, 2) the kinds of improvements to health services we have achieved, 3) our experience mobilizing village health committees, 4) the importance of providing adequate supervision and support to frontline advocates, and 5) our effort to translate grassroots experience into system-wide change.
Mozambique context
Health and development
Despite having endured a brutal civil war from 1977 until 1992—a devastation compounded by recurrent droughts and flooding—Mozambique has made considerable strides in reconstruction and public health. In the two decades since the conflict ended, under-five mortality has declined by more than 50%. In 2003, the government established a free national HIV care and treatment program. The number of people receiving lifesaving antiretroviral therapy (ART) quadrupled from 200,000 in 2010 to 800,000 in 2016.8 But Mozambique is still at the bottom of the Human Development Index, ranking 180 out of 188 countries in 2015.9 More than 40% of children are stunted as a result of chronic illness and malnutrition, and the maternal mortality rate remains among the highest in the world.10 Even with the recent expansion of HIV services, ART retention rates are low.11 The challenges include extreme poverty and inequality, vast distances to health facilities, and a profound shortage of health care providers. Mozambique has 0.4 physicians and 4.1 nurses and midwives per 10,000 inhabitants––one of the lowest health worker densities in sub-Saharan Africa.12
Law, policy, and the right to health
Articles 89 and 116 of the Mozambican Constitution recognize the right to health, guaranteeing that “the State shall promote the extension of medical and health care and equal access of all citizens to the enjoyment of this right.”13 The Constitution also provides for the right to ‘popular action,’ under which individuals or groups can bring a case to court in relation to issues such as public health, consumer rights, and environmental conservation, though no such case has ever been raised in relation to public health.13
The Charter on Patients’ Rights and Obligations (Carta dos Direitos e Deveres dos Utentes), adopted by the Ministry of Health in 2006, elaborates on the centrality of human rights in health services, highlighting human dignity, equality, and ethics as fundamental values. The charter prohibits discrimination on the basis of health status and guarantees the confidentiality of patient information. It gives all patients the right to voice suggestions and grievances, and the right to a timely response.
The Law on Protection of the Individual, the Worker, and the Candidate for Employment Living with HIV and AIDS (Lei da Protecção da Pessoa, do Trabalhador e do Candidato a Emprego Vivendo com HIV e SIDA; Lei no 19/2014) specifies the rights of people living with HIV, including information, free treatment, and protection from discrimination.15
Mozambique has ratified a number of global treaties, including the Convention on the Rights of the Child, the Convention for the Elimination of all Forms of Discrimination against Women, and the International Convention on the Rights of Persons with Disabilities.
In addition to these national and international legal instruments, the Ministry of Health has developed a range of powerful policies and clinical protocols. The impact of these laws and policies, however, is undermined by insufficient dissemination, poor enforcement, low literacy rates, and power dynamics that prevent those whose rights have been violated from pursuing redress.16
Namati’s approach
Defensores de saúde work to address this gap between policy and reality by supporting communities in exercising their basic rights to health. They present themselves not as watchdogs who would police health care providers but rather as supporters of the system and its staff, many of whom themselves do not have access to the resources or essential information they need to work effectively. We share the same fundamental goal as the government: to improve health outcomes in Mozambique. This framing has been critical in building constructive relationships with both health care providers and Ministry of Health leadership.
We have four criteria when recruiting health advocates: problem-solving ability, a secondary school education, proficiency in reading and writing, and a proven commitment to the common good. As of this writing, Namati employs 21 full-time health advocates: 12 women and 9 men. Each advocate is responsible for between one and three health facilities, depending on patient volume and geographic coverage. Health advocate catchment areas range from 23,000 to 115,000 people (with larger catchment populations in urban and peri-urban facilities). Three program officers and a small technical team provide the advocates with ongoing support.
Namati began working in primarily rural areas of two districts in southern Mozambique in March 2013. One year later we launched a partnership with MSF in several sites in Maputo city. In May 2015, we expanded further to two high-volume government health centers in Matola, and we are now establishing operations in five districts of Inhambane province.
Selection of districts for the initial phase was based on our commitment to conducting regular and intensive supervision, and at the same time containing travel-related costs given our limited budget at the outset. We have viewed this as Phase I of our work, during which we have focused on implementation research to identify a socially grounded model through a process of trial and error. We adapted the program based on regular input from communities and providers and evidence about what was working and what was not.17
We have conceived of the learning and tweaking as valuable experimentation, along the lines of what Lant Pritchett and colleagues call “structured experiential learning.”18 We are guided as well by Mansuri and Rao’s findings about participatory approaches to development—that “context, both local and national, is extremely important” and that “strong built-in systems of learning and monitoring, sensitivity to context, and the willingness and ability to adapt are therefore critical in implementing projects.”19
Our model has evolved to involve three core elements: increasing awareness of health policy, pursuing solutions to specific breakdowns in health care delivery, and facilitating dialogue between communities and clinics. We have found that when integrated, these approaches offer powerful synergies.
