Volume 24/1, June 2022, pp. 189-202 | PDF
Michael J. Cole
Abstract
Globally, there are not enough services to meet the enormous demand for evidence-based community-based drug treatment. Further, the effectiveness of available services varies as much as the diversity of their treatment regimens. Capacity-building can help increase the scale and improve the quality of those interventions. Maximizing the impact of capacity-building requires a comprehensive and systematic approach considering three levels—the individual worker, organization, and service sector—and it starts with assessment and planning. This paper describes the areas to consider and steps to follow when planning and implementing a comprehensive capacity-building approach in community-based drug treatment services. Utilizing an empowerment model for capacity-building can increase the stakeholders and resources engaged in the process. Better engagement with community stakeholders increases the likelihood that capacity-building outcomes will be sustainable. Further, the institutionalization of capacity-building can establish and promote an organizational culture of continuous learning.
Introduction
Global expenditure on drug law enforcement is well over US$100 billion annually.1 Despite this, the number of people who use illicit drugs continues to grow. In 2019, approximately 275 million people, or 5.5% of the world’s population (15–64 years of age), had used illicit drugs in the previous year.2 In the same year, approximately half a million people died from drug use, mainly from overdoses and liver disease.3 It was also estimated that just over 12%, or approximately 36.3 million, of those who had used illicit drugs in 2019 may experience drug use disorders for which they may need treatment.4 Treatment can dramatically reduce the costs associated with problematic drug use. For example, US estimates indicate that every US$1 invested in treatment for drug use results in a savings of US$12 in costs associated with health care, drug-related crime, and criminal justice.5 A significant obstacle to people who use drugs achieving positive health outcomes is the insufficient availability of community-based services to meet demand. According to the United Nations Office on Drugs and Crime (UNODC), only one in six people with a drug use disorder received treatment during 2016, and this fraction has remained relatively constant.6
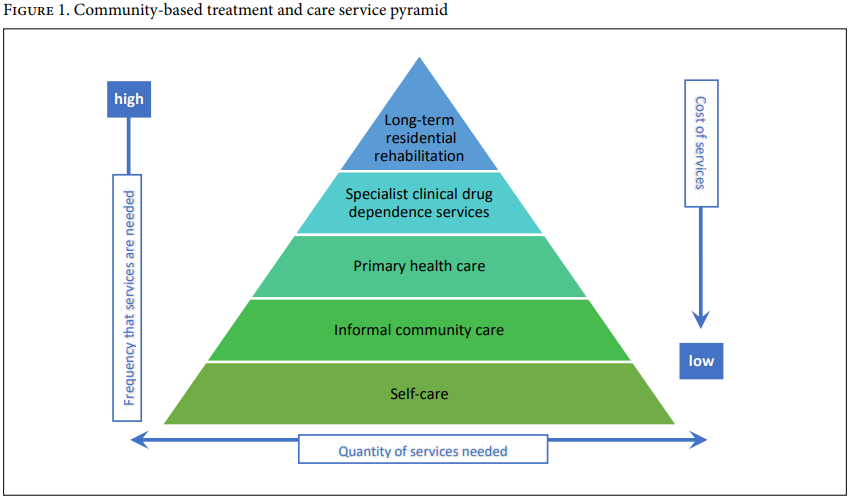
Community-based treatment and care (CBTC) services for people who use drugs are informed by the World Health Organization (WHO) and UNODC international treatment standards for drug use disorders and by UNODC principles and guidance.7 The CBTC model is based on evidence showing that approximately 90% of people who use drugs do not develop problematic or dependent drug use.8 Of those who do, most can be supported by informal services (self-care and community care) without entering a residential treatment setting. These informal services are the cheapest to fund and deliver. A much smaller number of people with severe dependence or complex needs may need a residential setting (e.g., clinical service or hospital) with specialist staff. This is the most expensive way to provide services.9 Integrated within existing health care systems, CBTC provides the opportunity for each client to choose the least restrictive and most appropriate type of service.
