Julia Smith
Abstract
Despite a history of championing HIV/AIDS as a human rights issue, and a rhetorical commitment to health as a human right, European states and institutions have shifted from a rights-based response to a risk management approach to HIV/AIDS since the economic recession of 2008. An interdisciplinary perspective is applied to analyze health policy changes at the national, regional, and global levels by drawing on data from key informant interviews, and institutional and civil society documents. It is demonstrated that, in the context of austerity measures, member states such as the UK and Greece reduced commitments to rights associated with HIV/AIDS; at the regional level, the EU failed to develop rights-based approaches to address the vulnerabilities and health care needs of key populations affected by HIV/AIDS, particularly migrants and sex workers; and at the global level, the EU backtracked on commitments to global health and is prioritizing the intellectual property rights of pharmaceutical companies over the human rights of people living with HIV/AIDS. The focus within and from the EU is on containment, efficiency, and cost reduction. The rights of those most affected are no longer prioritized.
Introduction
The EU and European states have in many ways been leaders in both human rights and the HIV/AIDS responses. The European Convention on Human Rights and the European Social Charter both recognize the right to health. European countries were among the first to adopt harm reduction approaches to mitigate HIV infections through injecting drug use, to champion the rights of men who have sex with men (MSM), and to lead in the formation of global health institutions to address HIV/AIDS epidemics in lower- and middle-income countries (LMICs).1 This article asks how responses to HIV/AIDS have changed within and from Europe since the economic recession that began in 2008. While much has been written about the impact of austerity measures on health in Europe, and on the outcomes of these policies in specific states, little of it focuses explicitly on HIV/AIDS.2 As the HIV/AIDS response pioneered a rights-based response to health within Europe, it presents a critical case to explore policy changes.
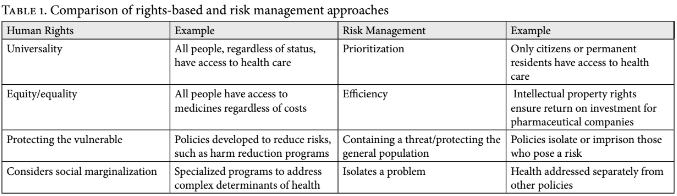
Despite a history of championing HIV/AIDS as a human rights issue, and a rhetorical commitment to health as a human right, European states and institutions have shifted from a rights-based response to a risk management approach since the economic recession of 2008. Ines Keygnaert et al. define a rights-based approach to HIV/AIDS as one that “considers health as a human right and assesses policies, programs and legislation accordingly, expecting them to promote health and guarantee access to health care for all independently of any status. This approach is rooted in the overarching principle of universality.”3 While campaigns for health-related rights have shifted focus over time, the key principles of access to health care for all, support for the most vulnerable, and protection from stigma and discrimination have been key pillars of rights-based responses related to HIV/AIDS since the 1980s. In contrast, a risk management approach is defined as “the identification, assessment, and prioritization of risks followed by coordinated and economical application of resources to minimize, monitor, and control the probability and/or impact of unfortunate events or to maximize the realization of opportunities.”4 While not necessarily mutually exclusive, key differences between rights-based and risk management approaches relate to principles of universality versus prioritization; and a focus on equity/equality as opposed to economic efficiencies (see Table 1). There is also a notable difference between the goal of addressing a threat to protect the most vulnerable, and containing it to protect those not yet affected.
While the first section of this article describes processes in place prior to the creation and expansion of the EU, the term ‘European states’ refers to those states who are presently members. The European institutions that are discussed are those engaged in lawmaking and policy setting, including the European Parliament, European Commission, and Council of the European Union. The paper presents three levels of analysis that represent different but overlapping concepts of Europe: Europe as a group of states, Europe as a regional entity, and Europe as a global actor. The first level focuses on policies within European member states, facilitating discussion (through select case studies) of how health policies, which remain a national competence, have shifted. The second level is regional, considering how the European Parliament has responded to issues related to HIV/AIDS within its governance jurisdictions. Finally, the paper considers how the European Commission’s engagement with the global HIV/AIDS response has changed. This multilevel analysis is crucial for two reasons. First, HIV/AIDS is a transboundary health threat that cannot be contained or addressed solely within one state or region and thus requires action across governance levels.5 Second, shifts from rights-based approaches to risk management approaches have occurred at all three levels, suggesting a regional shift that calls for further investigation and redress.
This topic is approached from an interdisciplinary perspective. In order to gain perspectives on more recent events that are not documented in the scarce literature on Europe and HIV/AIDS responses, the analysis draws on data from 12 key informant interviews with members of civil society organizations (7), civil servants within European institutions (2), and staff from global health institutions (3). Interviewees were selected purposefully and interviews were conducted in person or over the phone/Skype between January 2013 and May 2014. Transcripts were analyzed using iterative, inductive content analysis to identify key themes and policy processes, and the interviewees’ perspectives on them. These were triangulated with secondary literature and document analysis of publications from civil society organizations, European institutions, and global health institutions. Ethical approval for this research was granted by the Ethics in Research Committee at the University of Bradford, where the author was based at the time.