Providing essential information and education: The foundation for action
Health advocates strive to make health-related laws, policies, and protocols accessible to everyone. They address large groups of patients in health center waiting areas. They visit schools, farmers’ associations, women’s cooperatives, and HIV support groups. They go door to door, speaking with people in their homes. Increasingly, they also engage the public through newspapers, television, and radio.
We take inspiration from South Africa’s Treatment Action Campaign (TAC). Forbath describes TAC as “a model for methods of education, outreach and institutional reform that help equip and enable the ‘clients’ of social programs to participate in reforming and reshaping local state institutions and wider systems of social provision.”20 TAC co-founder Mark Heywood writes:
The right to health…may be recognized in international covenants, national constitutions, and jurisprudence. But it cannot be effectively utilized by community activists unless health itself is better understood; nor can the right to health be pursued without connecting it to issues of law, politics, or governance.21
In Mozambique, as in many countries, most health information that reaches grassroots level is about science or behavior rather than policy. People are taught how malaria is transmitted, for example, and why birth spacing is important, but not which medicines or family planning services they’re entitled to.22 Our education efforts intertwine scientific information with specific health protocols so that patients can more effectively advocate for themselves.
Supporting individuals and communities to seek redress for grievances
Many public health facilities in Mozambique have suggestion boxes or registers in place, but they are seldom used. The existing system requires patients, many of whom are illiterate, to submit feedback in writing. Moreover, fear of retribution and imbalances of power tend to silence the most vulnerable citizens when their rights are violated.23 Namati’s health advocates help clients pursue remedies to grievances. They document the problem clearly, analyze it in relation to health policy, and formulate a potential solution. Whenever possible, advocates and clients aim for amicable resolution with local facility staff. When necessary, they seek redress from higher levels of authority in the ministry. Health advocates collect data on every case they handle: client demographics, the specific nature of the grievance, actions taken towards resolution, and outcomes.
Facilitation of community-facility dialogue regarding health system performance
In addition to seeking redress for specific grievances when they arise, health advocates work with communities to take a more proactive role in the governance of their health services. To do so, we engage an existing structure: the village health committee. According to national guidelines, the role of these village health committees is to “mobilize members of the community to identify health problems in general, with a particular focus on those that affect women and children, as well as to identify respective solutions both within and beyond the community.”24
We aim to transform what are often inactive groups into effective institutions for governance. We provide training and ongoing technical support to village health committee members regarding, for example, the patient bill of rights, key health protocols and policies, conflict resolution, and advocacy strategy. Health advocates work with committees to conduct systematic assessments of health services on a biannual basis. The assessment instrument, which incorporates detailed feedback from community members and health workers, assists committees in identifying and prioritizing problems related to provider performance, infrastructure, equipment, and medicines.
Committee members and defensores then analyze the root cause of each problem, agree on strategy, and commit to specific actions and timelines. This process will allow Namati staff, communities, and government to track progress on barriers to the right to health over time.
What happens when people stand up for the right to health
Alcina
When Alcina gave birth to her first two children amidst verbal and physical abuse, she recalls having had nowhere to turn. “We felt helpless. We didn’t know what we were supposed to do when things went wrong.” By the time her daughter arrived in early 2014, however, Namati’s health advocate, Hortência, had been working to support communities in the health center catchment area for nearly a year. The village health committee, which had previously existed only on paper, was now an active group of five women and four men who, with guidance from Hortência, had begun conducting advocacy at local and district level and had gained the trust of both community members and health providers.
After Alcina approached several committee members, they went to speak with Leonor, the cleaner, who denied having slapped and mistreated her patient. Several weeks later, they invited Leonor, the head nurse, and a community leader to a meeting, during which they discussed the incident and the potential impact of such behavior on maternal and newborn health. Leonor finally acknowledged her wrongdoing. Over the next few months, Hortência and the health committee members monitored Leonor’s behavior. An elder woman from the community noted:
Leonor has really changed. The way in which she talks to patients is different. She used to berate everyone, but now she treats people well. Since Hortência’s arrival, we have become capable of applying pressure, and things are improving. In the past, the maternity waiting house was always empty, but now there are pregnant women who come.