The CBTC service pyramid in Figure 1 shows that most people who have problematic drug use resolve it themselves with the support of friends and family or informal community services. Specialist longer-term residential services are needed for only a small percentage of people with severe dependence and complex needs.10
Despite advocacy for CBTC by entities such as WHO, UNODC, Human Rights Watch, and national civil society organizations, many countries still favor punitive compulsory drug detention centers rather than voluntary community-based therapeutic services. People who use drugs are incarcerated in compulsory centers long term, from several months to a few years. Compulsory drug detention centers are not evidence based, have high relapse rates, and frequently involve abuse, corporal punishment, and torture.11 It should not need to be stated that vulnerable people with treatable health conditions should not be subjected to cruel, inhuman, or degrading actions. Treating a client with care, respect, and dignity is essential to achieving therapeutic outcomes. It is also cost-effective. For example, research comparing compulsory drug detention centers and community-based voluntary methadone maintenance treatment in Vietnam confirmed that community-based treatment is less expensive and more effective than compulsory centers in achieving drug-free days among heroin-dependent individuals.12
Unfortunately, globally CBTC services are trying and failing to meet an enormous unmet need. The World Drug Report 2021 estimates that of the 275 million people aged 15–64 who used drugs in the previous 12 months, about 13%, or 36.3 million, suffer from drug use disorders requiring treatment.13 Yet evidence-based drug treatment services in most countries are relatively new fields compared with other health and social services. As a result, they are frequently underdeveloped and under-resourced. Even in countries with well-developed and well-resourced health service infrastructure, CBTC services are under-resourced. Before accessing treatment and support, their clients often endure long waiting times, sometimes in desperate circumstances. An Australian study, for example, found that, against international benchmarks, Australia had high rates of treatment utilization and one of the lowest rates of unmet demand in the world.14 Despite this, Australian drug treatment services were meeting only 26%–48% of demand, with residential rehabilitation, residential withdrawal, pharmacotherapies, and counseling most frequently unable to meet demand.15
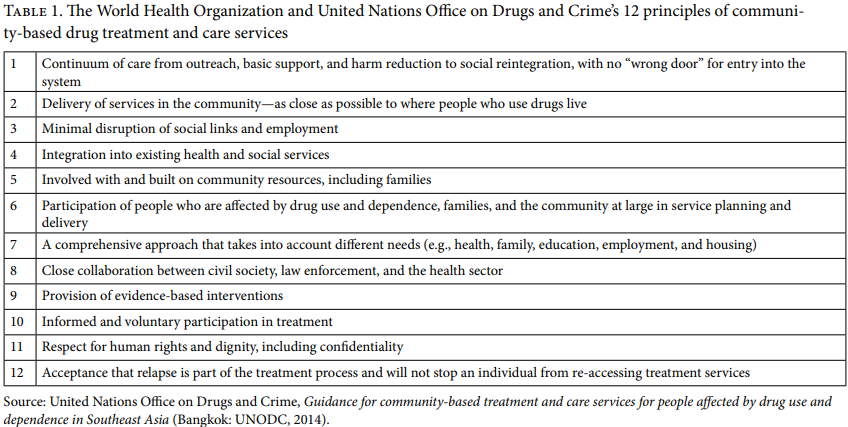
UNODC and WHO have published a set of 12 principles to guide the design and delivery of drug treatment services (see Table 1).16 Each is a core characteristic of the CBTC model and an essential element to consider when strengthening capacity. In addition, depending on the organization’s goals, context, and clientele, other principles may be considered—for example, principles requiring that service provision be culturally appropriate, equity-focused, and client-centered. Good-quality CBTC services are guided by international, national, or professional principles. They are also designed and delivered around their clients’ and communities’ unique contexts and needs.
Capacity gaps in existing services
One reason for the inadequate availability of evidence-based community services for people who use drugs is that there are gaps and shortages in the capacity of existing services and the capability of their workforce. Over the past two decades, the author’s work on capacity-building and program evaluation of such services throughout Asia has identified a growing need for capacity-building to establish and strengthen the CBTC services sector. Many local drug treatment systems across a variety of settings lack sufficient staff with the appropriate type and level of knowledge and skills to establish and maintain community services that achieve reliable, good-quality client outcomes. Furthermore, the establishment of new services and their scale-up are often constrained by difficulties in recruiting enough qualified staff.17
In addition, capacity-building is important to ensure the health and safety of staff working in CBTC services. It can make the difference between staff feeling empowered and capable or becoming despondent and burnt out and leaving the field altogether. Jianhua Li and colleagues found that high rates of staff turnover in drug treatment services were associated with staff feeling underprepared for their role and requesting additional professional development to enhance their competence and ensure their own safety and well-being.18
Capacity-building for expansion and improvement of CBTC services
Capacity-building is frequently misunderstood and often considered to be synonymous with training. However, a focus on training underestimates the contribution capacity-building can make when carefully planned and systematically applied to transforming services and service systems. It also confines the focus of capacity-building to increasing individual competence rather than increasing the capacity of the whole organization. This paper follows a practical working description of capacity-building:
Capacity building in drug use treatment and rehabilitation services is the process of developing and enhancing the knowledge, skills, attitudes, values, strategies, structures, and resources that individuals and organizations require to meet the complex needs of people who use drugs and their communities and to support them in achieving positive bio-psycho-social outcomes.19
The terms capacity, capability, and competence are used interchangeably in the literature, so it is worth describing and distinguishing these concepts to promote greater clarity. An individual’s competency is demonstrated by their ability to apply acquired knowledge and skills, and these can be measured against well-accepted standards required in employment and assessed against evidence in the workplace.20 Capability is having or developing the ability to do something—in other words, it is the skills, knowledge, and attitudes necessary to complete a particular task to a level of competence. Capacity is the amount of time, resources, appropriate personnel available, and supporting structures and processes that enable staff and volunteers to apply their capabilities to achieve their organization’s objectives (e.g., quality of care and optimal client outcomes).