Early rights-based response to HIV/AIDS
In the early 1980s, a mysterious cause of death among young adults in Europe resulted in hysteria and fear. WHO reported in retrospect, “AIDS was – and in absolute, global terms still is – a stinging challenge to the values of modernity received, for better or worse, from Europe’s Age of Enlightenment. Affluent, confident, gender-progressive, often social-democratic welfare states awoke, in the early 1980s, to an uncomfortable reminder of their human frailty.”6 Early responses focused on containing the virus, often stigmatizing those already infected. For example, far-right French politician Jean-Marie Le Pen proposed implementing “sidatoria,” which would have confined people living with HIV/AIDS (PLWHAs) in prison-like hospitals.7 Such proposals had counterproductive outcomes, such as reducing testing, as those at risk feared that if they knew their status they would be isolated and prosecuted. Meanwhile, public health programs focused on individual behavior. In 1987, the British government launched a major advertising campaign with the slogan “AIDS: Don’t Die of Ignorance.”8 Such approaches lacked appreciation for the sociopolitical context of the epidemic.9
As efforts to produce a vaccine or treatment failed, and as public health approaches bordered on blaming individuals for their positive status, PLWHAs and their allies developed an alternative response. In 1983, the Terrence Higgins Trust formed in London to support those affected by HIV/AIDS, and in 1984, Aides formed in Paris with a similar mandate.10 Over the next decade, PLWHA support groups mushroomed, providing palliative care to the sick, confidential testing to those at risk, and counseling to those affected.11 Together with health professionals and human rights activists, these groups advocated for a response that recognized HIV/AIDS as an exceptional health issue requiring the empowerment of those most affected.12
In the absence of treatment options, public health programs increasingly adopted this human rights frame. European states, after their initial response of punishment and stigmatization, provided favorable policy environments for the realization of a rights-based response. In 1976, most had ratified the International Covenant on Economic, Social and Cultural Rights (ICESCR), which recognized the right to health. In many European states, the feminist struggles of the 1970s had resulted in greater access to contraception, which made the promotion of condoms and other means of prevention less contentious than in, for example, the American context.13 Many states already had policies in place to reduce risks associated with sex work and drug use, such as decriminalization and harm reduction programs. The UK started the first syringe exchange programs to prevent HIV as early as 1987.14 Most European countries also accepted access to health care as a human right by providing comprehensive public health insurance. Due to the favorable policy and social context, there was widespread adoption of rights-based prevention strategies. In 1994, 42 states joined forces with AIDS service organizations (ASOs) at the Paris AIDS Summit, signing a declaration committing to a rights-based response to the epidemic, led by those most affected.15
In response to increasing awareness of the global scale of the HIV/AIDS epidemic, European states were among those advocating for a more coordinated global response. Scandinavian countries played a key role in the formation of the United Nations Joint Program on HIV/AIDS (UNAIDS) in 1994, and the UK played a primary role in the creation of the Global Fund to Fight HIV/AIDS, Malaria and TB in 2001.16 European countries, such as France, led the formation of UNITAIDS, which aims to improve treatment access.17
Reflecting member state practices, the European Union developed its regional and neighborhood policies in line with a rights-based approach. In response to the growing epidemic in Eastern Europe, in 2004, 52 EU member states and civil society observers gathered in Dublin for a conference on “Breaking the Barriers – Partnership to fight HIV/AIDS in Europe and Central Asia.”18 The resulting declaration called for universal access to treatment, two years before the UN Declaration on Universal Access.19 The EU maintained support for Universal Access campaigns during the initial negotiations of the Doha Round of World Trade Organization (WTO), siding with PLWHAs and their allies, as opposed to the US and pharmaceutical companies.20
In 2007, the European Commission announced its four-year Programme for Action to Confront HIV/AIDS, Malaria and Tuberculosis.21 The program asserted European leadership in the HIV/AIDS response in general, and a commitment to a rights-based response in particular.
European states: The human costs of austerity
Risk management is generally associated with financial governance, as opposed to health governance, but the two fields inevitably overlap.
Due to austerity measures, many European states have deprioritized a rights-based response to HIV/AIDS in order to mitigate financial risk. The UK and Greece provide two examples of this trend. These countries were selected as critical cases based on the breadth of the health-related austerity policies they implemented post-2008, and on their geographic location; in order to include examples from Northern and Southern Europe. While these two countries are not a representative sample, nor the findings generalizable, they present a similar policy shift in two very different European states.
