Case Study of an Aboriginal Community-Controlled Health Service in Australia: Universal, Rights-Based, Publicly Funded Comprehensive Primary Health Care in Action
Toby Freeman, Fran Baum, Angela Lawless, Ronald Labonté, David Sanders, John Boffa, Tahnia Edwards, and Sara Javanparast
Abstract
Universal health coverage provides a framework to achieve health services coverage but does not articulate the model of care desired. Comprehensive primary health care includes promotive, preventive, curative, and rehabilitative interventions and health equity and health as a human right as central goals. In Australia, Aboriginal community-controlled health services have pioneered comprehensive primary health care since their inception in the early 1970s. Our five-year project on comprehensive primary health care in Australia partnered with six services, including one Aboriginal community-controlled health service, the Central Australian Aboriginal Congress. Our findings revealed more impressive outcomes in several areas—multidisciplinary work, community participation, cultural respect and accessibility strategies, preventive and promotive work, and advocacy and intersectoral collaboration on social determinants of health—at the Aboriginal community-controlled health service compared to the other participating South Australian services (state-managed and nongovernmental ones). Because of these strengths, the Central Australian Aboriginal Congress’s community-controlled model of comprehensive primary health care deserves attention as a promising form of implementation of universal health coverage by articulating a model of care based on health as a human right that pursues the goal of health equity.
Introduction
Universal health coverage (UHC) is “access to key promotive, preventive, curative and rehabilitative health interventions for all at an affordable cost.”1 UHC is seen as critical to the health and well-being of populations, and a contributor to reducing poverty.2 Achieving UHC is one of the Sustainable Development Goals in the 2030 Agenda for Sustainable Development.3 However, UHC is but one part of the conception of health as a human right, which also strives for equity in the social determinants of health and in health outcomes.4 Depending on how UHC is pursued, it can either support health as a human right or undermine it.5 There is a risk that a focus on UHC could emphasize access to health care over other measures to equitably improve health—for example, the remainder of measures needed to realize health as a human right.6 There is also debate over whether UHC should strive for universal health care, which would require realized access to health services, or universal health coverage, which focuses on the necessary, but not sufficient, affordability element of access.7
The definition of UHC leaves open to interpretation exactly what model would realize equitable access.7 In addition, UHC focuses predominantly on access to primary medical care and does not distinguish between modes of financing or delivery (e.g., whether publicly or privately financed), which could lead to profit-taking by private insurers or providers, representing opportunity costs to UHC systems.8
In the 1978 Alma-Ata Declaration, the World Health Organization detailed a comprehensive approach to health system development.9 The declaration calls for the integration of promotive, preventive, curative, and rehabilitative activities; a holistic and rights-based approach to health; community participation in health care; universal accessibility; and intersectoral action on the social determinants of health. This was swiftly challenged by a selective, technical approach to primary health care (PHC) targeting the prevention of key diseases.10 As a result of this resistance, and despite the World Health Organization’s renewed call for a more comprehensive PHC vision, comprehensive PHC implementation internationally has been patchy, with few strong national programs.11 Ronald Labonté et al. argue that with the focus in international dialogue shifting to issues of financing and UHC, articulating the necessity of comprehensive PHC is as important as ever.12 While not explicitly named, strong PHC is essential to achieving many of the Sustainable Development Goals.13 A publicly funded comprehensive PHC approach to UHC would promote health, prevent ill health, allow affordable curative and rehabilitative interventions, and emphasize health as a human right.
In Australia, Medicare is the primary vehicle for UHC. Introduced in 1975 (as Medibank) by the Labor government of the time, Medicare allows citizens and permanent residents to access primary medical care through fee-for-service private general practitioners for little or no cost. Medicare includes preventive medicine (within a biomedical framework), but little that could be classified as promotive services. General practitioners are free to charge a higher fee than Medicare will reimburse, in which case the patient pays out of pocket for any fee gap. The pharmaceutical benefits scheme also subsidizes medications, improving affordability. As in other countries, recent austerity and negative perceptions of health care costs have brought UHC under threat.14 Since 2013, the conservative government has sought to increase primary medical care user fees and public health care costs, and remove subsidies from services such as pathology, threatening the affordability and accessibility of PHC. Fear of the government privatizing Medicare was a key theme in the 2016 election, which was seen to contribute to the government’s greatly reduced majority and highlights Australian public support for the universality of Medicare.15
In Australia, in 2011 there were 669,900 Aboriginal and Torres Strait Islander people, comprising 3% of the population.16 In the Northern Territory, where this case study is situated, the proportion is much higher, at 30%.16 Aboriginal and Torres Strait Islander people are more likely to live outside major city areas (65% versus 29% of non-Indigenous people), with 44% living in regional areas and over 20% living in remote or very remote areas.16
Australia lags behind other colonial nations in achieving Indigenous health equity.17 Aboriginal and Torres Strait Islander peoples experience inequities in health (with a life expectancy 10.6 and 9.5 years lower than non-Indigenous males and females, respectively), and in social determinants, including employment (65% employment versus 79% for non-Indigenous Australians), income (2.5 times more likely to be in the lowest income bracket), and increased rates of incarceration (comprising over 25% of prisoners).18 Racism and other intersecting forms of discrimination continue to be reported in health services, with up to 42% of Aboriginal and Torres Strait Islander peoples reporting racism in health services.19 Regular experience of racism in other daily life also has significant detrimental effects on health.19
Aboriginal community-controlled health services pioneered comprehensive PHC in Australia, predating WHO’s Alma-Ata Declaration. First established in the 1970s as a response to poor access to services and discriminatory practices in mainstream health care, these services present a radically different model of primary care to Medicare-financed general practice.20 The first Aboriginal community-controlled health services, including the Central Australian Aboriginal Congress (hereinafter referred to as Congress), were established as a result of public meetings of local Aboriginal people seeking collective advocacy and action to support their rights, including their right to health. In 2016, over 150 Aboriginal community-controlled health services served between a third to a half of the Aboriginal and Torres Strait Islander population.21 In current-day Australia, where the self-determination-centered policies of the 1980s and early 1990s have been replaced by an approach characterized by paternalistic interventionism and a deficit model of Aboriginal and Torres Strait Islander health and well-being, Aboriginal community-controlled organizations play a vital role in providing voice and control to local Aboriginal and Torres Strait Islander communities.22 If UHC is to be pursued in a way that embraces health as a human right, particularly in the context of Indigenous peoples’ rights, then Aboriginal community-controlled organizations provide an illuminating case study of one way to achieve its vision.23
This study is a reflection on findings from a five-year research project on the implementation of comprehensive PHC that partnered with six PHC services: five in South Australia and one Aboriginal community-controlled organization in the Northern Territory, the Central Australian Aboriginal Congress Aboriginal Corporation. Three of the South Australian sites (anonymized as Services, A, C, and E) were longstanding services which arose from a national Community Health Program in 1973 that established community health centers led by community boards and that provided comprehensive social health services; medical services, meanwhile, were largely provided in parallel by private general practitioners. The program was discontinued after three years, but in South Australia and some other states, the services were maintained with state funding. The two remaining South Australian services were an Aboriginal health team (Service D) and a nongovernmental sexual health organization, Shine SA. While we found that the South Australian services moved away from implementation of the comprehensive PHC vision, we found that Congress maintained a comprehensive view of health as a human right, potentially providing a strong basis for UHC.24 In this paper, we explore two questions: What were the strengths of the Aboriginal community-controlled service as a comprehensive PHC model for UHC compared to state-funded and state-managed PHC services? And what threats did the Aboriginal community-controlled service face in achieving a comprehensive PHC model for UHC?