Capacity-building helps create the structures and systems that enable practice skills and knowledge (i.e., capabilities) to be applied. It can also address some of the most immediate barriers to expanding voluntary, evidence-based CBTC services in the community. There is an interplay between the concepts of capacity and capability-building. Building individual competencies (e.g., knowledge, attitudes, and skills) enhances a worker’s capability (e.g., the practice of assessment, counseling, or case management), which they can apply if their organization has the capacity (e.g., the policies, systems, and procedures) to enable them to do so. In many cases, building capability by increasing a team’s knowledge and skills can help expand capacity. This is the idea of working smarter, not harder.
Empowerment through capacity-building
The literature raises the concern that the term capacity-building suggests no preexisting capacity.21 However, the reality is that many countries have been providing various forms of care and treatment for people who use drugs for generations, so capacity-strengthening or enhancing capacity would be a more accurate and fair description. This discussion will assume a base level of specialist or generic capabilities supported by organizational leadership, structures, systems, and resources upon which capacity can be further built or strengthened to achieve improved client outcomes.22
The literature also distinguishes two major capacity-building orientations—the “deficit” model versus the “empowerment” model.23 The deficit model emphasizes an external intervention to diagnose weaknesses or gaps in capacity and fill those gaps. This is contrasted with the empowerment model, where the emphasis is on enabling organizations and their personnel to identify and respond to the problems and opportunities they face. The empowerment model has been particularly emphasized in community development and international development, where significant inequalities of power and resources often exist that can undermine capacity-building processes.24 These two orientations are perhaps best regarded as opposite ends of a spectrum, with many approaches to capacity-building lying somewhere in the middle.25 It is generally held that participatory and collaborative approaches using a combination of external and internal expertise produce more significant sustainable change in capabilities and capacity. The technical input of an external expert can help initiate change. However, to institutionalize and sustain that change and associated reforms requires purposeful efforts to expand and upgrade individual capabilities and organizational capacity.26
However, a more incisive and nuanced examination of the difference in capacity-building development approaches is emerging from research on Indigenous empowerment initiatives that distinguish between technical assistance done to, for, with, or by the intended beneficiaries (see Table 2).27 These are highly relevant to capacity-building efforts in local CBTC services and salient for how people who use drugs are engaged in capacity-building processes.
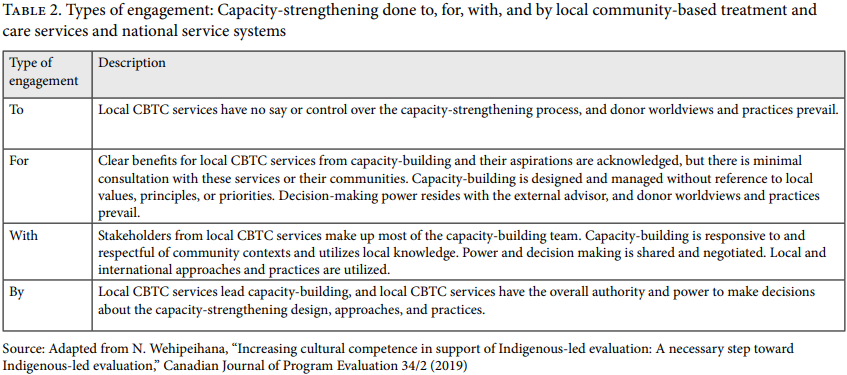
Local services and communities stand to gain or lose far more from a capacity-strengthening approach than an external consultancy team, which usually leaves once the plan is in place and may never see the results of its work. Indeed, the local community must live with those results for better or worse. Therefore, these actors should not be considered passive recipients of technical assistance but active participants in addressing their health and social issues. Harnessing the expertise of local experts, including those with lived experience, is critical. Doing so transforms capacity-strengthening from something done to the national CBTC sector and local services into something done for people who use drugs into processes undertaken by CBTC with key stakeholders, especially people who use drugs. Assessment and planning for capacity-strengthening are unlikely to be effective or sustainable if, for example, they are applied as part of a standard template prescribed by an external or foreign advisor. Local experts are best placed to understand capacity gaps, assets, and the opportunities for strengthening capacity. They understand the factors (political, economic, social, cultural, legislative, and environmental) at play in their national context. They also have the local knowledge, experience, and networks to plan the necessary and pragmatic changes appropriate to their service system and the needs of their CBTC workforce. Finally, when local CBTC services manage the capacity-building knowledge transfer, they make adaptations and generate innovations that contribute to and expand the global knowledge base and can be adopted by either Global North or other Global South actors.
