Nino Kiknadze and Leo Beletsky
Health and Human Rights 15/2
Published December 2013
Abstract
Background: After gaining independence following the dissolution of the Soviet Union, Georgia has aspired to become the region’s leader in progressive legal reform. Particularly in the realm of health care regulation, Georgia has proceeded with extensive legislative reforms intended to modernize its health care system, and bring it in line with international standards.
Objectives/Methods: As part of a larger project to improve human rights in patient care, we conducted a study designed to identify gaps in the current Georgian health care legislation. Using a cross-site research framework based on the European Charter of Patients’ Rights, an interdisciplinary working group oversaw a comprehensive review of human rights legislation pertinent to health care settings using various sources, such as black letter law, expert opinions, court cases, research papers, reports, and complaints.
Results: The study identified a number of serious inconsistencies, gaps, and conflicts in the definition and coverage of terms used in the national legislative canon pertinent to human rights in patient care. These include inconsistent definitions of key terms “informed consent” and “medical malpractice” across the legislative landscape. Imprecise and overly broad drafting of legislation has left concepts like patient confidentiality and implied consent wide open to abuse. The field of health care provider rights was entirely missing from existing Georgian legislation.
Discussion: To our knowledge, this is the first study of its kind in Georgia. Gaps and inconsistencies uncovered were categorized based on a short-, medium-, and long-term action framework. Results were presented to key decision makers in Georgian ministerial and legislative institutions. Several of the major recommendations are currently being considered for inclusion into future legal reform.
Introduction and background
Georgia regained its independence after the dissolution of the Soviet Union in 1991, when it faced a transition from the Soviet universal, centralized, and monolithic health care system. Similar to other post-Soviet countries in South Caucasus, organization of health care changed, with an increase in the role of municipal and regional authorities and private entities. In the sphere of service provision, Georgia’s system currently includes public and private, as well as hybrid institutions.1 In the realm of financing, Georgia shifted from its voluntary health insurance model to 2007 and 2012 state insurance programs, which covered children under age five, students, socially unprotected and pension-age persons, disabled children, and adults with severe disabilities.2 In February 2013, a new universal health care program started, expanding coverage to all uninsured individuals.3 Even though the funds allocated to health care have been increasing in the past years (doubling the health care budget in 2013), financing remains problematic.4
The aspiration of Georgia to become a leading reformer among the former Soviet and other Eastern European states has spurred a dynamic volume and rate of legislative activity over the course of the past two decades.5 In this context, the domain of health care has been of particular importance as a target of reform and innovation. Georgian legislation in this area spans the Constitution, international instruments to which Georgia is party, national laws, and regulations. These instruments cover various established and evolving aspects of health, including the rights of patients and research subjects; rights and duties of health care professionals and institutions; special provisions covering vulnerable groups (such as minors, persons with mental disorders, and people living with HIV/AIDS); human organ transplantation; and public health.
Driven by domestic and international forces, the development of the legislative canon governing health care has evolved significantly over the last two decades. In 1997, the Georgia Law on Health Care was adopted—the country’s first legal framework focusing on health and human rights.6 The law set out the fundamental principles of health care regulation and continues to determine its priorities. The Law on the Rights of Patients followed in 2000 by defining all major principles of patient rights and protections.7 Legal duties of physicians in relation to patients’ rights, as well as key aspects of training, professional development, and practice were in turn defined by the 2001 Law on Doctors’ Professional Practice.8 The adoption of the Law on Public Health followed in 2007, further elaborating on the rights of patients as it recalibrated the rules of interaction between individuals and the public health system.9 Other laws were also adopted during this period to regulate more narrow aspects of medicine and public health, in such areas as HIV/AIDS, psychiatry, and human organ transplantation.10
Historically, in Georgia, as elsewhere across the former Soviet Union, the provision of health care has not had a particularly pristine human rights record.11 Frequent violations of informed consent, confidentiality, privacy, and non-discrimination are only some of the areas where pervasive problems have been observed.12 Ineffective implementation and enforcement of health care legislation, due to structural issues and problems with resource allocation, at times render some of the legal instruments largely aspirational. If adequately implemented, the relatively new and numerous laws have the potential to address prevalent violations of human rights in the provision of health care in Georgia. Remedying these violations theoretically can be accomplished through several formal and informal mechanisms, including litigation and alternative forums for resolving claims, such as ombudspersons and ethics review committees. However, many of these systems are underutilized.