According to the head nurse, births at the facility have risen from an average of two births per month to as many as 12 to 15, which is slightly higher than the national average for a rural catchment area of its size.
Jorge
One morning in October 2015, a group of six patients living with HIV came to speak with Namati’s health advocate, Abudo, in the waiting area outside the HIV clinic to ask if she could help them track down their CD4 test results. The following week, Abudo, together with two of the patients, met with the head of the health center, who shared their concern that the transport of blood samples and results was increasingly disorganized. She showed them a copy of a request she had submitted to district health management nearly two months earlier, asking for a CD4 machine to be installed permanently at the facility. She had not received a response.
Abudo discussed the case with the program officer, Ofélia, and they then requested a meeting with the district director of health. They spoke about the impact the delayed test results were having on patients’ lives, including money spent, time wasted, and increased illness. The district director agreed that given the high patient volume at the facility, a CD4 machine was justified, but in light of many competing priorities, she could not say when it would be procured. As an interim solution, Abudo collaborated with the head of the health center to improve management of blood samples and results by introducing a logbook and limiting responsibility for transport and documentation to one driver who was trained and supported to take on this task. Patients and providers at the health center soon noticed marked improvements. Ofélia continued to advocate at the district level for allocation of a CD4 machine, and in March 2016 a machine was delivered to the health center. Jorge recalls:
In the past, it was very difficult for me. I live more than 20 kilometers from here. I was very weak, and it was not easy for me to get here every day to check on my results. I wanted to abandon treatment. Today, things are different. The care I get is much better. I know that when I come here I will have my results immediately.
Learning and results
Breaking the silence
A series of focus groups conducted in February 2013 as part of a baseline assessment in our original catchment areas suggested that there was virtually no community engagement in governance of the health sector. People are now beginning to come forward; day-to-day violations that affect many people are being noticed and reported. We are slowly chipping away at the culture of silence.
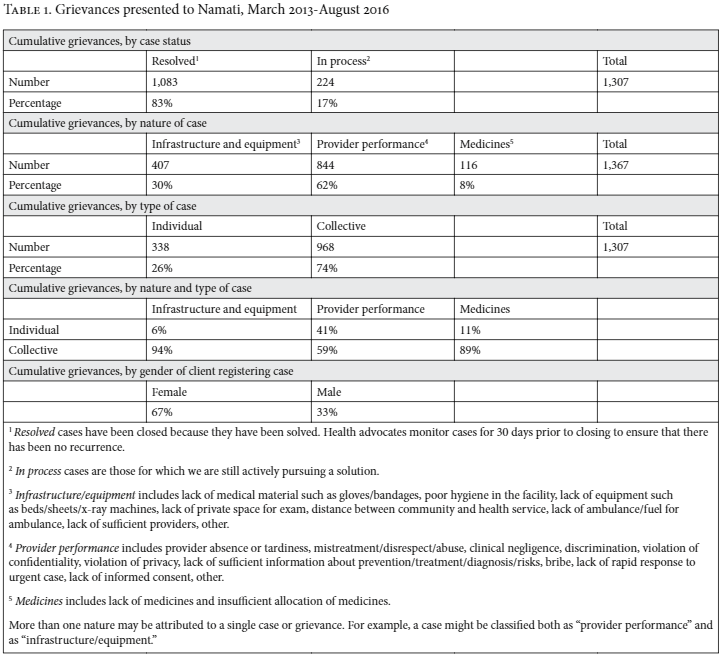
As of August 2016, 21 defensores and their clients have taken on a total of 1,307 grievances across 27 health facilities, of which 83% have been resolved (see Table 1). Seventy-four percent of these cases were collective, directly affecting anywhere from 10 to 10,000 people (for example, lack of privacy at the pharmacy window or inadequate number of beds and/or sheets in the maternity ward). Sixty-seven percent of the clients were women.
Rights awareness is low, and there is a widespread belief that any provision of care, even if delivered with apathy or ineptitude, is a gift bestowed upon the patient. In this context, we view an initial rise in complaints not as a sign that health care is worsening, but as an indication that people are beginning to stand up for themselves.25
One challenge we have encountered is relatively lower demand for the help of health advocates in some rural settings. In remote areas with limited geographic access to services, rights violations are more often acts of omission than acts of commission; the vast majority of people living in isolated rural areas simply do not interact with the health system. The act of not receiving something is less often recognized and reported as a violation, which means that demand for health advocate services can be slow at the outset even while the need is great. We have learned that sharing examples of successful cases can be helpful in mobilizing others to come forward. These success stories have the power to change expectations and to catalyze a ripple effect in the community.