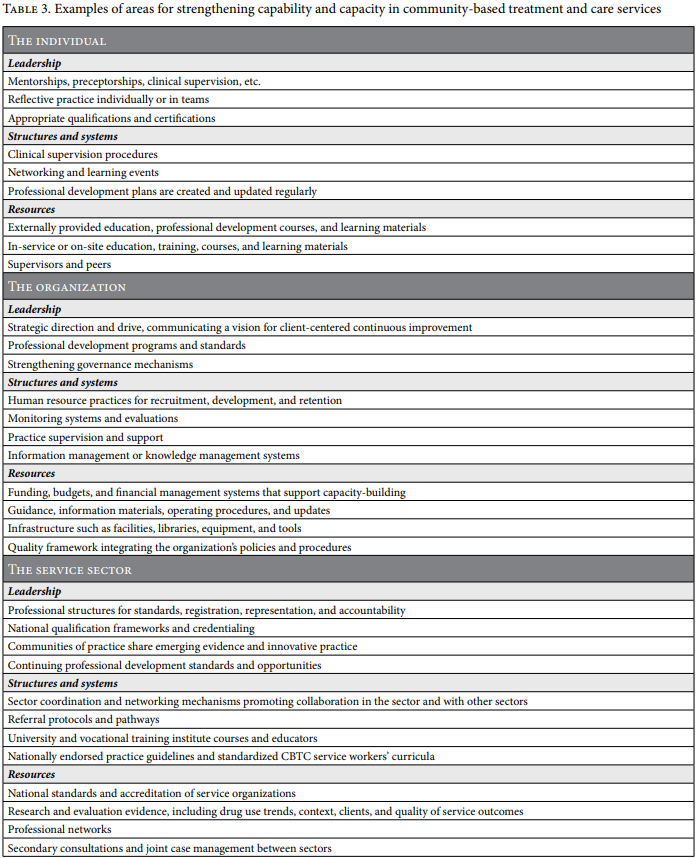
A systematic approach to capacity-building considers development on at least three levels—individual, organization, and service system or sector.
- The individual: The focus here is to equip individuals with the right cognitive tools, knowledge frameworks, and skill sets to perform effectively.
- The organization: The focus here is on the institutionalization of capacity-building and integrating skills and training into the organization’s policies, programs, and processes.
- The service sector: The focus here is on collaboration with and integration of the service system.
These can be described and analyzed as the micro, meso, and macro capacity and capability-building levels. Although the three streams are conceptualized separately here, they are integrated, work synergistically, and may overlap—for example, communities of practice may occur at a sector-wide level with organizational support to improve the skills and knowledge of individual practitioners.28
A systematic approach to capacity-building enables the appropriate sequencing of mutually supportive actions, prioritizing high-need areas for development, and helps maximize outcomes in those areas. It also encourages a longer-term view of building an enduring organizational culture of continuous reflection and improvement in supporting clients in achieving their treatment outcomes. In other words, it promotes the sustainability of those strengthened capacities. WHO notes that capacity-building requires individuals and institutions to have a clear capacity-building mission or strategy and adequate supporting organizational structures and systems.29 It also requires that staff have sufficient autonomy, incentives, and supervision to apply their drug treatment knowledge and skills. A systematic approach to capacity-building begins with a comprehensive assessment that informs the development of a capacity-strengthening plan. If well supported and thoughtfully managed at all levels, this promotes the development of a self-sustainable organizational culture of reflective practice and continuous improvement.
Steps in developing a capacity-building strategy
It is widely recognized that there is no single treatment or program that works for all people who use drugs under all circumstances. Perhaps best expressed by Steve Allsop and Sue Helfgott, “Most interventions are effective under some circumstances, while no single strategy is effective under all circumstances.”30 It is typical rather than exceptional for people to try multiple treatment options (where available) before finding the form of treatment and the treatment provider that works best for them, at that time, and in those specific circumstances.31
Similarly, there is no one-size-fits-all approach to capacity-building. Each organization and its service context are unique, as are its capacity assets and needs at any point in time. Instead, each service or organization can benefit from creating its own unique and fit-for-purpose capacity-building strategy. When planning a capacity-building strategy, we must first define its purpose: What do we want the organization and the staff practice to look like when we have achieved this capacity increase? Part of the answer to this question emerges from the foundations upon which we build—the guiding principles for CBTC service provision, as outlined by WHO and UNODC and listed in Table 1.32
The following framework is presented to assist organizations in planning for capacity- and capability-strengthening to enhance the quality and outcomes of their services, improve the proficiency of their personnel, and reduce burnout and turnover of staff and volunteers.
Step 1: Systemic community-based assessment
While there are various capacity-building approaches, any strategic approach to capacity-building planning should be preceded and informed by an assessment of organizational capacity assets and needs. For example, developing capacity in one area alone may not be effective if there are problems in other areas. The capacity-building assessment must be systemic to diagnose accurately the capacity strengths, gaps, and support needed. Barbara Blumenthal argues that assessment using a skilled consultant is more likely to uncover underlining problems than self-assessment.33 Another critical part of a comprehensive assessment is examining “the internal and external organizational context, power hierarchies, administrative culture, and decision-making processes.”34
Step 2: Planning
To be effective, a capacity-building strategy must be tailored to the organization’s needs, the environment in which it works, and its life cycle.35 A planned and coordinated approach to capacity-building that considers tailored and mutually supportive interventions targeting capacity gaps or needs at each level is more likely to produce better outcomes than single interventions.36 Building capacity is an investment in the long-term success of an organization. A step-by-step process to institutional strengthening and building capabilities is essential due to its dynamic nature. Maintaining flexibility in designing capacity-building projects and associated frameworks enables better adaptation to that dynamism and better enables alignment with changing priorities and emerging trends or needs.