An assessment of the completeness in this extensive and relatively novel framework of legislation designed to safeguard human rights in the health sphere does not yet exist. As part of a larger project, “Human Rights in Patient Care,” described in depth by others in this special issue, we conducted a study aiming to identify gaps in the current Georgian health care legislation.13 Though not exhaustive, this paper identifies a number of major shortcomings in the legislative regime. To our knowledge, this is the first study of its kind in Georgia.
Methods
The methodology for this study is described in detail in Human rights in patient care: A practitioner guide—Georgia and other project documents.14 Briefly, in parallel with efforts of other national working groups convened to assess the gaps in human rights in patient care legislation, experts in health care legislation, public health policy, bioethics, media, and the medical insurance sector convened in an interdisciplinary working group on this topic in Georgia. The working group had a team leader, who facilitated meetings and communication of information. Using a comprehensive human rights in patient care framework based on the European Charter of Patients’ Rights, the group oversaw and conducted a comprehensive review of human rights legislation pertinent to health care settings in Georgia.15 In collaboration with the full working group, individual member experts researched and synthesized information from various sources, such as black letter law, expert opinions, court cases, research papers, reports, and complaints. They identified relevant norms regulating specific issues; assessed the adequacy of the norms; and drew conclusions as well as recommendations on the extent to which certain legal provisions needed to be modified.
Based on group consensus, the study classified the gaps in legislation into three categories for action, corresponding to short-, medium-, and long-term priorities. Three university professors reviewed the findings midway as well as at the completion of the study process. The results were presented at the office of the Open Society Georgia Foundation before representatives from the Ministry of Labor, Health, and Social Affairs, including the Deputy Minister of Health; parliamentarians; and experts in the field of health care. This article presents a synthesis of these findings.
Results
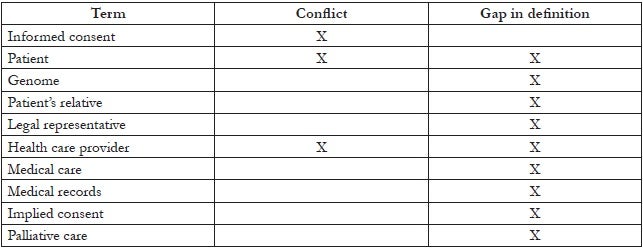
We identified a number of serious inconsistencies, gaps, and conflicts in the definition and coverage of terms used in the national legislative canon pertaining to human rights in patient care. Below, we provide an overview of the most egregious examples. A full list appears in Table 1.
Informed consent
The Law on Health Care and the Law on Public Health provide significantly different definitions of “informed consent,” creating a conflict in both letter and spirit of the law. Under the Law on Health Care, “informed consent” is the consent of the patient, his or her relative, or legal representative to perform a necessary medical intervention after the risks of the procedure have been explained.16 This definition covers only a small subsection of the definition of “informed consent” under the Law on the Rights of Patients, which also indicates that the patient has to be informed of the essence of the proposed treatment as well as its necessary results, expected results, alternative options of treatment and their risks and effectiveness, expected results of refusal of medical care and other accompanying financial and social issues regarding the proposed treatment.17 Thus, the definitions in these two laws significantly differ and can cause divergent outcomes depending on which legal standards are followed.
Patient’s relative
In both the Law on the Rights of Patients and the Law on Health Care, the term “patient’s relative” is defined as a person who enjoys a preferred right to participate in decision making as it relates to the provision of medical care for a patient or after a patient’s death.18 However, no legislation actually establishes the order of persons enjoying this preferred right to participate in the decision-making process. The definition of the term “patient’s relative” is therefore dangerously vague.
Implied consent
A prime example of definitional ambiguity resulting from flawed legal drafting relates to the term “implied consent.” The term is defined in the Law on the Rights of Patients as the situation when, although there is an absence of a written or oral agreement to care, “a patient has asked a physician for medical advice and the physician in turn has spoken to the patient, examined him, etc.”19 The vagueness of this definition—especially with the use of the term “etc.”—allows for health care providers to misuse what constitutes “implied consent” and permits a virtually limitless list of possible interventions to be subject to “implied consent.” Regulation of patient consent carries particular importance in relation to human rights in patient care, and the law must provide exhaustive and unambiguous instances of when a patient’s consent can be considered implied. The vagueness of this definition, especially the use of the term “etc.” within the actual definition, opens a door to misuse by health care providers of what constitutes “implied consent.”