Method
The six PHC services were selected to maximize diversity and because of their existing relationships with the research team that would make participation in a five-year research (2009–2014) project feasible. All services strove to be universally accessible (with the Aboriginal services striving to reach the full local Aboriginal and Torres Strait Islander population) and affordable (only the nongovernmental organization charged fees, and these were minimal and negotiable). However, in reality, the South Australian services were mostly small in scale and residual (available only to those unable to afford private services); they provided timely care only to those individuals and families who qualified as disadvantaged, and their care generally centered only on physical chronic diseases. Congress placed no access criteria on its target Aboriginal population.
For each service, we developed a program logic model in conjunction with service staff to capture in a diagram how the service worked, its suite of activities, its intended outcomes, and the influence of contextual factors.25 At Congress, we did this through two iterative workshops with senior staff and board members in March and August 2010. We employed a range of evaluation methods to measure the services’ performance against the service qualities and outcomes in the logic models, including the following:
- Two rounds of staff interviews: one in 2009–2010 with 68 employees, managers, and regional and central health executives, including 14 interviews with Congress staff and board members,13 and one in 2013–2014 with 63 employees, managers, and executives, including 15 interviews with Congress staff and board members.26 The first round explored the services’ implementation of comprehensive PHC principles, while the second round focused on how this had changed in the intervening four years.
- An online survey of 130 service employees in 2012–2013, including 59 responses from Congress covering the implementation of comprehensive PHC principles in its work.27 This survey aimed for breadth to complement the depth of the interviews.
- Workshops at each service with community members, including three workshops at Congress with a total of 13 community members.28 Community members were asked to rate the services’ achievement of nine different PHC service qualities and to provide reasons for those ratings.
- For each service, a case study of intersectoral action on a social determinant of health.29 For Congress, its contribution to collaborative advocacy work on alcohol supply restrictions in Alice Springs was documented through the collection of reports and media releases, and interviews with two Congress employees, three employees from partner organizations, and one community member.
Each service provided six monthly reports on changes in service provision, partnerships, budgets, staffing, and other relevant factors for the duration of the project.
Congress board members and senior executive staff were informed of each stage of research, and the board approved Congress’s participation in the project. Two Congress staff members served as associate investigators for the grant proposal, on which they provided input. Ethical approval for each research stage was received from the relevant Flinders University and South Australian Health research ethics committees, as well as the Aboriginal Health Research Ethics Committee in South Australia.
Findings
Summary and context history of service
The Central Australian Aboriginal Congress was formed at a public meeting in Alice Springs (a remote township of approximately 28,000 people) in June 1973, which was attended by over 100 Aboriginal people from across Central Australia.30 Established as an advocacy organization to provide a voice for Aboriginal people, its first service was a “tent program” to provide shelter to Aboriginal people living in town. In 1974, Congress’s founders called for a comprehensive approach to health that included addressing access to economic opportunities and nutrition, as well as health care. They lobbied the minister for Aboriginal affairs and minister for health to establish a multidisciplinary health service that would be “comprehensive, not selective” and that would incorporate preventive and curative approaches and be controlled by the Aboriginal community.30, p. 126 A medical service was established with a doctor, and later, in 1975, two Aboriginal people were trained and employed as health workers. In the late 1970s, Congress’s services expanded to include a dental clinic, a pharmacy, and welfare services. In the 1980s, they were further expanded to include an alcohol rehabilitation center, a child care facility, a women’s health and maternity service, family support services, and outreach health promotion programs in remote areas. A social and emotional wellbeing service was set up in the 1990s, followed by a male health service.30 Congress also provides PHC services in partnership with other remote Northern Territory Aboriginal communities in Central Australia. By the time our research program began in 2009, Congress employed approximately 300 staff.
The project started two years after the controversial Northern Territory Emergency Response began in the Northern Territory. Known as “the intervention,” it was prompted by the release of a report on child sexual abuse.31 During this intervention, the Australian government suspended the Racial Discrimination Act in order to instigate a range of health and social measures in the territory, including alcohol restrictions, compulsory income management, child health checks, and a ban on pornography.31 The intervention is widely regarded as a racist and paternalistic exercise, with considerable negative health impacts.32 However, it was a source of significant additional funding for Congress PHC services.