Identifying trends across individual grievances can also lead to proactive collective action. For example, over the course of one year, several individuals brought complaints against the same provider for refusing to attend to patients in labor or those who were gravely ill. Suspecting other unreported incidents, the health advocate and village health committee called a meeting with the broader community, during which six additional grievances were raised against the nurse. Namati then supported the committee in documenting and presenting the series of testimonies to ministry officials. As a result, the provider was relocated from a remote area to a district hospital, and placed under close supervision.
At some of our sites, defensores have helped health providers break their own silence. Many providers struggle to deliver quality services in a system sorely lacking financial and human resources. Some say são as condições que nos temos—this is the reality in which we must operate– and they regard health advocates with indifference or even resistance. But many other providers, like the health center director in Jorge’s story above, have come to view us as allies and have sought the assistance of health advocates in addressing problems that keep them from doing their jobs well.
Improvements in health services
We have seen promising results in our first three years, including improvements in quality of care, access to services, infrastructure, and essential medicines. At one facility, Namati registered a collective grievance regarding the chronic tardiness of the nurse responsible for prenatal consults. The health advocate, Leopoldina, first approached the nurse directly but was rebuffed. She then worked with the health center director to call a meeting of maternal and child health providers, during which the group discussed patient rights and the importance of respecting working hours. In collaboration with several members of the health committee, Leopoldina monitored the situation over the next two months and reported improvements in terms of tardiness and a 50% increase in the number of prenatal exams conducted per day.
We have observed numerous examples of increasing adherence to Ministry of Health protocol. At one site, for example, a patient living with HIV and TB raised a complaint regarding the delay in initiating antiretroviral therapy. According to national policy, patients with HIV and TB co-infection qualify to begin ART immediately. With our health advocate’s intervention, the patient initiated ART and began receiving nutritional support. The nurse then went through the HIV register and identified 15 additional patients in the same situation, and started all of them on treatment.
We have also seen tangible improvements in the geographic reach of services. Health advocates have worked alongside communities and health committees to advocate for bringing community health workers to isolated rural areas that previously had no access to health services; for increasing frequency of existing mobile clinics; and for improving the number and type of services offered at peripheral sites. Whereas in the past, mobile clinics only offered vaccinations and weighing, for example, several now offer malaria testing, TB and HIV care, family planning, and management of chronic diseases such as hypertension and diabetes.
We have managed to resolve more than 70 cases involving access to medicines, but many of these resolutions have been ephemeral. Recently, we worked with an epileptic patient who dropped out of school because her seizures had become too frequent and severe. The local health center and district hospital both told her that medicines for her condition were not available. A health advocate ultimately discovered that the medicine was indeed available in the district government pharmacy stores and helped the patient begin treatment. But solutions like these are limited in that they are often short-term, and do not adequately address the systemic causes of the stock-out, including challenges related to logistics and supply chain management.
More promisingly, defensores de saúde and community members have identified and pushed for a number of low-cost improvements to infrastructure. At one site, we worked with health center leadership to secure modest funding from the district government to construct a wall separating the pharmacy from the consult room, resulting in an increase in patient privacy and confidentiality.
At multiple sites, health advocates received complaints that outpatient bathrooms were inoperative for extended periods—often months at a time. Patients were urinating and defecating in the grass surrounding the health facilities. We were able to resolve these collective grievances through district-level advocacy, which resulted in the application of flexible funds to restore broken toilets. More recently, in a crowded district hospital, we advocated for renovation of an unused structure to be used for TB care, as infectious TB patients were previously congregating in a hallway with little ventilation just outside the prenatal and under-five consult area.
Many of our cases represent egregious violations of the right to health and of human dignity, and yet a substantial proportion of them are relatively easy to resolve if a vocal advocate is committed to pursuing a solution.
The potential power of village health committees
Although the government assigns significant responsibility to village health committees, it has done little to support them. Where they do exist, these committees tend to focus almost exclusively on promoting individual behavior change, tracking down patients who have dropped out of treatment, providing home-based care, and ensuring that the grounds of the health facility are well-maintained.