Thomas Backer suggests that while narrowly defined interventions can work, those capacity builders with the most impact offer a range of services such as assessment, technical assistance, financial assistance, and other support.37 First, they need to choose a primary focus for their work.38 It may be general or aimed at strengthening a specific area (e.g., a particular priority topic or client target population) and is likely to prioritize the most significant unmet demand areas. Many of them are easily identifiable and already well known to service providers and their communities. Typical examples may include services for young people, homeless people, women with children, people identifying as LGBTQIA+, and Indigenous people.39 Alternatively, an organization might not want to initially choose the areas of greatest need but those areas with the most potential to improve. Getting a few early wins may help encourage support and alignment with the strategy and attract or justify resources allocated to capacity-building.40 Another consideration is that “capacity can often be increased more effectively by reinforcing existing structures than by building new ones.”41
Capacity-building is likely to be an iterative process, such as a series of phases or stages targeting prioritized areas or levels of capacity.42 The flexibility of a staged or iterative approach can be necessary because, for example, the allocation of time and scarce resources must be prioritized. The acquisition of new practice skills may require sequential scaffolded learning approaches. Work in one area often exposes limitations in another. Additionally, some capacity-building outcomes are preconditions for others. For example, establishing a national professional credentialing system and registration may precede the requirements for continuing professional education and the delivery of professional development programs.
Step 3: Research, evaluation, and monitoring
Increasing the overall volume of CBTC services provided is essential, but equally important is increasing the quality of those services. Monitoring and evaluation can help assess and improve the effective and efficient achievement of clients’ outcomes. However, capacity-building is often vaguely defined in the literature, and descriptions lack precision. Without precision, it is difficult to measure or evaluate progress in achieving capacity-strengthening objectives.43 Monitoring and evaluating any capacity-strengthening efforts requires a detailed plan that explicitly defines the intended outcomes. This will, in turn, support better decision-making, improve the allocation of resources, improve the understanding of capacity strengths and challenges, and promote organizational learning.
Research and evaluation are essential for generating, testing, and continually improving the evidence base of policies, programs, procedures, and practices. These activities require the specialist skills of researchers and evaluators. However, to be well informed and to be of actual practical benefit, evaluation and research must engage CBTC practitioners, the communities in which services are based and into which clients will return, and, most importantly, those with lived experience (i.e., people who use drugs). Working collaboratively with people who use drugs, their families, and communities helps interpret evidence and synthesize lessons learned through the lens of lived experience, which promotes practical responses to immediate capacity issues. Leonora Angeles and Penny Gurstein call this “the inclusion of innate wisdom and knowledge of those affected in decision making.”44 They advise this can result in more manageable processes that are less reliant on external tools and technologies, cheaper, and more likely to be sustained.
Table 3 summarizes common areas for strengthening capability- and capacity-building. This list is intended to be illustrative, not exhaustive. There is overlap between levels; for example, the sector might fund an organization to promote education and training in which individuals strengthen their practice skills. For ease of reference, items have been classified under leadership; structures and systems; and resources. However, many could be listed under more than one; for example, professional bodies that establish standards, registration, and accountability may be considered structures that provide leadership.
These are not prescribed steps but examples to consider, and while each capacity-building strategy is unique, any strategy should place the client at its center and work outward. For example, one planning technique could be to answer a series of questions such as the following:
- What outcomes does the client want to achieve?
- What do our staff and volunteers need to be able to do to help clients achieve those outcomes?
- How can our organization support its staff and volunteers in that work?
- How can our organization better engage with our sector and other sectors to support our staff and volunteers’ work and assist our clients in achieving their outcomes?
Individual capacity-building
Any individual capability plan is more likely to be effective and lasting if based on an assessment to identify areas in which staff require additional professional development. This assessment is incorporated into a formal plan, such as professional development plans, created and updated regularly for all staff and volunteers. These plans can include internal and external education opportunities, qualification and certification planning, development milestones, career trajectories, and structured opportunities for reflective practice.