The study took place one year after the Australian prime minister’s apology to Australia’s Indigenous peoples in 2008, and the Closing the Gap national partnership agreements, which committed resources against Aboriginal and Torres Strait Islander health inequality reduction targets. In 2009, Congress had an annual budget of $27m. The Alice Springs Transformation Plan, a Commonwealth-funded collaboration between the Federal and Northern Territory Governments, was established in 2009 with the aim of expanding social support services and reducing homelessness in the town. Congress staff reported that the initiative improved intersectoral collaboration and dialogue on social determinants of health, and funded some of the service’s programs, such as the Safe and Sober alcohol treatment program and the Targeted Family Support Service.
In 2011, there were further modest increases in funding to Congress programs, including its Preschool Readiness Program, a trachoma program, and the Indigenous Chronic Disease Program. In 2012, it hired a renal PHC team and launched an Intensive and Targeted Family Support Service. There were few programs or positions lost over this period—one sexual offender program ceased, with responsibility transferred to the jail; two positions were lost when a regional center’s funding was cut; and a youth psychology service ceased.
In 2012, Congress leadership underwent significant changes, including a change of chief executive officer. Also that same year, Congress held an annual general meeting, where the community voted to make changes to Congress’s constitution and to register the service under the Corporations (Aboriginal and Torres Strait Islander) Act 2006. Our findings suggest that while such high-level changes—particularly the transition of chief executive officer—had the potential to be disruptive, Congress day-to-day operations and its community control and comprehensiveness remained largely unaffected.
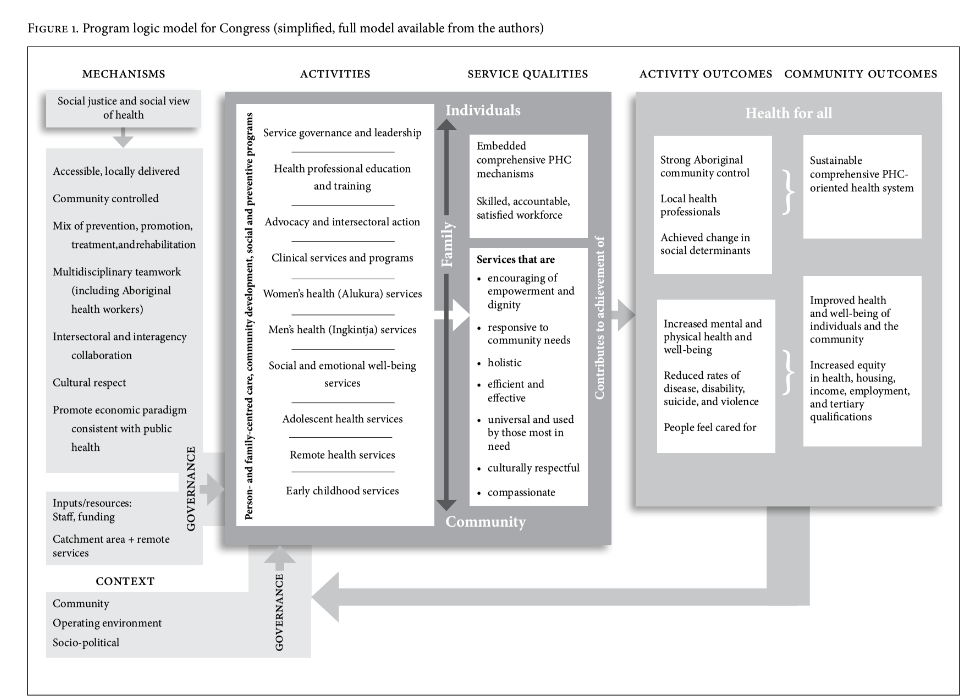
Program logic model
A simplified version of the program logic model developed in 2010 in collaboration with Congress staff is presented in Figure 1.25 The model captures the goals of the health service and the values that underpin it, and articulates the logic of the activities and strategies used to reach those goals. The elements on the left and bottom cover the primary mechanisms of comprehensive PHC that Congress sought to implement, as well as the service’s context and operating environment. These combined to inform, through the filter of governance, the service’s “space for action” to implement comprehensive PHC, including the activities that Congress undertook and the comprehensive PHC service qualities that it sought to enact in all its programs. These activities, conducted in accordance with the service qualities, in turn seek to contribute to activity outcomes, such as reduced rates of diseases and improved local social determinants of health. These activity outcomes fed into the aspirational goals of improving the health and well-being of individuals and the community, improving equity in health and other arenas for Aboriginal people, and having a sustainable and comprehensive PHC-oriented health system.