When Namati began implementation in early 2013, there was not a single functioning health committee in our program catchment areas. In several instances, the names of the committee members were on file at the district level, but on arrival we discovered that a number of these individuals were not aware that they were on the committee. In other cases, committees had dissolved or become inactive.26
Health advocates, together with government partners, have focused on vitalizing these committees, ensuring that empty seats are filled with committed individuals and educating committee members about the full scope of their role and about the details of health policy. These committee members become our “super-clients,” identifying many cases and taking part in regular dialogue and advocacy with the health ministry at local and district levels.
At our strongest sites, these committees embody Namati’s vision of public spiritedness and citizen empowerment. As these committees assume a more active role, health advocates have been able to reduce the intensity of their engagement, increasing their coverage area to include another health facility. If we can reproduce this dynamic, it will make scale-up more plausible and less costly.
Where we have had less success working with village health committees, common factors include members who were selected based purely on political affiliation, lack of motivation to engage in unpaid work, and limited capacity of the health advocate supporting the committee.
The vital role of supervision, support, and a vertical network for the pursuit of justice
Health advocates cannot fulfill their potential if left on their own. The advocates need to be connected to a larger team—including each other, lead advocates, program officers, and senior experts in public health and law—for two reasons.27 First, continuous supervision and support is necessary to ensure that advocates are consistently serving with excellence. We bring the entire team together every two months to provide updates on policy and science and to share emerging challenges and good practices. Our program officers and lead advocate also conduct regular visits to each advocate. The visits are an opportunity to review case files, watch the advocate in action, and discuss strategy on difficult cases.
We have a developed a method of internal spot-checks, whereby our database randomly selects several recently closed cases every month for review. The monitoring and evaluation officer reviews the files in these cases and conducts separate interviews with the advocates and clients involved.
Client feedback on questions such as “were you satisfied with how the case was handled?” and “how can we do better?” helps us monitor the quality of the advocates’ efforts. We also ask, “can you describe the process of resolving the case?” “did you learn anything and, if so, what?” and “have you helped anyone else since?” The three latter questions give us a sense of whether we are genuinely achieving legal empowerment, whereby the advocates are not solving problems on behalf of clients (“I will solve this for you”), but rather the clients are taking an active role (“we will solve this together”), and in the process, clients are becoming more knowledgeable and capable of advocating for themselves in the future.
Several health advocates have interacted with government health staff in a confrontational manner, which is counterproductive. In these circumstances, we have found it useful to establish informal mentorships through which the health advocate who is having difficulty spends time shadowing another, more experienced health advocate.
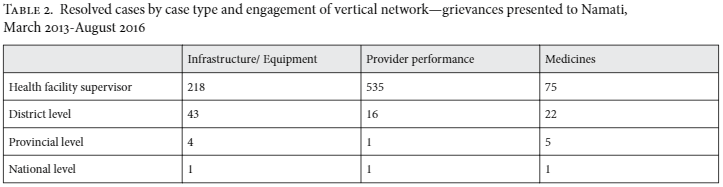
In addition to quality control, the second crucial function for the support network around health advocates is providing help with tough cases. We need our own vertical network in order to effectively pursue solutions from the vertical network of government authority. As the following table illustrates, different types of cases require different levels of intervention.
Grievances related to infrastructure and equipment often require more formal advocacy at higher levels and take longer to resolve. The average time of resolution for these cases is 85 days, as compared to 50 days for cases related to provider performance and 57 days for those related to medicines. Improvements to infrastructure and equipment—for example, a separate room for HIV counseling and testing or a shaded seating area with benches for patients—normally require budgetary support, which involves sometimes lengthy bureaucratic processes.
In some cases, health advocates have collaborated closely with facility leadership, health committees, and community members to draft and submit petitions and written requests to district and provincial government, with varying levels of success. In other cases, the program officer has participated in the annual district budget planning exercise to advocate for inclusion of a particular item.
Fewer cases involving provider behavior have required us to go beyond the level of the facility—just 18 out of 844. Among these 18 exceptions are bribery allegations, which often involve numerous providers working in collusion. In those cases, the health facility director is often aware of the problem but is reluctant or unable to intervene effectively, either because of fear of retaliation, limited management capacity, or both. In addition, health workers are often unwilling to harm a colleague’s career by reporting on the colleague’s misbehavior. In these cases, when a remedy is unattainable at the facility level, and because of the sensitivity of the allegations, our program officer and legal adviser help the health advocate and clients to approach district level authorities in the ministry.
In one case involving the suspected bribery of maternity patients, discussions with the health advocate led the district health director to call several community meetings in which he heard patient complaints firsthand. After investigating these claims, the director took formal disciplinary action against one medical technician. He followed up over the next few months, meeting regularly with health facility leadership and health committee members. He introduced a new district-wide policy of publicly posting phone numbers of key personnel—including his own—in an effort to curb the practice of bribery and encourage patients to seek redress for grievances when violations do occur.