The United Kingdom
In the 1990s, the UK developed one of the most progressive HIV/AIDS responses, ensuring social protection of PLWHAs. These programs recognized that in order to enjoy the right to health, PLWHAs require not only treatment, but also food security, stable living conditions, and psychosocial support. Government funding provided food aid programs and resources to support groups. Since 2008, however, the UK government has cut social spending and hollowed out this rights-based response.22
The Welfare Reform Act of 2012 had a number of negative impacts on PLWHAs. Previously, PLWHAs who were unable to work because of their illness could apply for the Incapacity Benefit. The Reform Act initiated a reassessment process of this benefit, which aimed to move people from the Incapacity Benefits to the Employment and Support Allowance. The assessment was fraught with inconsistencies and delays, largely due to mismanagement, poor performance, and problematic assessments by Atos Healthcare, the company conducting the assessments.23 Even without these challenges, PLWHAs faced difficulties in getting a fair assessment of their needs. The National AIDS Trust found that, “the barriers to work experienced by people living with HIV such as severe immune deficiency, side-effects of treatment, depression, pain and fatigue are not fully taken into account by the assessment.”24 Many PLWHAs had their sick benefits canceled, and others had their support reduced by up to GBP 36 per month.
In April 2013, the UK Government introduced a new benefit, Personal Independence Payment (PIP), to be rolled out between 2013 and 2017 in place of the Disability Living Allowance (DLA), which provides support for extra mobility and care costs related to living with a disability. While the rates under the new PIP remain the same as under the DLA, the assessment criteria is different, and therefore there are fears that the process will reassess PLWHAs at a lower rate, or remove their access to the benefit altogether.25 The National AIDS Trust (NAT) writes:
NAT believes that the PIP assessment will fail to pick up the needs of many people living with HIV. We also disagree with only focusing PIP payments on those with the most severe barriers—DLA currently has an important preventative impact for people living with HIV who have lower-level needs, which will now be lost.26
The trust notes that reassessment takes more than a year and is often conducted by private companies with little knowledge of HIV/AIDS; while PLWHAs can appeal the decision, they do not get support during the appeal processes, which leaves them vulnerable.27 While data on PLWHAs claims are not available, nearly half of all claims for PIP benefits have been refused.28
The Bedroom Tax, instituted in 2013, also negatively impacts PLWHAs on benefits, reducing assistance to those in public housing with unused bedrooms. According to an article in the Independent newspaper, 96% of affected people are paying the tax not because they refuse to downsize, but because they have not been able to find affordable smaller properties.29 For PLWHAs, who may need caregivers to stay with them when they are unwell, the Bedroom Tax does not recognize that their particular health needs mean a spare room increases their ability to draw on the support of family and friends.
Such cuts affect the ability of PLWHAs to meet their treatment and care needs. In 2013, the Terrence Higgins Trust National Hardship Fund for People with HIV/AIDS registered a 63% increase of those needing emergency help because their benefits had been stopped.30 Corrine Squire notes, in her longitudinal research, that many PLWHAs suffer from increased food insecurity due to the cuts.31 Doctors report having to prescribed food supplements to PLWHAs who are otherwise unable to maintain treatment regimens, as they can no longer afford the high-protein diet essential for effective treatment. One doctor is quoted in a newspaper article explaining:
Before the past three or four years, I never saw people coming in and saying they didn’t have enough money for food. Now I’ve seen several people in my clinic where the fact that they’ve had a decrease in their income, related to benefit changes, means they can’t afford regular food.32
Such challenges are exacerbated by cuts to support groups for PLWHAs. Cuts to psychosocial services correspond to increased levels of depression among PLWHAs.33 In the context of social cuts, justified in relation to austerity measures, the shift within the UK’s response to HIV/AIDS is subtle, but notable. It reflects an erosion of the previous rights-based response, justified by the need to reduce state costs.
Greece
As has been well documented, Greece was severely affected by the 2008 financial crisis. In order to mitigate its economic woes, and stay within the EU, it accepted a loan from the International Monetary Fund (IMF) and underwent substantial restructuring of public assets and systems. These included a restructuring of the public health system, which was admittedly suffering from poor management and corruption. However, the IMF conditionalities also included restrictions on public health spending, reducing it to less than 6% of GDP, down from approximately 10%.34 As a result, many hospitals had to cut their budgets by 40%, resulting in shortages of staff and medical supplies. The crisis was compounded by the increased demand for public health services as patients could no longer afford private care due to widespread economic hardship.35
Among the programs cut were harm reduction interventions, such as needle exchanges and opiate substitutes, which are proven to be the most effective way to prevent HIV infection among PWID.36 Budget cuts in 2009 and 2010 resulted in one-third of such programs being cut.37 The reduction in needle exchanges and opiate substitute programs was exacerbated by other health care cuts, which decreased access to services for PLWHAs and PWID to treat opportunistic infections, consult their doctors, and access rehabilitation services. The cancellation of harm reduction and other programs resulted in an immediate spike in HIV infections: incidence rose more than tenfold from 2009 to 2012 among PWID.38 While this increase may also be due to more people resorting to the drug and sex trade because of the recession, lack of access to clean needles and opiate substitutes is recognized as a primary contributing factor.39
In response to rising HIV infection rates, the Greek government “brought back into force a regulation on the transmission of infectious diseases that runs counter to all international guidelines on HIV testing and breaches human rights.”40 Greek authorities began arresting and forcibly testing PWID and sex workers for HIV. In 2012, women suspected of being sex workers were pulled off the streets, detained by the police, tested for HIV, and then had their details, including their HIV status, published on the internet. These women were not asked to consent to the testing and felt that they were not able to refuse.41 Thirty of those found to be HIV-positive were jailed for causing intentional harm to clients.