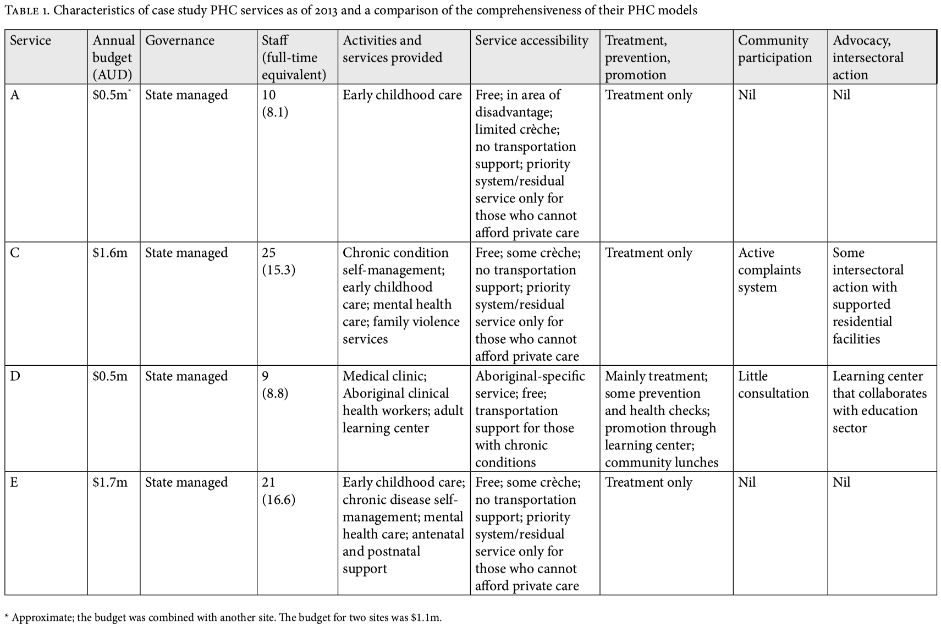
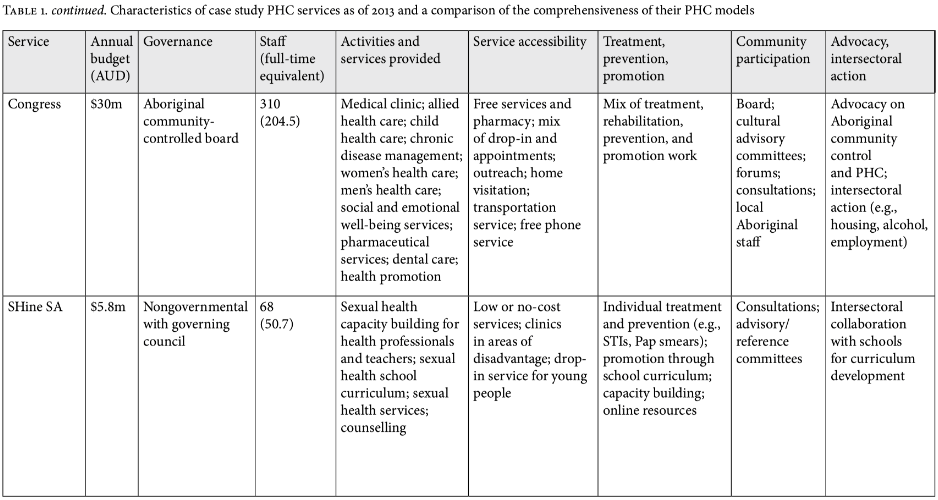
The key definitional elements of UHC—universal affordable access to promotive, preventive, and curative services—are clearly present in this model, even though the focus was on comprehensive PHC and even though UHC was not explicitly raised in the design of the model. The model also highlights the critical elements of advocacy and action on social determinants in order to improve health equity, thus addressing Harald Schmidt et al.’s concerns about a narrow focus on UHC.6 Again, while the logic models for the other partner services contained these same UHC elements, Congress demonstrated the most extensive implementation of these ideals. Table 1 shows the characteristics of all six services, as well as a comparison of their accessibility, treatment, prevention, and promotion work; community participation; and advocacy and intersectoral action. Congress exhibited a number of strengths over the other service models. These are presented below.
1. A more comprehensive multidisciplinary service
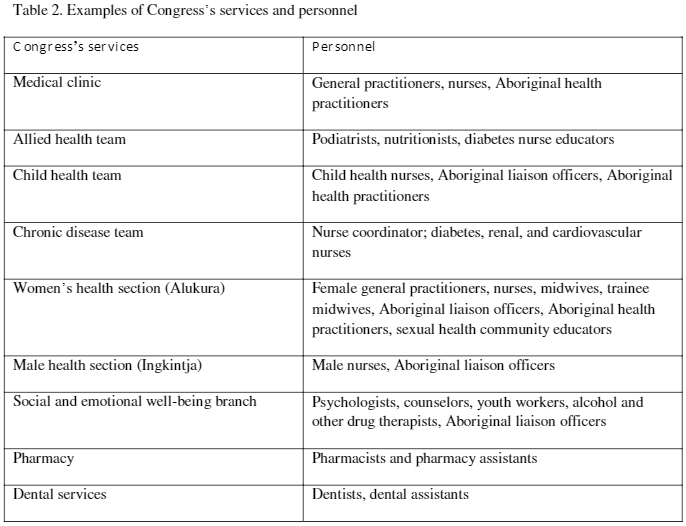
One question the World Health Organization includes in its consideration of UHC is “Which services are covered?”33, p. 12 Moreover, the World Bank report on UHC highlights that integration is vital to quality of care.34 Part of the necessity for a comprehensive PHC approach to UHC is the need for coverage to access a wide range of disciplines to support the health and well-being of individuals and the community. Universal coverage for only a narrow set of services is likely to have a reduced ability to address health inequities. Congress is an exemplar of such a free, multidisciplinary service. In addition to providing primary medical care with salaried general practitioners, Congress offers transportation services and employs a wide range of disciplines that provide many programs and services (see Table 2). This represents a far greater breadth of disciplines than those employed in the smaller South Australian services, allowing Congress to offer a more comprehensive, holistic response to the community’s health and well-being.
2. Multiple avenues of community participation
Of all the services studied, Congress enacted the widest range of strategies to ensure community participation. This is unsurprising given that Congress is community controlled and comes from a social movement emphasizing self-determination. The service’s board was the only example of structural participation in our research—that is, participation driven and controlled by the community, where the community can define the scope and agenda of its participation.27A number of other community participation strategies were documented at Congress, including taking community members to external forums to provide a voice for the local community, consulting community members about new programs, employing local Aboriginal health practitioners, and having cultural advisory committees which provided advice and guidance on cultural protocols. Staff felt that this community participation provided community members with a sense of ownership over the service.35 Community participation is a critical element of a rights-based approach to health, including through the politics of solidarity and civil society movements, and is hence valuable for framing UHC in terms of health as a human right.36
Engaging in community participation is rarely unproblematic, and Congress faced barriers to successful community participation in service planning. In particular, challenges were reported in balancing community desires with evidence-based medicine and with program requirements accompanying vertical funding sources, and in ensuring that views from both the town community and the geographically widespread, remote, and often very impoverished town camps were gathered.27
3. Greater scope of cultural respect and accessibility strategies
Congress demonstrated the greatest scope of strategies to address the accessibility of its services, including culturally respectful service delivery.37 It addressed the following elements:
- Availability through the provision of a free transportation service to all its service areas; outreach; home visitation; and a hybrid appointment system that allowed for walk-ins.