Other cases have been less successful. In Maputo, where power is highly centralized, health center directors tend to have less autonomy than in the other areas where we work. At one busy urban facility, there were frequent complaints about delayed initiation of consults: patients typically begin queuing at 6:00 am, as the facility is supposed to open at 7:30, yet at this particular site a handful of providers were regularly arriving to work one to two hours late.
After hearing from the health advocate and committee members, the facility director called an all-staff meeting. In the days that followed, she instituted a new policy by which the head nurse was to monitor an attendance log. A number of health workers gamed this system by signing in and then leaving during the day, only to return to sign out at 3:30 pm. Despite clear evidence that this was taking place, the director did not take any disciplinary action. District leadership has been unresponsive, and the problem persists.
It is difficult to say why some attempts at remedies from ministry authorities succeed while others fail. When presented with specific claims via in-person meetings, formal letters, or petitions, health officials are often prompted to take action. Leadership may be aware of common violations of patients’ rights in the broad sense—for example, that a particular facility has a problem with theft of medicines—but the presentation of concrete evidence demonstrating a breach of policy makes it easier to intervene. In other cases, officials refuse to act.
There are multiple variables at play, including the skill of the advocates and the responsiveness of the particular officials involved. The state is, of course, not a monolithic structure.28 We try to identify champions of patients’ rights within the government and cultivate relationships with them. These allies vary by location and include health center directors, the chief nursing officer at the district level, influential traditional authorities, and provincial directors.
Translating grassroots experience into systemic change
We track data rigorously on every case the advocates take on, and every community-facility dialogue they facilitate. In the aggregate, this information provides invaluable insight into how health policy is working in practice. We draw on this information to propose systemic changes that can affect the entire population, not just those living in catchments where health advocates are active.
We convey recommendations through quarterly reports to government, issue-specific policy briefs, and in-person meetings. A recent brief based on the bribery cases we have handled, for example, explains how to detect when bribery is taking place (common signs to look for) and proposes reforms for curtailment.29 The health ministry distributed 200 copies to hospital directors and incorporated recommendations into its training materials. We are currently collaborating with the ministry to develop a new national strategy on prevention of bribery in the health sector.
In 2015, the Ministry of Health asked Namati to assist in revising its national policy on the “quality and humanization” of health services. Based on our experience, we have proposed new guidelines for grievance redress and national implementation of the health facility assessment process we have used to catalyze dialogue between communities and health facility staff.
Going forward, we aim for clients to take part directly in not just resolving their own cases, but in advocating for systemic change. True legal empowerment means that ordinary people can not only understand and use the law, they can shape it too.
Conclusion
Our preliminary experience suggests that when people are equipped to exercise their rights to health, even a poorly resourced system can improve. We have found value in blending legal empowerment and social accountability practices. The health advocates’ three modes of action––popular education about health policy, regular community-facility dialogues, and a rigorous case-based approach to resolving grievances—interact synergistically.
Heightened awareness leads more people to raise grievances and to participate in the community-facility dialogues. The dialogues uncover system failures and provide a forum for resolving as many problems as possible at the facility level. The case-based approach allows advocates to pursue redress systematically for those problems that aren’t resolved through dialogue. With the help of a vertical team, health advocates and their clients can engage every rung of state authority in pursuit of a solution. For people like Alcina and Jorge, health services transform from something for which they should be grateful, even when the services are dysfunctional, into something in which they can take part.
One might worry that deploying advocates in a small proportion of the country could end up redistributing limited resources to communities that happen to have health advocates—grease for squeaky wheels—rather than improving the system as a whole. We have three thoughts in relation to that concern.
First, we do not believe that the health system is zero-sum. Many improvements are possible within existing resource constraints, and persuading officials to respond in specific instances may increase rather than diminish their responsiveness overall.
Second, even at a small scale, this grassroots experience can create a compelling basis for advocating reforms that affect the entire population. For that reason, it’s important to deploy advocates in multiple provinces or regions––even before serving the entirety of any province––so that the data can tell a nationally representative story.
Third, these efforts should not stay small scale. We estimate that advocates could serve the entire country for roughly 1% of the national health budget.30 Even if the money is made available, the prospect of scale poses challenges. Is it possible to maintain dynamism and excellence if the number of defensores grows dramatically? Can the vertical network that supports health advocates—which we have found to be crucial for both quality control and for engaging the full network of state authority––be scaled in proportion to the advocates themselves? These are challenges we are eager to take on.