While education and training are not the only (or necessarily most critical) tactics in a capacity-building strategy, they can be indispensable, for example, in establishing foundational knowledge, attitudes, and values. In addition, education and training initiatives need to be sophisticated enough to target the desired outcome level—that is, the content, structure, and delivery determined by whether they are designed to raise awareness, increase practice knowledge, increase skills development, influence attitudes and beliefs, or change behaviors.45
Internal learning opportunities may include various forms of formal in-service training. These can be more effective and enduring if supported with experiential learning opportunities, including supervised, structured programs such as probationary placements, internships, preceptorships, and mentoring programs. Specialist CBTC sector knowledge and skills must be learned and practiced in a combination of experiential learning and formal training.46 Combined approaches like these allow for scaffolded learning in which each learning approach supports the understanding, application, and extension of the knowledge frameworks and skills learned earlier.47 Those opportunities must match the person’s current skills and occur in an environment that encourages taking risks and is challenging without being overwhelming.48
Learning knowledge frameworks and skills is facilitated through reflective practice and by “reflective practitioners who are able and willing to challenge continuously their own assumptions and the assumptions of their colleagues in a constructive way which generates new insights and leads to the development of explicit wisdom.”49 Self-reflection and reflective practice can be further facilitated in clinical supervision, mentoring relationships, team reviews, or communities of practice.50 Building capacity not only entails learning technical concepts and processes but also, if it is to be self-sustaining, requires learning soft skills. For example, while harnessing scientific evidence to guide good practice is crucial, it is equally important to use critical thinking and practical experience to ensure that evidence is applied appropriately and adapted to the service context and individuals’ needs. Standard practice guidelines can be a helpful point of reference for ensuring consistent quality outcomes. Even so, if used mechanically without interpretation and adaptation to contexts and needs, they may be ineffective or even harmful.51
Access to external education, seminars, conferences, and webinars is also valuable because it creates open information exchange systems and exposes personnel to emerging trends, innovative practices, and new knowledge from the evolving scientific evidence base. External events can also promote a sense of professional identity: formally, when they involve consultation and development of professional standards and guidance, as well as qualification and certification frameworks, or more informally, with opportunities for expanding professional networks, advocacy, and peer support.
Organizational capacity-building
Leadership is essential to strengthening organizational capacity. The support of CEOs, managers, and other key decision-makers helps in developing and sustaining organizational capacity because it provides strategic direction and drive and communicates a vision for client-centered continuous improvement.52 Leaders who are well informed about the context and needs of people who use drugs make better advocates for policy change, service design, and resource allocation. They also offer guidance and encouragement, support the development of staff and volunteers, and steward institutional change for a sustainable organizational culture. Therefore, CBTC service strengthening must invest in developing organizational leaders, ensuring that they are well informed about what constitutes current good practices in service delivery and achieving client outcomes.
An organization’s systems and staffing structures mediate its members’ ability to interact, collaborate, and communicate.53 Joanne Sobeck and Elizabeth Agius suggest that building peer support networks for sharing information and mentoring can also greatly enhance the effectiveness of capacity-building interventions.54 To strengthen their capacity, organizations need to establish, maintain, and improve their supporting structures and systems. Effective governance structures, for example, provide direction, guidance, and accountability for immediate and long-term capacity-strengthening activities. They are independent, hold the leadership team accountable for meeting strategic and operational objectives, and have clearly defined succession plans.55
Organizational policies are vital because they guide why, when, and how procedures and practices are carried out within the specific organizational, cultural, and political context. In this way, evidence-based policies serve as mechanisms to institutionalize good practice in CBTC services and help build genuine learning organizations.56 Each CBTC organization’s systems will vary in type and form, but key elements include the following:57
- quality frameworks integrated across the organization’s policies and procedures
- information or knowledge management systems
- human resource practices for recruiting and retaining capable committed staff and volunteers
- monitoring and evaluation systems to track progress toward client outcomes and organizational objectives
A systematic and comprehensive capacity-building strategy requires resources. Specifically, it requires dedicated funding, an endorsed budget, and sound financial management systems. Therefore, the ability to raise funds in a structured and targeted manner and maintain relationships with potential funders is important for supporting capacity-building programs and achieving sustainable impact at scale. It can be challenging to make a case for capacity-building funding in services that a government considers low priority or for politically unpopular people. However, the case can be strengthened by using robust evidence. This is another critical reason to strengthen systems to monitor, evaluate, and report service outcomes and to promote research demonstrating the benefits of good treatment practices.
Service sector
Improving care systems within and between the treatment sectors relies on sector workforce development, sector-wide data collection systems, and strengthening service connections and networks within the CBTC sector. This includes broader initiatives such as national accreditation of service organizations, national qualification frameworks and credentialing, CBTC curricula by universities and vocational training institutes, and research to generate evidence about client needs and effective interventions.
Cooperation and collaboration among CBTC services can maximize opportunities for practice learning, promote consistent and reliable high-quality service delivery, and shape that service delivery with an understanding of what constitutes good practice.58 In addition, coordination across sectors is crucial for the CBTC sector because it interacts with many other service systems (e.g., primary health care, mental health, vocational, and justice service sectors). Effective and efficient sector coordination and networking can improve treatment and care provision, help ensure the consistent and reliable delivery of high-quality services, and facilitate seamless referrals within and between service sectors.