- Affordability through the provision of all services and medicines free of charge.
- Acceptability through the design of spaces to make the service welcoming and culturally respectful, the employment of local Aboriginal staff, and a consideration of cultural protocols.
- Engagement through interactions with the local community, including campaigns, awareness raising, and informal community development activities (such as cultural days that acted as entry points into the service).38
As explained above, strong community participation also promoted a sense of ownership that facilitated access. As a result of these accessibility initiatives, a senior staff member of Congress noted that a demographer had told him, “We are the only health service I’ve ever seen that could honestly say we are seeing 100% of the population every year.”35, p. 359 Congress’s success implies the importance of a comprehensive approach to accessibility (the specifics of which would vary by context) if the UHC goal of equity in access at an affordable cost is to be achieved.7
4. Health promotion and disease prevention
Congress participated in a wide range of disease prevention and health promotion activities in addition to providing treatment and rehabilitative services that included a medical clinic, a dental clinic, and mental health and addiction therapy (all of which also incorporate prevention and health promotion). Congress’s prevention and health promotion activities included early childhood and youth programs (e.g., antenatal care and birthing classes, immunizations, day care, a preschool readiness program, and youth outreach), adult health check-ups, healthy lifestyle groups, exercise groups, community health education (e.g., on young women’s and men’s sexual health), and mental health promotion (including for young people and the community at large).39
While the state-funded services in the study were stripped of their health promotion funding and mandate, Congress—like SHine SA, the other nongovernmental service in our study—was able to continue its health promotion work with strong organizational support due to the fact that it was not managed by the government and had a board committed to comprehensive PHC.40 However, Congress did feel pressure on its prevention and health promotion work in light of the need to balance this work with the need to meet an immediate and high ongoing demand for curative services for a “very sick” population.39, p. 716 Congress thus exhibited a comprehensive PHC approach to the spectrum of “treatment, prevention, and promotion” activities embedded in the definition of UHC. In its service reports, Congress estimated spending 70% of its time and resources on individual-level treatment, prevention, and promotion work, 10% on group work, and 20% on community health promotion, with an estimated 33% of its budget allocated to prevention and promotion work.
5. Advocacy and intersectoral collaboration on social determinants
Congress engaged in more efforts than the other services to address local social determinants; these efforts included an anti-violence campaign, participation in a local government-led “transformation plan” for the town, attention to housing issues, and advocacy around comprehensive PHC in multiple forums.41 The service’s employment of Aboriginal staff was also seen as a way to directly affect social determinants and thus improve population health. In addition, we documented Congress’s involvement in a community coalition that lobbied for alcohol supply restrictions in collaboration with community organizations and other sectors. This case study highlighted potential threats to successful advocacy, with some of the changes that the coalition had lobbied for implemented and then subsequently dismantled by a successive government, despite emerging evidence of the reduction in alcohol-related harm.29 However, the major change of increasing the minimum unit price of alcohol has been sustained. Additionally, as Congress staff were aware, many social determinants of the community’s health were not local in origin and were largely outside the health service’s area of influence.41
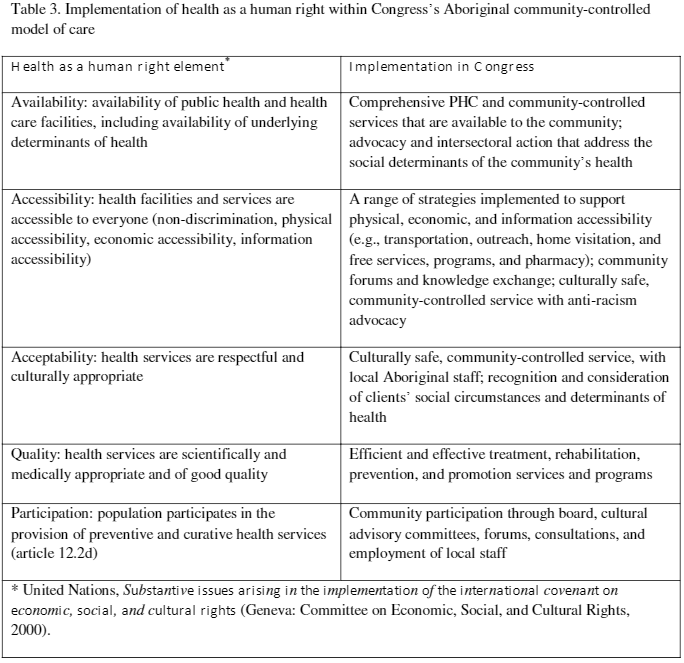
Table 3 summarizes how these characteristics relate to the implementation of health as a human right within Congress’ model of care.42
Discussion
Translating comprehensive PHC from ideal to practice raises many political and practical challenges. Nonetheless, it provides a potentially valuable model of accessible UHC that maintains a focus on health as a human right and on the reduction of health inequities, including through action on the social determinants of health. Congress implemented the most comprehensive approach to PHC among the services in our study. It was able to maintain its commitment to accessibility, community participation, disease prevention, health promotion, and action on social determinants, while the services in South Australia were unable to do so. Congress is located in a different jurisdiction (Northern Territory), with most of its funding coming from Commonwealth sources for Aboriginal community-controlled services. The policies of the Australian federal government are supportive of the need for comprehensive PHC within Aboriginal health services although less so within non-Indigenous services.43 The withdrawal from comprehensive PHC in South Australia was driven by the state government’s desire to reduce health care expenditures, cost-shift PHC to federally funded regional PHC organizations, and treat chronic physical conditions in out-of-hospital services. While the sexual health nongovernmental organization in this state (SHine SA) was less affected than the state-managed services, its prescriptive service agreement nevertheless constrained its comprehensive PHC practice. Congress and SHine SA maintained their conception of health as a human right, while this approach was no longer evident at the state-managed services. These two services’ nongovernmental nature seems to have protected them somewhat from changes in state government budgets and priorities.