We are keen to collaborate with other groups pursuing the right to health and to see defensores across many countries collecting a common core set of data on the grievances they address—information on the nature and prevalence of different types of problems and the ways in which those problems are resolved. That information could be a basis for comparative methodological learning on how health advocates can be effective across different social and legal contexts. We can get better at what we do by learning from one another.
This would also create a multinational portrait of how health systems are working, and how they respond to citizen action. A coalition of groups could harness that information to identify and advocate systemic reforms to the practices of international bodies like UNICEF and the Global Fund on AIDS, TB, and Malaria.
We believe that the right to health will not be realized through top-down reforms alone, or even through democratic elections every few years. We the people need to take part daily in the rules and institutions that shape our lives.
Acknowledgments
We would like to express our deep gratitude to the health advocates, village health committees, health providers, and communities whose story this is, for their perseverance in the face of injustice. Huge thanks also to Eric Friedman, Alice Goldenberg, and Akhila Kolisetty for invaluable research assistance; to Marta Schaff and two anonymous peer reviewers for insightful feedback that significantly improved the essay; and to Open Society Foundations (OSF), the UK Department for International Development (DFID), the Skoll Foundation, Centro de Colaboração em Saúde (CCS), Centers for Disease Control and Prevention (CDC Mozambique), the U.S. President’s Emergency Plan for AIDS Relief (through a sub-agreement with CCS), Open Society Initiative for Southern Africa (OSISA), Médicos Sem Fronteiras (MSF) and Oxfam Novib, without whom this work would not be possible.
* The names of all patients and providers have been changed
Ellie Feinglass, MSc, is Director of the Right to Health Program at Namati, Maputo, Mozambique.
Nadja Gomes is a Mozambican human rights lawyer. She is Adjunct Director of Namati Moçambique and Lecturer in the Faculty of Law at Eduardo Mondlane University, Maputo, Mozambique.
Vivek Maru, JD, is Founder and CEO of Namati, Washington, DC.
Please address correspondence to the authors c/o Ellie Feinglass. Email: elliefeinglass@namati.org
Competing interests: None declared.
Copyright: © Feinglass, Gomes, and Maru. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted noncommercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- M. Kruk, G. Yamey, S. Angell, et al. “Transforming global health by improving the science of scale-up,” PLoS Biology 14/3 (2016), p. 2; World Health Organization, Knowledge management strategy (Geneva: WHO, 2005).
- P. Mannava, K. Durrant, J. Fisher, et al., “Attitudes and behaviours of maternal health care providers in interactions with clients: A systematic review,” Globalization and Health, 11/36 (2015), pp. 11-14; Physicians for Human Rights, Ensuring equity: A guide to addressing and eliminating stigma and discrimination in the health sector (Cambridge/Washington, DC: Physicians for Human Rights, 2011), pp. 6-13.
- See, for example, World Bank, “Spotlight on Kerala and Uttar Pradesh” in The world development report: Making services work for poor people (Washington, DC/Oxford: World Bank and Oxford University Press, 2003); J. Dasgupta, “Ten years of negotiating rights around maternal health in Uttar Pradesh, India,” BMC International Health and Human Rights 11/3 (2011), pp. 2-4.
- V. Maru, “Allies unknown: Social accountability and legal empowerment,” Health and Human Rights 12/1 (2010), pp. 83-93.
- See, for example, S. Golub, “Beyond the rule of law orthodoxy: The rule of law alternative,” Rule of Law Series Working Papers No. 41 (Washington, DC: Carnegie Endowment for International Peace (2003), pp. 25-37; Commission on Legal Empowerment of the Poor, Making the law work for everyone (New York: Commission on Legal Empowerment of the Poor and UNDP 2008), vol. I, pp. 1-11; V. Maru, “Between law and society: Paralegals and the provision of primary justice services in Sierra Leone and worldwide,” The Yale Journal of International Law 31 (2006), pp. 465-470.
- M. Bjorkman and J. Svensson, “Power to the people: Evidence from a randomized field experiment on community-based monitoring in Uganda,” Quarterly Journal of Economics 124/2 (2009), pp. 735-769.
- J. Fox, “Social accountability: What does the evidence really say?” World Development 72 (2015), pp. 346-361; J. Fox and B. Halloran (eds) with A. Levy, J. Aceron, and A. van Zyl, Connecting the dots for accountability: Civil society policy monitoring and advocacy strategies (Washington, DC/London: Transparency and Accountability Initiative, American University School of International Service, 2016), pp. 5-6; Dasgupta (see note iii), pp. 2-4.