Table 1. Terminology issues identified in health care legislation of Georgia
Medical malpractice
The Law on Health Care defines medical malpractice as “unintentional diagnostic and/or therapeutic measures prescribed improperly for a patient’s condition by a physician, which has become a direct cause of inflicted damage.”20 Out of several legal flaws associated with this definition, it is noteworthy that “medical malpractice” under the law equates to physician’s malpractice, since it implies that a physician is the only person who can engage in medical malpractice. In reality, medical malpractice can be caused not only by a physician but also by any professional involved in the provision of medical care, such as physician assistants and technical personnel, or even by a medical institution.Other shortcomings in the definition of medical malpractice include the usage of the word “damage,” which is overly vague.
Confidentiality
Confidentiality of patient information is one of the most crucial issues in the protection of patients’ rights. Both the Constitution of Georgia and the General Administrative Code of Georgia guarantee the right of confidentiality of information.21 Despite this, the Law on Health Care does not ensure the protection of the right of patient confidentiality, and furthermore, even violates this right. Pursuant to this law,
[m]edical employees and all other employees of a medical institution shall be obligated to preserve medical secrets, except in cases when the disclosure of confidential information is requested by a relative or legal representative of the deceased person, the court, investigative bodies, or this is necessary for ensuring public security and protection of the rights and freedoms of others.22
This definition implies that an investigator who requests a patient’s health record from a patient’s physician or medical institution is entitled to receive such information, without need for a court order or decision.
The Law on the Rights of Patients does not define the circumstances and extent to which a patient’s information is protected. The issue is relatively clearer and better regulated under the Law on Medical Practice, which provides a list of concrete cases when an independent medical entity has the right to disclose confidential information concerning a patient’s health status and private life:
- A patient authorizes disclosure.
- Nondisclosure of information endangers the health and/or life of a third person (whose identity is established).
- There is a reasonable suspicion as to the existence of a disease subject to mandatory registration.
- The information is provided to other medical personnel participating in the medical care.
- Disclosure of information is required for the forensic medical examination.
- Disclosure of information is requested by law enforcement agencies in accordance with a court decision.
- The information is provided to state agencies for establishing social privileges for a patient.
- In such a case a patient’s consent to disclosure of information is required.
- The information is for education/scientific purposes and the data are presented so that identifying an individual is impossible.
However, this legislation still contains flaws: lack of protection for a patient’s right to confidentiality, overly-broad interpretation of the term “reasonable doubt,” and lack of definition for grounds for disclosing information from forensic medical examinations.
Patients’ right to information
Shortcomings are observed in relation to informing patients about their right to information, which constitutes one of the most significant rights of the patient. The Law on the Rights of Patients provides a list of instances in which patients—or their relatives or legal representatives in the case of a patient’s legal incapacity or inability to provide consent—enjoy the right to receive information. The law states that patients, and with their consent or in the case of legal incapacity, their relatives or legal representatives enjoy the right to:
- Become familiar with their medical records and request changes to existing information in them. Medical records should contain both the original information and the new information provided by a patient, his or her relative, or legal representative; and
- Request copies of any part of their medical records.
Patients or their agreed-on representatives also have the right to receive information on:
- Existing resources for medical care, the fees charged, and forms of payment accepted;
- The rights and obligations of a patient under the legislation of Georgia and the internal regulations of a medical institution;
- Proposed preventive, diagnostic, treatment, and rehabilitation services; their accompanying risks; and likely effectiveness;
- Results of medical examinations;
- Alternatives to the proposed medical care, their accompanying risks and likely effectiveness;
- Likely outcome if proposed medical care is refused;
- Diagnosis and expected prognosis, as well as the treatment process; and
- Identity and professional experience of person providing medical care.
The list is exhaustive, which could lead to the restriction of a patient’s right to information.
It must also be noted that although the law grants patients or their legal representatives the right to receive information, the law is silent as to the obligation of a medical institution or medical personnel to provide such information.
Patient safety
Despite its significance, the health care legislation of Georgia pays almost no attention to the issue of patient safety and is totally silent on the term itself. Georgian legislation not only underregulates the individual components of patient safety (such as medical malpractice or safety of medical devices), but also contains no provisions acknowledging patient safety as a concept.