Developing an organizational capacity-building culture
Organizational change influences organizational culture, and organizational culture can facilitate or hinder organizational change. A comprehensive long-term capacity-building strategy should consider the intended impact of its activities on the organization’s culture. Organizational culture comprises an enduring system of traditions, values, attitudes, rules, norms, and symbols upon which members agree is the basis for their actions—in other words, consensual notions of how things are done around here.59 The culture of a learning organization “must encourage questioning of organizational processes and experimenting with new approaches” and include simple, practical steps such as the institutionalization of routine professional learning and reflective practice.60
Evelyn Pitre and Henry Sims state, “The essence of cultural change is the replacement of one consensual pattern with another.”61 They highlight that leadership is of prime importance in strengthening or changing an organization’s culture. The leader’s vision (i.e., their ability to formulate, articulate, and share new ways of thinking or presenting innovative knowledge frameworks) drives the organization toward its objectives. Susan Labin and colleagues advise that the factors that influence the extent to which an organizational learning culture will become sustainable (adapted here to capacity-building of CBTC) are (1) the strength of CBTC services leadership support, governance, and oversight of capacity-building; (2) the resources available for strengthening capacity-building in CBTC services (staff, time, and financial); (3) the amount and type of internal capacity-building expertise applied to workplace learning and practice improvement; and (4) the degree of capacity-building mainstreaming in CBTC services—that is, how widely capacity-building is considered a routine part of organizational policies, procedures, and practices.62
Strengthening and shaping the organizational culture can also contribute to sector-wide capacity more broadly. Particularly when an organization is well networked, diffusion of knowledge and practices occurs through interactions with other services, civil society organizations, and sector peak bodies.
Conclusion
Globally, the capacity of available CBTC services is not even close to meeting the enormous demand for such services. The effectiveness of all currently available drug treatment services varies as much as the plethora of treatment approaches offered. Governments, regulatory bodies, and service managers urgently need to apply the available scientific evidence on what works, for whom, and under which circumstances to all drug treatment services and in ways that treat clients with care, dignity, and respect. The CBTC model developed and promoted by WHO and UNODC is underpinned by such principles. Capacity-building can help increase the scale of those interventions and improve their quality. At the level of the organization and the individual worker, capacity-building can help increase the quantity and quality of treatment episodes delivered and client outcomes achieved through CBTC services. A comprehensive and systematic approach should be taken to maximize the return on investment of capacity-building. Taking a longer-term strategic approach to developing organizational and individual capacity enables the growth of a sustainable organizational learning culture. This paper has described one way to plan and implement such an endeavor. Governments and donors should seriously consider investing in the capacity-building of CBTC. One component of this investment should come from diverting funding from compulsory detention centers and promoting CBTC as an alternative.
Michael J. Cole, PhD, MEval, is assistant director of evaluation and research at the Australian Department of Social Services, Canberra, Australia.
Please address correspondence to the author. Email: michaeljcole@y7mail.com.
Competing interests: None declared.
Copyright © 2022 Cole. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted non-commercial use, distribution, and reproduction.
References
- Count the Costs, The war on drugs: Wasting billions and undermining economies (Bristol: Count the Costs, 2013).
- United Nations Office on Drugs and Crime, World drug report 2021: Booklet 2; Global overview of drug demand and drug supply (Vienna: UNODC, 2021).
- United Nations Office on Drugs and Crime, World drug report 2021: Booklet 1; Executive summary (Vienna: UNODC, 2021).
- Ibid.
- United Nations Office on Drugs and Crime, Investing in drug abuse treatment: A discussion paper for policymakers (Vienna: UNODC, 2003).
- United Nations Office on Drugs and Crime, Booklet 2 (2021, see note 2).
- World Health Organization, International standards for the treatment of drug use disorders: Revised edition incorporating results of field-testing (Geneva: WHO, 2020); United Nations Office on Drugs and Crime, Guidance for community-based treatment and care services for people affected by drug use and dependence in Southeast Asia (Bangkok: UNODC, 2014).
- United Nations Office on Drugs and Crime, Booklet 1 (2021, see note 3).
- United Nations Office on Drugs and Crime, Trainers’ manual: Community-based services for people who use drugs in Southeast Asia; Module 2; The community-based drug treatment and care approach (Bangkok: UNODC, 2015).
- United Nations Office on Drugs and Crime (2014, see note 7).
- A. Kamarulzaman and J. L. McBrayer, “Compulsory drug detention centers in East and Southeast Asia,” International Journal of Drug Policy 26 (2015), pp. S33–S37.
- T. Vuong, M. Shanahan, N. Nguyen, et al., “Cost-effectiveness of center-based compulsory rehabilitation compared to community-based voluntary methadone maintenance treatment in Hai Phong City, Vietnam,” Drug and Alcohol Dependence 168 (2016), pp. 147–155.
- United Nations Office on Drugs and Crime , Booklet 2 (2021, see note 2).
- A. Ritter, L. Berends, J. Chalmers, et al., New horizons: The review of alcohol and other drug treatment services in Australia (Sydney: Drug Policy Modelling Program, National Drug and Alcohol Research Centre, 2014), p. 191.
- Ibid.
- United Nations Office on Drugs and Crime (2014, see note 7).
- J. Li, C. Wang, J. McGoogan, et al., “Human resource development and capacity-building during China’s rapid scale-up of methadone maintenance treatment services,” Bulletin of the World Health Organization 91 (2013), pp. 130–135.
- Ibid.