One critical supportive factor is Congress’s public funding of approximately $30 million per year, an amount much higher than that enjoyed by the South Australian services. This has allowed Congress to implement a wide range of programs and overcome the access challenges faced by community members and the geographic challenges of such a remote setting. However, this funding alone does not explain Congress’s commitment to comprehensive PHC, as the service’s history indicates a dedication to human rights, comprehensive PHC, and universal access for Aboriginal and Torres Strait Islander peoples.30 Indeed, Congress implemented health and social programs during a long period of hostile and underfunded circumstances. The period of sufficient public funding is relatively recent and has enabled Congress to more fully implement its long-held commitment to comprehensive PHC.
Our research utilized a case study design with six partner services to provide an in-depth examination of local context and the practice of comprehensive PHC. We included one case study of an Aboriginal community-controlled service—the Central Australian Aboriginal Congress—whereas there are 150 other such community-controlled health services in Australia that vary in size, resources, staffing, and ability to implement comprehensive PHC. However, the Congress model is illustrative of what Aboriginal community-controlled services can accomplish and provides insight into the contextual factors that can support the implementation of comprehensive PHC; these factors include the provision of adequate public funding that allows for comprehensive service provision, being a nongovernmental organization with local community governance that enables advocacy, and policy support for a comprehensive PHC approach. While this may suggest that Congress is a “best case” of an Aboriginal community-controlled PHC, it is unlikely to be unique. Although we do not have comparable data from this research, other Aboriginal community-controlled health services— including the Aboriginal Medical Service Redfern (New South Wales), Rumbalara Aboriginal Cooperative (Victoria), and Winnunga Nimmityjah Aboriginal Health Services (Australian Capital Territory)—are equally highly regarded and demonstrate a comprehensive, rights-based model of PHC.
Action and advocacy on social determinants is particularly important when considering the ongoing colonization of Aboriginal and Torres Strait Islander peoples in Australia, as well as other Indigenous peoples worldwide, due to unequal power and voice, discrimination, and racism.44 In order to maintain health equity as the overarching goal, and UHC as the means to this end, the health-promotion aspect of UHC needs to include advocacy and action on social determinants.6 Furthermore, health sector actions need to be complemented by whole-of-government approaches to address social determinants—particularly for determinants that are nationally or internationally influenced, such as through trade and investment agreements and economic policies that affect wealth and income equity.45 Such efforts are integral to health as a human right.46
Our study did not gather comparative health outcome data that could yield further insight into the strengths and weaknesses of different PHC models and build the evidence base for effective, comprehensive PHC. Other Australian research has found that Aboriginal community-controlled health services achieve similar clinical outcomes as general practices despite having a more complex and disadvantaged caseload.46 The transfer of health services to Aboriginal community control has been associated with better access to doctors and Aboriginal health practitioners, more culturally respectful services, and a greater focus on population health.47
There is also Canadian evidence for community-controlled PHC. In one study, First Nation community health services that transitioned from government control to community control achieved a 30% reduction in hospital utilization rates compared to the non-community-controlled services, which the authors attributed to the positive health benefits of self-determination.48 A survey of over 200 community health centers in Canada serving non-Indigenous populations found that community-governed centers were more likely than non-community-governed centers to undertake work on social determinants and health equity, such as programs and advocacy on food security, homelessness and housing, poverty and income security, and refugee health services.49 While these associations may be correlational—with community governance, social determinants, and health equity ideals all stemming from a comprehensive PHC vision—these findings together suggest that community-controlled PHC services may lead to better health outcomes because of the ability of the service to take on responsibility for the health and well-being of its community, carve out space to take action on social determinants, and increase the community’s voice in decision making. This further highlights the community-controlled model as a potentially beneficial pathway to achieve UHC with a focus on health as a human right. While Aboriginal and Torres Strait Islander services target a specific population group, they indicate how UHC could be achieved with a comprehensive and rights-based approach if the comprehensive community-controlled model were employed for the wider population.
Conclusion
Our research highlighted the strengths of a well-funded Aboriginal community-controlled model in achieving UHC, based on a comprehensive PHC approach that covered treatment, prevention, and promotion activities and that was rooted in a commitment to health as a human right. The community-controlled model emerged as a promising form for the implementation of the UHC vision, which stresses health equity. The model suggests a range of benefits for population health over and above what a purely primary-medical-care or private-health-insurance-driven vision of UHC may have to offer, and it is worthy of serious attention and consideration in debates as countries strive to achieve the UHC Sustainable Development Goal.
Toby Freeman is a Senior Research Fellow at the Southgate Institute for Health, Society, and Equity, Flinders University, Adelaide, Australia.
Fran Baum is Director of the Southgate Institute for Health, Society, and Equity, Flinders University, Adelaide, Australia.
Angela Lawless is a Senior Lecturer at the Department of Speech Pathology, Flinders University, Adelaide, Australia.
Ronald Labonté is Professor and holder of the Canada Research Chair in Contemporary Globalization and Health Equityat the Institute of Population Health, University of Ottawa, Ottawa, Canada.
David Sanders is an Emeritus Professor at the School of Public Health, University of the Western Cape, Cape Town, South Africa.
John Boffa is Chief Medical Officer Public Health at the Central Australian Aboriginal Congress Aboriginal Corporation, Alice Springs, Australia.
Tahnia Edwards is a Manager at the Central Australian Aboriginal Congress Aboriginal Corporation, Alice Springs, Australia.
Sara Javanparast is a Senior Research Fellow at the Southgate Institute for Health, Society, and Equity, Flinders University, Adelaide, Australia.
Please address correspondence to Toby Freeman, Southgate Institute for Health, Society, and Equity, Flinders University, GPO Box 2100, Adelaide SA 5000, Australia. Email: toby.freeman@flinders.edu.au.
Competing interests: None declared.
Copyright © 2016 Freeman, Baum, Lawless, Labonté, Sanders, Boffa, Edwards, and Javanparast. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- World Health Assembly, Sustainable health financing, universal coverage and social health insurance, WHO Doc. WHA58.33 (2005).