In 2012, the Greek Ombudsman reported complaints related to the sharing of confidential medical records, the refusal of housing or employment based on HIV status, and the testing and communicating of HIV status without consent. Some employers were reportedly forcing employees to get tested for HIV prior to taking up jobs.42 In 2014 and 2015, Human Rights Watch documented police harassment of PWID and sex workers, quoting one methadone recipient: “Wherever you’re coming from, wherever you’re going, without any grounds, and without provoking anyone, you are always, always going to be taken to the police station.” 43 Human Rights Watch also found, “Twenty-one people described situations in which police stops had a direct or indirect negative impact on their right to health, including interfering with their access to a doctor and necessary medication, as well as to services and information on HIV prevention, methadone, and other prescription drugs.”44 Greek authorities were restricting access to health care for vulnerable groups, violating General Comment 14 of the International Covenant on Social, Economic and Cultural Rights (ICESCR), which includes the entitlement to “a system of health protection providing equality of opportunity for everyone to enjoy the highest attainable level of health” and the freedom of “the right to be free from non-consensual medical treatment . . .and to be free from degrading treatment or punishment.”45
Managing HIV/AIDS within the EU
The right to health is recognized by the European Convention for the Protection of Human Rights and Fundamental Freedoms of the Council of Europe, and the European Social Charter. In the EU, the Charter of Fundamental Rights sets out the right of everyone to access preventive health care and to benefit from medical treatment. While health governance falls under state jurisdiction, these delineations indicate an element of regional oversight to ensure the right to health. However, the European Parliament has more often taken a risk management approach, which frames health and related issues as isolated problems to be contained. In order to demonstrate the dominance of this approach this section focuses on two key population groups: migrants and sex workers.
Migrants
The designation of migrants as a key population affected by HIV/AIDS is unique to Europe. Approximately 43% of all heterosexually transmitted HIV infections reported in Western Europe in 2006 occurred among immigrants from high-prevalence countries, such as those in sub-Saharan Africa.46 It is assumed, though hard to prove, that most of these infections occur in the country of origin, though higher prevalence among migrants may also be due to vulnerability upon arrival in the EU, resulting in the exchange of sex for food, shelter, or money. Migrants are also less likely to use health services, and are more at risk of other sexually transmitted infections and sexual violence than the general population, all of which increases their vulnerability to HIV.47
In 2005, the European Court of Human Rights stated that social benefits such as health services are a property right, irrespective of work or other contributions, and that denying health care to irregular migrants may breach the right to be free from inhumane and degrading treatment.48 Health remains a national competency, however, and each member state implements individual policies related to migrants’ access to health care. Several states only allow migrants to access health care for emergencies and core benefits. Since each member state defines these terms differently, migrants who move within the EU are often unaware of what health services they can access. In some states, migrants’ access to health care has decreased with austerity measures, and due to assumptions that providing quality care will encourage migration and therefore increase costs. For example, the UK removed HIV treatment from its emergency care list in 2009, abandoning free treatment for migrants.49 Keygnaert et al. write, “While the rights-based approach of health seems to gain some momentum in international and regional frameworks, EU member states face a hiatus between these requirements and their own migration policies.”50
The EU has neglected to address contradictory approaches to HIV/AIDS treatment and the health rights of migrants, based on the argument that health is a national competence. The European Commission stated that sexual and reproductive health rights remained primarily a national competence and that the EU had no vocation to take the lead.51 In fact, the EU has taken few actions on sexual and reproductive health in general, likely due to the highly political and culturally sensitive nature of such health issues. Migration is an even more highly politicized issue, and linking it to a health condition that attracts stigma and discrimination could potentially be problematic. As Richard Coker writes: “In Europe migration policy is a politically flammable issue; HIV could cause it to combust.”52 The intersection of migration, sex, and disease means that asserting the rights of migrants to HIV prevention and treatment services has few political benefits and many pitfalls. As a result, instead of recognizing and addressing the linkages between the social vulnerabilities migrants face, barriers to access to health care, and high HIV/AIDS prevalence among this population, the European Parliament has continued to address health, migration, and related issues as separate problems. In the process, the health rights of migrants are obscured within the political discourse.