Rights and obligations of health care providers
Another alarming issue is that the health care legislation of Georgia does not regulate the rights of health care providers. The legislation only provides meager norms determining the rights of physicians. There are some provisions containing certain rights, but their content is vague and incomplete. For instance, under the Law on Health Care, in the case of patients’ incapacity, a physician has the right to assist them, if their relatives or legal representative so request.23 Furthermore, a physician enjoys the right of implied consent when a capable patient does not resist in any form in the course of providing medical care.24
In addition, a physician is only allowed to refuse medical care in two circumstances, if:
- The continuity of medical care to a patient can be ensured and a patient does not require emergency medical care; or
- A physician’s life would be at risk during the provision of medical care.25
The Law on Health Care also includes the right of a physician to prescribe any medicine and enact any method of treatment in the interests of protecting the health of a patient.26 The other health care laws are silent on the rights of health care providers.
Discussion
This overview of Georgia’s legislative canon in the realm of human rights in patient care helps identify a number of shortcomings in domestic legislation covering patient and provider rights. These findings have critical public health implications because the provision of high-quality health care and public health services cannot occur without a robust legal framework to define and operationalize the rights of patients and providers. This is as true in obvious areas such as medical malpractice and patient safety, as it is in extending and protecting the rights of health care providers, broadly defined. Highlighting gaps and ambiguities in these legislative instruments is also important both as an aspect of the normative agenda of the state to improve human rights protections in Georgia, as well as to the state’s programmatic goal of developing a more actionable human rights regime.
Based on the study summarized here, a package of legislative amendments was prepared and presented to the Ministry of Labor, Health, and Social Affairs. Currently, the Ministry is reviewing the suggested amendments and planning to issue orders to fix deficiencies in the country’s health care legislation. The study has also served as a reference guide for the Ministry’s legislative work, whose deliberations in this realm are underway.
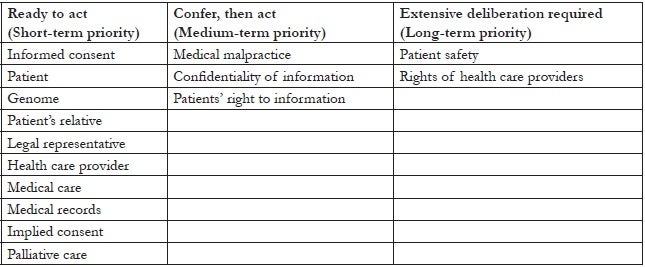
Based on these findings, a number of recommendations follow. The problematic issues fall into three short-, medium-, and long-term priority categories of action: “Ready to Act,” “Confer, then Act” and “Extensive Deliberation Required.” Table 2 provides an overview of the issues in each category.
Table 2. Categories of definitional gaps identified in health care legislation of Georgia
Ready to act
Issues which are associated with technical legal flaws, such as definitions of informed consent, the rights of a patient’s relative, and implied consent can be classified as “Ready to Act,” since remedying such issues does not require additional discussions about health care policy. The recommendations offered are sufficient for amending the respective legislative acts.
The Law on the Rights of Patients and the Law on Health Care as well as any other legal instruments that contain the term “patient’s relative” should establish the priority ordering of ascending and descending relatives, or at least adopt the procedural framework established by Article 1336 of the Civil Code of Georgia. The article determines 1st class heirs (decedent’s children, spouse and parents, grandchildren, great grandchildren and great-great grandchildren), 2nd class (siblings of the decedent; nieces and nephews and their children), 3rd class (grandparents; great grandparents), 4th class (uncles and aunts), 5th class (first cousins; their children). The ambiguity and vagueness of the term “implied consent” under the Law on the Rights of Patients could be addressed by eliminating the word “etc.” and providing an exhaustive list of the situations and legal triggers when implied consent can be invoked. For medical malpractice, the issue of unacceptably restrictive scope could be resolved by using the term “health care provider” instead of “physician” in defining the term “medical malpractice” because “health care provider” extends liability to other individuals and institutional entities involved in the provision of health care. In order to resolve the current ambiguities, the legal definition of medical malpractice could be formulated as follows: “Medical malpractice shall be an unlawful action or act of omission of a health care provider, which has resulted in a patient’s death or disorganization of health, or has inflicted moral and/or material damage to a patient.”