- S. J. Allsop, and S. Helfgott, “Whither the drug specialist? The workforce development needs of drug specialist staff and agencies,” Drug and Alcohol Review 21/3 (2002), pp. 215–222; J. F. Ohiorhenuan and S. M. Wunker, Capacity building requirements for global environmental protection (Washington, DC: Global Environment Facility, 1995); Ritter et al. (see note 14).
- M. Wahba, Competence standards for technical and vocational education and training TVET 28/11 (2013).
- S. N. Labin, J. L. Duffy, D. C. Meyers, et al., “A research synthesis of the evaluation capacity building literature,” American Journal of Evaluation 33/3 (2012), pp. 307–338.
- P. Samuel and World Health Organization, Capacity building for health sector reform, WHO/SHS/NHP/95.8 (1995).
- J. Harrow, “‘Capacity building’ as a public management goal-myth, magic or the main chance?,” Public Management Review 3/2 (2001), pp. 209–230.
- A. Noya and E. Clarence, Community capacity building: Fostering economic and social resilience (Paris: Organisation for Economic Co-operation and Development, 2009), pp. 26–27.
- C. Cornforth and J. Mordaunt, “Organisational capacity building: Understanding the dilemmas for foundations of intervening in small-and medium-size charities,” Voluntas: International Journal of Voluntary and Nonprofit Organizations 22/3 (2011), pp. 428–449.
- Samuel and World Health Organization (see note 22).
- N. Wehipeihana, “Increasing cultural competence in support of Indigenous-led evaluation: A necessary step toward Indigenous-led evaluation,” Canadian Journal of Program Evaluation 34/2 (2019).
- Samuel and World Health Organization (see note 22).
- Ibid.
- Allsop and Helfgott (see note 19), p. 218.
- Allsop and Helfgott (see note 19); Ritter et al. (see note 14).
- United Nations Office on Drugs and Crime (2014, see note 3).
- B. Blumenthal, Investing in capacity building: A guide to high-impact approaches (New York: Foundation Center, 2003); Cornforth and Mordaunt (see note 25).
- B. Volkov and J. A. King, A checklist for building organizational evaluation capacity (2007), p. 1.
- Blumenthal (see note 33).
- Cornforth and Mordaunt (see note 25).
- T. E. Backer, Strengthening nonprofits: Capacity-building and philanthropy (Encino: Human Interaction Research Institute, 2000); Cornforth and Mordaunt (see note 25).
- Blumenthal (see note 33).
- Ritter et al. (see note 14).
- Blumenthal (see note 33).
- J. A. Trostle, J. U. Sommerfeld, and J. L. Simon, “Strengthening human resource capacity in developing countries: Who are the actors? What are their actions?,” in M. S. Grindle (ed), Getting good government: Capacity building in the public sectors of developing countries (Boston: Harvard University Press, 1997), p. 63.
- C. Potter and R. Brough, “Systemic capacity building: A hierarchy of needs,” Health Policy and Planning 19/5 (2004), pp. 336–345.
- Harrow (see note 23).
- L. Angeles and P. Gurstein. “Planning for participatory capacity development: The challenges of participation and North-South partnership in capacity building projects,” Canadian Journal of Development Studies 21/Suppl 1 (2000), p. 34.
- A. Aljawharah and C. Callinan, “The Kirkpatrick model for training evaluation: Bibliometric analysis after 60 years (1959–2020),” Industrial and Commercial Training 54/1 (2022).
- J. Sobeck and E. Agius, “Organizational capacity building: Addressing a research and practice gap,” Evaluation and Program Planning 30/3 (2007), pp. 237–246.
- Labin et al. (see note 21).
- J. Spouse, “Scaffolding student learning in clinical practice,” Nurse Education Today 18/4 (1998), pp. 259–266.
- B. Britton, “The learning NGO,” INTRAC occasional paper series, no. 17 (1998), p. 5.
- D. Ballantyne, “Pathways less traveled to value creation: Interaction, dialogue and knowledge generation,” Journal of Business and Industrial Marketing 19/2 (2004).
- Allsop and Helfgott (see note 19).
- Dasra, Ready, set, grow: Effective capacity building for NGOs and funders who dream big. (Mumbai: Dasra, 2019).
- H. Preskill and R. T. Torres, “The learning dimension of evaluation use,” New Directions for Evaluation 88 (2000), pp. 25–37.
- Sobeck and Agius (see note 46).
- Dasra (see note 52), p. 12.
- L. Peirson, D. Ciliska, M. Dobbins, et al., “Building capacity for evidence informed decision making in public health: a case study of organizational change,” BMC Public Health 12/1 (2012), pp. 1–13.
- Ibid.; Ritter et al. (see note 14).
- E. Pitre and H. P. Sims Jr., “The thinking organization: How patterns of thought determine organizational culture,” National Productivity Review 6/4 (1987), pp. 340–347.
- I. Bourgeois and J. B. Cousins, “Understanding dimensions of organizational evaluation capacity,” American Journal of Evaluation 34/3 (2013), pp. 299–319; Preskill and Torres (see note 55).
- Bourgeois and Cousins (see note 59), p. 301.
- Pitre and Sims (see note 58), p. 345.
- Labin et al. (see note 21).