Sex workers
Migrant sex workers face particular barriers because of differing legal approaches to sex work in the EU. In many countries, such as Greece, sex workers who fear legal prosecution avoid health centers. Some countries (Austria, Hungary, and Latvia) continue mandatory HIV testing of sex workers, which violates patients’ rights to voluntary testing.53 In the interest of promoting a uniform approach to managing sex work, European Parliament voted in February 2014 to support the Nordic model throughout the union. Already implemented in Sweden, Norway, and Iceland, this approach criminalizes buying sex and benefiting from the profits of sex work, but does not criminalize selling sex. The argument is that it criminalizes clients and not workers, but sex worker organizations and HIV/AIDS activists generally condemn this model as contradicting a rights-based approach to sex work and HIV/AIDS. Because the Nordic model prohibits buying sex, workers are isolated to obscure locations where their clients are not at risk of getting caught. In such places, sex workers are less able to screen potentially dangerous clients, such as those who do not want to use condoms or who are violent. Clients are also unlikely to report abuse they may witness in brothels for fear of prosecution. Workers cannot employ bodyguards to protect themselves from unprotected and violent sex, since the Nordic model prohibits benefiting from the income of sex workers.54 One advocate notes,
We have seen so much evidence that the control sex workers have over their working conditions, including protecting themselves from HIV, has a huge impact on their health, and the adoption of Nordic policies in driving this wedge between sex workers and health care.55
Neither WHO nor UNAIDS supports the Nordic model, instead advocating for decriminalizing both buying and selling sex as the most effective way to ensure sex workers’ right to health and to prevent the spread of HIV/AIDS. Similarly, Amnesty International declared its support for decriminalization of sex work in 2015.56
In 2014, a coalition of 450 civil society organizations and 45 researchers protested the European Parliament’s decision to promote the Nordic model.57 It is too early to know exactly how the support for the Nordic model may affect sex workers, but it demonstrates a shift away from a right-based response toward strategies that isolate sex workers.58
The treatment of key populations (those groups most at risk and affected by HIV/AIDS) within the EU is a key component to advancing a rights-based response. However, policy choices demonstrate a preference for containing the epidemic among vulnerable groups, as opposed to addressing their particular needs, which require recognizing the social determinants of health. As one key informant notes:
Europe is really doing what we call “managing AIDS.” Not ending AIDS, but managing AIDS. It is being very complacent about it; there are still many people living with HIV in Europe and you are still seeing new instances there, but since the epidemic is restricted to the key populations, nobody really thinks about it.59
Europe’s role in the global response
Since the European Commission’s Action on AIDS, TB and Malaria ended in 2011, global health policies have backtracked on human rights commitments, which is in particular contrast with increasing support for intellectual property rights that restrict access to medicines.
From HIV/AIDS to global health to inaction
When the EU’s HIV/AIDS Programme ended in 2011, it was not renewed. Instead, the European Commission adopted, in 2010, a communication on the EU’s Role in Global Health, which broadened the scope from focusing only on specific diseases and provided a policy framework for the EU’s future actions in global health.60 The shift from focusing solely on HIV/AIDS to working more generally toward global health reflects broader changes in development assistance for health, such as a backlash against vertical disease-specific initiatives and calls for more integrated health system strengthening.61 It also reiterates calls from civil society and HIV/AIDS activists to expand on the gains of the HIV/AIDS response and promote a rights-based response to other health issues.62
The 2010 communication was never developed into a program, however, and has not been included in any work plans since.63 One analysis of EU global health policy developments since 2010 finds that “the European debate [on global health] seems to have fallen largely silent.”63 Similarly, a key informant from a global health institution commented, “in terms of becoming instrumental on what actually that [the global health communication] will lead to, there has been dead silence.”64 The Global Health Policy Forums are the only related development, bringing together representatives from the European Commission, non-governmental organizations, industry representatives, and international organizations to discuss global health, but have produced few outcomes.65 One of the few European Commission documents to mention global health, the Third European Health Programme 2014–2020, only refers to global health in terms of the need to control cross-border health threats and infectious diseases. This represents a retreat from an expansion of the rights-based response, back towards vertical interventions that aim to protect the EU from external threats. Meanwhile, European Commission funding for global health has fallen from US$520 million in 2010 to $400 million in 2015, with HIV/AIDS funding decreasing from US$33 million in 2010 to $13 million in 2015.66
The EU has also shifted away from its previous alliances with civil society-led human rights campaigns. The UN General Assembly held a High-Level Meeting on HIV/AIDS in June 2011. Prior to this meeting, UNAIDS and civil society organizations lobbied aggressively for stronger human rights language than in the previous UN resolutions and declarations, which had not specified rights for key populations, and had allowed cultural qualifications on the rights of women. States with a history of resisting human rights language, such as Egypt and Iran, pushed back—as did the EU delegation.67 While not against the rights language, the EU delegation did not want to introduce specific targets to the declaration, without which it would lose much of its weight.68 Civil society found it was no longer able to rely on the EU as an ally for a global rights-based response.