In the realm of confidentiality, the Law on Health Care should be amended so that a patient’s information is available to third parties, including investigative bodies, only after provision of a court order. In the Law on Medical Practice, the term “reasonable doubt” should be defined to avoid wide interpretation. The law must also specify when it is justified to disclose patient information for forensic medical examination purposes. Either a court order or the consent of the patient or his or her legal representative must be required for disclosing the information.
Conversely, the Law on the Rights of Patients must expand the characterization of cases when information should be provided to next of kin or guardians of incapacitated individuals. It should also specify that patients possess the right to receive any other medical information related to their medical histories, treatment procedures, and personal identity. The obligations of medical professionals and institutions to provide information in such cases must be clearly delineated.
To avoid legal conflicts, gaps, duplications, technical flaws, and vague norms found in current health care legislation discussed in the “Ready to Act” domain of issues, unification, and codification of health care laws is desirable. Owing to significant influence from the continental legal system, the Georgian legal system offers an opportunity for such unification by the creation of what might be titled the “Code of Health Care.” This approach can eliminate the need for different definitions for identical or similar terms and concepts, and would help to avoid conflicts, inconsistencies, and other gaps currently found both in terms of legal procedure and content.
Confer, then act
There is a rather large group of issues where legislative action can be taken only after choices and priorities are first determined in public policy arena. For issues falling under this category, recommendations of technical legal analysis are not sufficient for remedial legal reform; however, these findings do help flag legislative norms that must be fleshed out or otherwise amended. These “Confer, Then Act” issues include the topics of medical malpractice, confidentiality of information, and patients’ right to information.
The situation is more complex regarding the issues in this domain, as decisions need to be made in the public policy area first and only then can these decisions be reflected in legislative reform. Furthermore, ambiguities and controversies in the health care policy arena need to be resolved and priorities defined before legislative action.
Extensive deliberation required
The study has identified several topics, such as patient safety and rights of health care providers, with respect to which there are no clear approaches in the current legislative canon in Georgia. These issues require conceptual consideration and synthesis of approaches; only after these steps can policy decisions be made. Only then, after those policy decisions have been made, will it be possible to bring the legal system into compliance with the requirements of a health care system emphasizing human rights in patient care. Hence, with regard to the issues in “Extensive Deliberation Required” as compared to the other categories, there is a longer road ahead before legislative amendments can be made to effectively address these issues.
In the area of patient safety, Georgia first needs to formulate a state policy on the topic and then bring the legislation into compliance with such policy. The article determines 1st class heirs (decedent’s children, spouse and parents, grandchildren, great grandchildren and great-great grandchildren), 2nd class (siblings of the decedent; nieces and nephews and their children), 3rd class (grandparents; great grandparents), 4th class (uncles and aunts), 5th class (first cousins; their children). The approach towards this issue should include at least two areas: regulation and implementation. For regulation, legislation needs to be improved with respect to patient rights and patient safety. For implementation, an authorized agency in this area needs to be determined, and national policy and safety standards need to be developed to enforce these concepts. In addition, it is necessary to implement projects and activities aimed at eliminating specific risks that pose a danger to patient and provider occupational safety.
To accomplish needed progress in the rights of health care providers, we recommend that a special section in the health care legislation of Georgia be dedicated to regulating and guaranteeing the rights of health care providers, perhaps in the Law on Health Care. At the very least, legislative amendments must cover issues such as contractual rights of health care providers and protections covering faith and religion.
Limitations
This study has several limitations. It was not the project’s goal to present an exhaustive inventory of all the gaps in the health care legislation of Georgia. It was also beyond the scope of the project to conduct empirical research to uncover health outcome implications or specific ways in which the gaps in definition, specificity, and nomenclature that we identified affect the implementation of the laws on the ground. Rather, this article represents an effort to identify and illustrate major shortcomings in the legislative canon in order to help set an agenda for both legal and policy reform, as well as future research. Our hope is that the findings will continue to inform advocacy and legislative efforts to develop and effectively implement relevant amendments in this important and constantly evolving field.
Conclusion
Even though current laws claim to address pervasive human rights violations in health care settings, the current framework squarely ignores the rights of health care providers, and the legislation fails to adequately cover confidentiality of information, the right to information, and patient safety issues. Shortcomings in the definition of some key terms in health care laws leave room for ambiguity and varied interpretations. Underregulation of some crucial rights of patients and providers suggests that the health care legislation of Georgia does not fully ensure an effective human rights-based framework.