- A. Maeda, E. Araujo, C. Cashin, et al., Universal health coverage for inclusive and sustainable development: A synthesis of 11 country case studies (Washington, DC: World Bank, 2014).
- United Nations, Goal 3: Ensure healthy lives and promote well-being for all at all ages. Available at http://www.hhrjournal.org/wp-content/uploads/sites/2//2014/09/Just2health.png
- P. Hunt, Economic, social and cultural rights: The right of everyone to the enjoyment of the highest attainable standard of physical and mental health, UN Doc. E/CN.4/2003/58 (2003).
- A. Chapman. “Evaluating Universal Health Coverage as a Sustainable Development Goal.” In Health and Human Rights Journal Blog, 2015. Available at: http://www.hhrjournal.org/2015/09/sdg-series-evaluating-universal-health-coverage-as-a-sustainable-development-goal/. Accessed 22/2/2016.
- H. Schmidt, L. Gostin, and E. Emanuel, “Public health, universal health coverage, and Sustainable Development Goals: Can they coexist?” Lancet 386/9996 (2015), pp. 928–30.
- T. O’Connell, K. Rasanathan, and M. Chopra, “What does universal health coverage mean?” Lancet 383/9913 (2014), pp. 277–79.
- J. Kutzin, “Anything goes on the path to universal health coverage? No.,” Bulletin of the World Health Organization 90/11 (2012), pp. 867–68.
- International Conference on Primary Health Care: Declaration of Alma-Ata, Alma-Ata, September 6–12, 1998.
- J. Walsh and K. Warren, “Selective primary health care: An interim strategy for disease control in developing countries,” New England Journal of Medicine 301/18 (1979).
- World Health Organization (WHO), World health report: Primary health care now more than ever (Geneva: WHO, 2008); R. Labonté, D. Sanders, C. Packer, et al., “Is the Alma Ata vision of comprehensive primary health care viable? Findings from an international project,” Global Health Action 7 (2014); F. Baum, D. Legge, T. Freeman, et al., “The potential for multi-disciplinary primary health care services to take action on the social determinants of health: Actions and constraints,” BMC Public Health 13/1 (2013), p. 460.
- Labonté et al. (see note 11).
- L. Pettigrew, J. De Maeseneer, M.-I. Anderson, et al., “Primary health care and the Sustainable Development Goals,” Lancet 386/10009 (2015), pp. 2119–21.
- M. McKee, D. Balabanova, S. Basu, et al., “Universal health coverage: A quest for all countries but under threat in some,” Value Health 16/1 Suppl (2013), pp. S39–45.
- I. McAuley, “Health funding: Somethinge else for Turnbull to worry about,” The Conversation. Available at https://theconversation.com/health-funding-something-else-for-turnbull-to-worry-about-61909.
- Australian Bureau of Statistics, 3238.0.55.001: Estimates of Aboriginal and Torres Strait Islander Australians, June 2011 (Canberra: Australian Bureau of Statistics, 2013).
- Ibid.
- Ibid.
- M. Cooke, F. Mitrou, D. Lawrence, et al., “Indigenous well-being in four countries,” BMC International Health and Human Rights 7/1 (2007), p. 9; J. Freemantle, K. Officer, and D. McAullay, Australian Indigenous health within an international context (Perth, WA: Telethon Institute for Child Health Research, 2007).
- Australian Institute of Health and Welfare, Mortality and life expectancy of Indigenous Australians 2008 to 2012: Cat. no. IHW 140 (Canberra: Australian Institute of Health and Welfare, 2014). Available at: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=60129548468; Australian Institute of Health and Welfare, The health and welfare of Australia’s Aboriginal and Torres Strait Islander people: An overview (Canberra: Australian Institute of Health and Welfare, 2011). Available at: http://www.aihw.gov.au/WorkArea/DownloadAsset.aspx?id=10737418955.
- A. Ziersch, G. Gallaher, F. Baum, et al., “Racism, social resources and mental health for Aboriginal people living in Adelaide,” Australian and New Zealand Journal of Public Health 35/3 (2011), pp. 231–37.
- Ibid.
- P. Torzillo, S. Rainow, P. Pholeros, et al., “Extending community health services,” in F. Baum, D. Fry, and I. Lennie (eds), Community health: Policy and practice in Australia (New South Wales: Pluto Press, 1992).
- J. Dwyer, J. Lavoie, K. O’Donnell, et al., “Contracting for Indigenous health care: Towards mutual accountability,” Australian Journal of Public Administration 70/1 (2011), pp. 34–46.
- K. Pholi, D. Black, and C. Richards, “Is ‘Close the Gap’ a useful approach to improving the health and wellbeing of Indigenous Australians?” Australian Review of Public Affairs 9/2 (2009), pp. 1–13; R. Aldrich, A. Zwi, and S. Short, “Advance Australia Fair: Social democratic and conservative politicians’ discourses concerning Aboriginal and Torres Strait Islander Peoples and their health 1972–2001,” Social Science and Medicine 64/1 (2007), pp. 125–37; J. Sherwood, “Colonisation: It’s bad for your health; The context of Aboriginal health,” Contemporary Nurse 46 (2013), pp. 28–40.
- United Nations Declaration on the Rights of Indigenous Peoples, G.A. Res. 61/295 (2008).
- F. Baum, T. Freeman, D. Sanders, et al., “Comprehensive primary health care under neo-liberalism in Australia,” Social Science and Medicine 168 (2016), pp. 43–52.
- A. Lawless, T. Freeman, M. Bentley, et al., “Developing a good practice model to evaluate the effectiveness of comprehensive primary health care in local communities,” BMC Family Practice 15 (2014), p. 99.
- Baum et al. (2013, see note 11); T. Freeman, F. Baum, A. Lawless, et al., “Revisiting the ability of Australian primary health care services to respond to health inequity,” Australian Journal of Primary Health 22 (2015), pp. 332–38.