From human rights to property rights
The EU delegation was particularly against treatment targets. One participant recalled:
In the beginning, just the EU was pushing for language such as “substantially increasing the number of people on treatment,” “substantially decreasing the number of people on treatment and new infections,” but they didn’t want to have figures in the political declaration, and we were working on it, so we could see the track changes on a day-to-day basis.69
The EU also pushed back on language related to intellectual property law flexibilities aimed to improve access to generic medications in developing countries. The statement from the EU representative only referred to access to treatment in relation to strengthening the Medicines Patent Pool.70 This contrasts sharply with the statement from the European Commission representative at the 2006 High-Level Plenary meeting on HIV/AIDS, which listed “affordability of new drugs, particularly through fair and tiered pricing for medicines, including the newest ones” as one of three crucial areas for future HIV/AIDS response. The changed position of European representatives was a substantial shift in EU policy, which had been previously supportive of increased access to ARVs and the ability of LMICs to access generic medications. In the end, due to extensive civil society lobbying, the EU did compromise on language related to a number of targets and intellectual property flexibilities. However, the shifting position in negotiations indicates a move away from access to medications as a human right.
The EU has continued to prioritize intellectual property rights over access to medicines in trade negotiations. In 2014, during negotiations between the EU and India, where the majority of generic HIV/AIDS medications are manufactured, the EU pushed for a data exclusivity provision that would have severely limited production of generic medications. India has refused this and other suggested provisions, but the negotiations are ongoing. For example, one proposed provision would allow EU companies to sue the Indian government for perceived threat to their profits. For example, if India overrode a medicine patent to allow for production of more affordable generic medicines (currently legal under international trade rules), a pharmaceutical company could sue the Indian government in closed-door proceedings.71 The EU is siding with pharmaceutical companies focused on profits, at the expense of those who cannot afford ARVs and will die without them.
Conclusion
While European states and institutions were once allies in campaigns to achieve the right to health, a shift is perceivable with European states cutting costs and implementing policies that threatening the health and well-being of PLWHAs and key populations. The history of the HIV/AIDS response indicates a need for bold action and controversial policies, yet politicians and policymakers are failing to develop a regional rights-based response that will address the social determinants of vulnerability for key populations. European institutions are not only reducing action on global health generally, but also retreating from previous rights-based commitments, such as those related to access to medicines. The focus within and from the EU is on containment, reducing costs, and isolating issues. The rights of those most affected are no longer prioritized. This risk management approach to the epidemic aims to control and manage HIV/AIDS, not address it or overcome its structural drivers.
While this approach is cheaper and avoids controversial issues, there are human costs. Denying PLWHAs benefits increases their risk to opportunistic infections, and reducing support services exacerbates still-prevalent stigma. While EU politicians and policymakers may prefer to ignore key populations, such as migrants, and hide others, such as sex workers, both these groups are living within the region, which purports to respect the right to health and freedom from discrimination. The EU’s reprioritization of the global response to HIV/AIDS and failure to advance its commitments to global health will impact people around the world, as will stronger intellectual property laws on pharmaceutical patents.
The history of the response to HIV/AIDS suggests that even as a short-term strategy, a risk-management approach is ineffective. The rights-based approach to health, pioneered by early European ASOs and activist groups was not only ethically sound, it was also effective in reducing HIV infection and ensuring that those affected could access care and prevent further health challenges. The tradeoff between a risk-management approach and rights-based response is perceived short-term savings and containment, versus the lasting gains of a healthier population. More importantly, the financial and political costs of a rights-based response cannot be weighed against the importance of ensuring the basic right to health to all people, as outlined in the European Convention for the Protection of Human Rights and Fundamental Freedoms.
Acknowledgments
I am grateful to the reviewers for their helpful comments and advice. This article builds on an early paper prepared for the European Community Studies Association of Canada Conference in 2014.
Julia Smith, PhD, is a Postdoctoral Fellow in the Faculty of Health Sciences at Simon Fraser University in Canada and a Research Fellow at the Health Economics and HIV/AIDS Research Division in South Africa.
Please address correspondence to the author at: Julia Smith, Blusson Hall, Room 11802, Simon Fraser University, 8888 University Drive, Burnaby, Canada, V5A 1S6. Email: Jhs6@sfu.ca.
Competing interests: None declared.
Copyright © 2016 Smith. This is an open access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/), which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original author and source are credited.