- Ministério de Saúde (MISAU) Moçambique, Relatório Anual 2015: Relatório Anual das Actividades Relacionados ao HIV/SIDA (Maputo: MISAU, 2016), p. 12.
- UNDP, Human development report: Work for human development 2015 (New York: UNDP, 2015).
- UNICEF, State of the world’s children 2015: Executive summary (New York: UNICEF, 2014), p. 44; World Health Organization, Trends in maternal mortality: 1990 to 2015 (Geneva: WHO, 2015), p. 95; Central Intelligence Agency, The world factbook: Country comparison, maternal mortality rate. Available at https://www.cia.gov/library/publications/the-world-factbook/rankorder/2223rank.html.
- Ministério de Saúde Moçambique (see note viii), p. 12.
- World Health Organization, World health statistics 2015 (Geneva: WHO, 2015), pp. 118, 122. Available at http://who.int/gho/publications/world_health_statistics/EN_WHS2015_Part2.pdf. Regional averages for physicians and nurses are 2.7 and 12.4 per 10,000 inhabitants, respectively.
- Boletim da República, Constituição da República Popular de Moçambique, de 2 de Novembro, I Série, Número 51, Maputo, 2004.
- Open Society Foundations, Mozambique: Justice sector and the rule of law (Johannesburg: Open Society Institute for Southern Africa, 2006), pp. 15, 125.
- Boletim da República. Lei da Protecção da Pessoa, do trabalhador e do candidato a emprego vivendo com HIV e SIDA, no 19/2014, de 27 de Agosto, I Série, Número 69, Maputo, 2014.
- A. Biza, Mozambique Right to Health Program Baseline Assessment Report (Maputo: Namati, 2013).
- D.H. Peters, T. Adam, O. Alonge, et al. “Implementation research: What it is and how to do it,” British Medical Journal 347/f6753 (2013).
- L. Pritchett, S. Samji, and J. Hammer, “It‘s all about MeE: Using structured experiential learning (“e”) to crawl the design space,” Faculty Research Working Paper 322 (Washington, DC: Center for Global Development, 2013).
- G. Mansuri. and V. Rao, Localizing development: Does participation work? (Washington, DC: World Bank, 2013), pp. 12, 287.
- W. Forbath, “Cultural Transformation, Deep Institutional Reform, and ESR Practice: South Africa’s Treatment Action Campaign,” in L. White and J. Perelman (eds), Stones of hope: How African activists reclaim human rights to challenge global poverty (Stanford, CA: Stanford University Press, 2010), p. 52.
- M. Heywood, “South Africa’s Treatment Action Campaign: Combining law and social mobilization to realize the right to health,” Journal of Human Rights Practice 1/1 (2009), pp. 14-36.
- S. Bennett and D. Ssengooba, “Closing the gaps: From science to action in maternal, newborn, and child health in Africa,” PLoS Medicine 7/6 (2010).
- Biza (see endnote 16), p. 26. From our baseline assessment in 2013, one complaints book had not had a new entry in over six years.
- Ministry of Health Mozambique, Guião de referência para o estabelecimento e funcionamento dos comités de saúde, MISAU, Direcção Nacional de Saúde Pública (May 2012).
- See, for example, R. Paterson and M. van Wyk, “Patient’s rights in New Zealand: Complaints resolution and quality improvement,” Medicine and Law Journal 23/1 (2004), p. 35.
- A. George, K. Scott, S. Garimella, et al., “Anchoring contextual analysis in health policy and systems research: A narrative review of contextual factors influencing health committees in low and middle-income countries,” Social Science & Medicine 133 (2015), pp. 159-167.
- A forthcoming book on community paralegal efforts across six countries makes the same conclusion. V. Gauri and V. Maru (eds), Community paralegals and the pursuit of justice: Bringing law to life (forthcoming, Cambridge University Press).
- See, for example, Dasgupta (note iii), p. 9.
- Namati Moçambique, “Recomendações Para Lidar com Casos de Suborno no Sector da Saude.” (2015). Available at https://namati.org/resources/recommendations-for-addressing-bribery-in-the-health-sector/
- This is a rough estimate based on the unit costs for our current effort. It assumes expansion to every province, with strategic selection of districts and health facilities. We anticipate that the vertical support we provide now would stay roughly proportional as the number of advocates grows. The national health budget is approximately $1 billion USD.