- T. Freeman, F. Baum, G. Jolley, et al., “Service providers’ views of community participation at six Australian primary healthcare services: Scope for empowerment and challenges to implementation,” International Journal of Health Planning and Management 31 (2016), pp. E1–E21.
- T. Freeman, G. Jolley, F. Baum, et al., “Community assessment workshops: A group method for gathering client experiences of health services,” Health and Social Care in the Community 22 (2014), pp. 47–56.
- J. Anaf, F. Baum, T. Freeman, et al., “Factors shaping intersectoral action in primary health care services,” Australian and New Zealand Journal of Public Health 38/6 (2014), pp. 553–9.
- C. Rosewarne, P. Vaarzon-Morel, S. Bell, et al., “The historical context of developing an Aboriginal community controlled health service: A social history of the first ten years of the Central Australian Aboriginal Congress,” Health and History 9 (2007), pp. 114–43.
- Ibid. p. 126.
- Ibid.
- P. O’Mara, “Health impacts of the Northern Territory intervention,” Medical Journal of Australia 192/10 (2010), pp. 546–48.
- Ibid.
- Australian Indigenous Doctors’ Association and R.a.E. Centre for Health Equity Training, University of New South Wales, Health impact assessment of the Northern Territory emergency response (Canberra: Australian Indigenous Doctors’ Association, 2010); F. Proudfoot and D. Habibis, “Separate worlds: A discourse analysis of mainstream and Aboriginal populist media accounts of the Northern Territory Emergency Response in 2007,” Journal of Sociology 51/2 (2015), pp. 170–88.
- Lawless et al. (see note 28).
- Schmidt et al. (see note 6).
- WHO, The world health report: Health systems financing (Geneva: WHO, 2010), p.12.
- D. Cotlear, S. Nagpal, O. Smith, et al., Going universal: How 24 developing countries are implementing universal health coverage reforms from the bottom up (Washington, DC: World Bank, 2015).
- Freeman et al. (2016, see note 30).
- T. Freeman, F. Baum, A. Lawless, et al., “Reaching those with the greatest need: How Australian primary health care service managers, practitioners and funders understand and respond to health inequity,” Australian Journal of Primary Health 17, no. 4 (2011): 355-61.
- A. Grover, Right of everyone to the enjoyment of the highest attainable standard of physical and mental health, UN Doc. A/69/299 (2014); S. Rifkin. “Lessons from community participation in health programmes: A review of the post Alma-Ata experience,” International Health 1/1 (2009), pp. 31–36.
- Freeman et al. (see note 30).
- Freeman et al. (2011, see note 35); Freeman et al. (2015, see note 26); T. Freeman, T. Edwards, F. Baum, et al., “Cultural respect strategies in Australian Aboriginal primary health care services: Beyond education and training of practitioners, Australian and New Zealand Journal of Public Health 38/4 (2014), pp. 355–61.
- F. Baum, T. Freeman, A. Lawless, et al., “Community development: Improving patient safety by enhancing the use of health services,” Australian Family Physician 41 (2012), pp. 424–28.
- Freeman et al. (2011, see note 44), p. 359.
- O’Connell et al. (see note 7).
- F. Baum, T. Freeman, G. Jolley, et al., “Health promotion in Australian multi-disciplinary primary health care services: Case studies from South Australia and the Northern Territory,” Health Promotion International 29 (2014), pp. 705–19.
- G. Jolley, T. Freeman, F. Baum, et al., “Health policy in South Australia 2003–10: Primary health care workforce perceptions of the impact of policy change on health promotion,” Health Promotion Journal of Australia 25/2 (2014), pp. 116–24.
- Baum et al. (2014, see note 51), p. 716.
- Baum et al. (2013, see note 11).
- Anaf et al. (see note 32).
- Baum et al. (2013, see note 11).
- United Nations, Substantive issues arising in the implementation of the international covenant on economic, social, and cultural rights (Geneva: Committee on Economic, Social, and Cultural Rights, 2000).
- Commonwealth of Australia, National Aboriginal and Torres Strait Islander health plan 2013–2023 (Canberra: Australian Government, 2013).
- Rosewarne et al. (see note 33).
- A. Browne, V. Smye, and C. Varcoe, “The relevance of postcolonial theoretical perspectives to research in Aboriginal health,” Canadian Journal of Nursing Research 37/4 (2005), pp. 16–37; Sherwood (see note 22).
- Schmidt et al. (see note 6).
- F. Baum and D. M. Sanders. “Ottawa 25 years on: A more radical agenda for health equity is still required,” Health Promotion International 26/Suppl 2 (2011), pp. ii253–7.
- Hunt (see note 4).
- J. Dwyer, A. Martini, C. Brown, et al., The road is made by walking: Towards a better primary health care system for Australia’s First Peoples (Carlton South: Lowitja Institute, 2015); P. Mackay, A. Boxall, and K. Partel, Relative effectiveness of Aboriginal community controlled health services compared with mainstream health service (Canberra: Deeble Institute/Australian Healthcare and Hospitals Association, 2014); Aboriginal Health and Medical Research Council, Aboriginal communities improving Aboriginal health: An evidence review on the contribution of Aboriginal community controlled health services to improving Aboriginal health (Sydney: Aboriginal Health and Medical Research Council, 2015).
- R. Bailie, Menzies School of Health Research Local Evaluation Team, and Katherine West Health Board, Jirntangku Miyrta: Katherine West coordinated care trial local evaluation final report (Casuarina: Menzies School of Health Research, 2000); Department of Health and Ageing, The national evaluation of the second round of coordinated care trials: Final Report (Canberra: Commonwealth of Australia, 2007).
- J. Lavoie, E. Forget, T. Prakash, et al., “Have investments in on-reserve health services and initiatives promoting community control improved First Nations’ health in Manitoba?” Social Science and Medicine 71/4 (2010), pp. 717–24.
- Canadian Association of Community Health Centres, 2013 CHCs Organizational Survey. Available at http://www.cachc.ca/2013survey.
- UN (2000, see note 57).
- Ibid.