References
- S. Matic, J. Lazarus, and M. Donoghoe, HIV/AIDS in Europe. Moving from death sentence to chronic disease management. (Geneva: World Health Organization, 2006)
- See, for example, H. Legido-Quigley, L.Otero, D. Parra, et al. “Will austerity cuts dismantle the Spanish healthcare system?” British Medical Journal 346 (2014), p. f2363 and S. Arie, “Has austerity brought Europe to the brink of a health disaster?” British Medical Journal 346 (2013), p. f3773.
- I. Keygnaert, A. Guieua, G. Ooms, et al.“Sexual and reproductive health of migrants: Does the EU care?” Health Policy 114 (2014), p. 217.
- M. Power, Organized uncertainty: Designing a world of risk management. (Oxford: Oxford University Press, 2008).
- A. Taylor, “Governing the globalization of health” Law Medicine and Ethics 23/3 (2004), pp. 500-508.
- Matic et al (see note 1).
- Ibid.
- P. Söderholm, Global governance of AIDS: Partnerships with civil society (Lund: Lund University Press, 1997), p.122.
- J. Gamson, “Silence, Death and the Invisible Enemy: AIDS Activism and Social Movement ‘Newness’,” Social Problems 38 (1988), pp. 351–367.
- Matic et al (see note 1), p.15.
- Soderholm (see note 8), p.78.
- L. Gordenker, R. Coate, C. Johsson, and P. Soderholm, International cooperation in response to AIDS (London: Pinter, 1995), p.65.
- Matic et al (see note 1), p.18.
- Ibid, p.7.
- UNAIDS, Greater Involvement of People Living with HIV/AIDS Principle (Geneva: UNAIDS, 2007). Available at http://data.unaids.org/pub/BriefingNote/2007/jc1299_policy_brief_gipa.pdf.
- Global Health Institution Key Informant (Geneva: July 2013).
- Civil Society Key Informant (Brussels: December 2013); Global Health Institution Key Informant (Geneva: June 2013).
- Matic et al (see note 1), p. 2.
- WHO Dublin Declaration on Partnership to Fight HIV/AIDS in Europe and Central Asia (Geneva: World Health Organization). http://www.euro.who.int/en/health-topics/communicable-diseases/hivaids/policy/guiding-policy-documents-and-frameworks-for-whoeuropes-work-on-hiv/dublin-declaration-on-partnership-to-fighthivaids-in-europe-and-central-asia
- European Commission, Communication from the EC to the TRIPs Council on the implementation of the Doha Declaration on the TRIPs Agreement and Public (Brussels: European Commission, 2003). Available at http://trade.ec.europa.eu/doclib/docs/2004/march/tradoc_113230.pdf
- European Commission, Programme for Action to Confront HIV/AIDS, Malaria and Tuberculosis (2007-2011) (Brussels: European Commission, 2007). available at http://europa.eu/legislation_summaries/development/sectoral_development_policies/r12537_en.htm.
- E. Dugan and Z. Boren, “Exclusive: Thousands of HIV patients go hungry as benefit cuts hit,” The Independent, February 23, 2014. Available at http://www.independent.co.uk/life-style/health-and-families/health-news/exclusive-thousands-of-hiv-patients-go-hungry-as-benefit-cuts-hit-9146888.html.
- J. Kennedy, “The Department of Work and Pensions and Atos Healthcare: still failing UK’s most vulnerable,” Open Democracy (2014). Available at https://www.opendemocracy.net/ourkingdom/jennifer-kennedy/department-of-work-and-pensions-and-atos-healthcare-still-failing-uk%E2%80%99s-m
- National AIDS Trust, Employment and Support Allowance Work Capability Assessment review: Making it work for fluctuating conditions (London: National AIDS Trust, 2011).
- Dugan and Boren (See note 22)
- National AIDS Trust, Benefits. Available at http://www.nat.org.uk/HIV-in-the-UK/Key-Issues/Benefits.aspx.
- National AIDS Trust, Providing medical evidence for benefits applications: A guide for HIV clinicians (June 2014). Available at http://www.nhivna.org/documents/Publications/providing-medical-evidence-for-benefits-applications/NHIVNA_NAT_FME.pdf.
- UK Department for Works and Pensions, Personal Independence Payment: Statistical Ad Hoc (London: Department of Works and Pensions, 2015) Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/398595/pip-ad-hoc-statistics-new-claims.pdf.
- E. Dugan, “Big lie’ behind the bedroom tax: Families trapped with nowhere to move face penalty for having spare room,” The Independent, August 4 2013. Available at http://www.independent.co.uk/news/uk/politics/big-lie-behind-the-bedroom-tax-families-trapped-with-nowhere-to-move-face-penalty-for-having-spare-8745597.html
- Ibid.
- C. Squire, Living with HIV and ARVs. Three-letter lives (London: Palgrave McMillan, 2013)
- Quoted in Dugan and Boren (See note 22).
- Squire (See note 31)
- E. Simou and E. Koutsogeorgou, “Effects of the economic crisis on health and healthcare in Greece in the literature from 2009 to 2013: A systematic review,” Health Policy 115 (2014), pp. 111–119.