Although this analysis has focused on a legislative approach and related remedies, issues we identified extend beyond the legislative domain. While legislation is one of the basic pillars of the health care system, flaws identified in it require not only the issuance of legislative amendments but also, in many cases, public policy deliberations and philosophical value judgments. Future research should address the evolution of human rights protections in patient care and also monitor the street-level implementation of these legal instruments.
Acknowledgements
Funding for this research was provided by the Open Society Foundations.
Nino Kiknadze, LLM, MPA, is a PhD candidate at Ilia State University, Georgia.
Leo Beletsky, JD, MPH, is Assistant Professor of Law and Health Sciences at the Northeastern University School of Law and Bouvé College of Health Sciences, Boston, USA and Adjunct Professor at the Division of Global Public Health, UCSD School of Medicine, San Diego, USA.
Please address correspondence to Nino Kiknadze, “Law, Media, and Health Project,” Open Society Foundation of Georgia, 10 Chovelidze Street, 0109, Tbilisi, Georgia, email: nkiknadze@osgf.ge.
References
1. L. Beletsky, T. Ezer, J. Overall, et al., Advancing human rights in patient care: The law in seven transitional countries (Open Society Foundations, 2013), p. 39. Available at http://www.opensocietyfoundations.org/sites/default/files/Advancing-Human-Rights-in-Patient-Care-20130516.pdf.
2. Ibid., p. 44.
3. Ibid.
4. Ibid.
5. E. Baumann, “Post-Soviet Georgia: It’s a long, long way to ‘modern’ social protection …,” Economies et Societes 46/2 (2012), pp. 259–285. Available at http://horizon.documentation.ird.fr/exl-doc/pleins_textes/divers12-07/010056159.pdf.
6. K. Aslanishvili, M. Djibuti, A. Imedashvili et al., Human rights in patient care: A practitioner guide—Georgia (Georgia Open Society Foundation, 2011), p. 131. Available at http://www.opensocietyfoundations.org/sites/default/files/Practitioner-Guide-Georgia-English-20130516.pdf.
7. Ibid.
8. Ibid.
9. Ibid.
10. Ibid.
11. See generally, A. Koryagin, “The Involvement of Soviet Psychiatry in the Prosecution of Dissenters,” British Journal of Psychiatry 154/1 (1989), pp. 336–340; D. Balabanova, M. McKee, J. Pomerleau, et al., “Health service utilization in the former Soviet Union: Evidence from eight countries,” BMC Health Services Research 39/6 (2004), pp. 1927–1949; see also L. Beletsky et al. (see note 1), pp. 9–10.
12. World Health Organization Regional Office for Europe and European Observatory on Health Systems and Policies, “Full list of health systems in transition (HiT) summaries.” Available at http:// www.euro.who.int/en/who-we-are/partners/observatory/health-systems-in-transition-hit-series/hit-summaries; see generally, E. Baumann (see note 6); J. Cohen, N. Kass, and C. Beyrer, “Human rights and public health ethics: Responding to the global HIV/AIDS pandemic,” in C. Beyrer and H. F. Pizer (eds), Public health and human rights: Evidence-based approaches (Baltimore, MD: Johns Hopkins University Press, 2007), pp. 362–390.
13. L. Beletsky et al. (see note 1), p. 16; see generally Open Society Foundations (see note 7).
14. L. Beletsky et al. (see note 1), at 11–13; Open Society Foundations (see note 7).
15. Active Citizenship Network, “European Charter of Patients’ Rights” (Rome: Active Citizenship Network, November 2002). Available at http://ec.europa.eu/health/ph_overview/co_operation/mobility/docs/health_services_co108_en.pdf; Open Society Foundations (see note 7), pp. 7–9.
16. Law on Health Care, Republic of Georgia (1997), Art. 3(j) [in Georgian] [author’s translation].
17. Law on the Rights of Patients, Republic of Georgia (2000), Art. 4(b).
18. Law on Health Care (see note 16), Art. 3(r); Law on the Rights of Patients (see note 17), Art. 4(e).
19. Ibid., Art. 4(k).
20. Law on Health Care (see note 16), Art. 3(o).
21. Constitution of Georgia (1995), Art. 20(1). Available at http://www.parliament.ge/files/68_1944_951190_CONSTIT_27_12.06.pdf.
22. Law on Health Care (see note 16), Art. 42.
23. Ibid., Art. 30.
24. Ibid.
25. Ibid., Art. 37.
26. Ibid., Art. 51.