- M. Karanikolos, P. Mladovsky, J. Cylus, S. Thomson et al., “Financial crisis, austerity, and health in Europe,” The Lancet 381/9874 (2013), pp. 1323–1331. p.1327
- A. Ball, “HIV, injecting drug use and harm reduction: a public health response,” Addiction 102/5 (2007) pp. 684-690.
- A. Kentikelenis, M. Karanikolos, I. Papanicolas et al. “Health effects of financial crisis: omens of a Greek tragedy,” The Lancet 378, pp. 1457-1458.
- Karanikolos et al. (See note 35) p.1327
- Kentikelenis et al. (See note 37), p. 1459.
- The Lancet, “HIV testing in Greece: repeating past mistakes,” The Lancet 382/9887 (2013), p. 102.
- Ibid.
- Human Rights Watch, Greece: Police Abusing Marginalized People, May 6, 2015. Available at https://www.hrw.org/news/2015/05/06/greece-police-abusing-marginalized-people
- Ibid.
- OHCHR, The Right to Health: Fact Sheet 41. Available at http://www.ohchr.org/Documents/Publications/Factsheet31.pdf
- B. Rechel, P. Mladovsky, D. Ingleby, J. Mackenbach, and M. McKee, “Migration and health in an increasingly diverse Europe,” The Lancet 381/9873 (2013), p. 1238.
- Keygnaert et al. (see note 5) p. 218.
- European Convention of Human Rights, Article 1 and Article 8 of Protocol No. 1 (2010). Available at http://www.echr.coe.int/Documents/Convention_ENG.pdf.
- Keygnaert et al. (see note 5), p. 218.
- Ibid.
- Ibid, p. 221.
- R. Coker, “The changing nature of HIV/AIDS in Europe,” The Lancet 368/9534 (2006), p. 443.
- TAMPEP Sex Work Migration Health. (Amsterdam: 2009) http://tampep.eu/documents/Sexworkmigrationhealth_final.pdf
- S. Ka Hon Chu and R. Glass, “Sex Work Law Reform in Canada: Considering Problems with the Nordic Model,” Alberta Law Review 51 (2013), pp. 101–124.
- Civil Society Key Informant (Toronto: February 2014)
- Amnesty International, Global movement votes to adopt policy to protect human rights of sex workers, August 11, 2015. Available at https://www.amnesty.org/en/latest/news/2015/08/global-movement-votes-to-adopt-policy-to-protect-human-rights-of-sex-workers/
- ICRSE, 560 Ngos And 94 Researchers Demand Members Of European Parliament To Reject Ms Honeyball Report, February 18, 2014. Available at http://www.sexworkeurope.org/news/general-news/more-540-ngos-and-45-researchers-demand-members-european-parliament-reject-ms
- Ka Hon Chu and Glass (See note 55).
- Global Health Institution Key Informant (Geneva: July 2013). INCOMPLETE
- European Commission, Communication from the Commission to the Council, the European Parliament, the European Economic and Social Committee and the Committee of the Regions: The EU Role in Global Health. COM(2010)128 (Brussels, 2010). Available at ec.europa.eu/health/eu_world/docs/20140930_global_health_infograph_en.pdf
- J. Smith and A. Whiteside, “The History of AIDS Exceptionalism” Journal of International AIDS Society 13/47 (2010).
- G. Ooms, W. Van Damme, B. Baker, P. Zeitz and T. Schrecker, “The ‘diagonal’ approach to Global Fund financing: a cure for the broader malaise of health systems?” Globalization and Health 46:6 (2008).
- C. Aluttis, T. Krafft, and H. Brand. “Global Health in the European Union – a Review from an Agenda-Setting Perspective.” Global Health Action 7 (2014)
- Global Health Institution Key Informant (Geneva: July 2013)
- European Commission, Global Health Policy Forum (Brussels: 2015). Available at http://ec.europa.eu/health/eu_world/events/ev_20150416_en.htm
- C. Murray and J. Dieleman, Global health funding reaches new high as funding priorities shift, Institute of Health Metrics (Seattle: 2016). Available at http://www.healthdata.org/news-release/global-health-funding-reaches-new-high-funding-priorities-shift
- Global Health Institution Key Informant (Geneva: July 2013); Civil Society Key Informant (Brussels: March 2013)
- European Institution Key Informant (Brussels: November 2012).
- Global Health Institution Key Informant (Geneva: July 2013).
- EU Statement, United Nations HIV/AIDS High Level Meeting – 8-10 June 2011. Available at http://www.un.org/en/ga/aidsmeeting2011/pdf/eu.pdf
- Medicins Sans Frontieres, “Europe pressures India to trade deal that will harm access to medicines” (March 2013). Available at http://www.msf.ca/en/article/europe-pressures-india-trade-deal-will-harm-access-medicines