Siri Gloppen
Health and Human Rights 10/2
Published December 2008
Abstract
This article offers a framework for exploring litigation as a strategy to advance the right to health by holding governments accountable to human rights norms. Since the 1990s, cases in which people go to court to claim their right to health have increased dramatically in resource-poor countries. With issues ranging from access to health services and medication, to discriminatory labor practices, to public health, to the basic determinants of health (such as food, water, shelter, and a healthy environment), these cases potentially have huge financial and social implications. Little is known, however, about the success of such attempts to hold governments accountable for their obligations with respect to the right to health — or about who benefits. Is litigation primarily used by marginalized persons to gain fair access to medical services, or is it more often a means by which those patients with more financial resources or creativity in seeking assistance pursue access to treatment that is not otherwise provided due to expense? To what extent does litigation affect health policy and service delivery? What little is known about these cases is fragmented and anecdotal. The theoretical framework outlined here facilitates the systematic comparative and interdisciplinary studies needed to advance knowledge in this field, taking account of the entire litigation and implementation process.
Introduction: The global spread of health rights litigation
States commit to respect, protect, and fulfill the right to health in their constitutions and laws, through acceding to international treaties and other international instruments as part of their human rights obligations under international law.1 What is the potential of litigation to advance the human right to health by holding governments accountable to these obligations? This article argues that such potential is not sufficiently understood, and offers a theoretical framework and tentative methodology for systematic comparative and interdisciplinary studies of health rights litigation. The framework offered here was developed as part of a research program that was undertaken by a multidisciplinary group of researchers in law, medicine, political science, economics, anthropology, and ethics, with the support of several partner institutions.2
Our starting point is the global spread of court cases that seek to advance the right to health. Since the 1990s, the number of such cases has increased dramatically, and this is also true in middle- and low-income countries. These cases have focused on a wide range of issues, including access to health services and medication; discriminatory labor practices; various aspects of public health; and the basic determinants of health, such as food, water, shelter, and a healthy environment.3 Court decisions have been wide-ranging as well: throughout Latin America, in particular, courts have ordered governments and public authorities to provide treatment for a range of conditions and to include new groups of patients in existing schemes.4 In Costa Rica and Colombia (where court access is particularly easy), in Brazil, and increasingly in Argentina, judges have heard thousands of cases brought by individuals claiming that their right to health has been violated.5 In Colombia alone, the annual number of health rights cases reached 90,000 in 2007.6 We also find significant health litigation in other regions. Common law countries generally have had fewer cases, but for many years India, in particular, has experienced much health-related public interest litigation, including cases concerning reproductive rights and the right to a healthy environment.7 On the African continent, South Africa has the most sophisticated health rights jurisprudence.8
Globally, many countries have made landmark decisions relating to the human rights concerns of people living with HIV/AIDS, such as access to treatment, HIV-related discrimination, HIV prevention, and medical care for prisoners living with HIV/AIDS.9 A study of litigation about access to essential medicines found such cases in 12 low- and middle-income countries.10 Courts have also ordered enforcement of environmental standards and policies to provide safe water and housing to disadvantaged groups, and they have heard cases regarding corruption in the public health sector.
While there seems to be a clear trend toward more court cases — some brought by individuals with a specific health problem, others by activists (sometimes backed by international organizations and donors) seeking to hold governments accountable for health rights obligations — we have limited knowledge about the rate of success, the effects on health systems and policies, or the economic and social implications of these cases. The economic and social implications also depend on the social composition of the litigants, or those on behalf of which the litigation is undertaken. Is litigation an avenue used primarily by (or on behalf of) marginalized people to gain fair access to medical services? Is it more often a means used by, or benefiting, patients who have greater resources (financial and other) and who now seek to obtain access to treatment that would not otherwise be provided for financial reasons? Or are such cases used to further the interests of pharmaceutical companies or others with powerful commercial interests?
Litigation as an accountability strategy
Despite increasing instances of such court cases, affirming rights at the formal level does not necessarily bring changes on the ground. To realistically assess the accountability potential of health rights litigation, we need to know to what extent the judgments are accepted and implemented and under what circumstances litigation brings changes to health systems and policies.
This article suggests a multi-step analysis to assess to what extent litigation has succeeded in securing the specific claims of the litigants. In order to evaluate the potential of litigation as a strategy to advance the right to health in society as a whole, we have created a framework to address the systemic impact of health litigation efforts, taking into account who benefits. We start by looking at what accountability means in the context of the right to health and how litigation strategies may operate to secure it, before addressing the circumstances under which efforts to pursue health rights through litigation are likely to succeed.
What is accountability for the human right to health — and how might litigation help secure it?
A person or institution entrusted with power and resources normally has an obligation to be accountable — that is, an obligation to justify that the power and resources are used in accordance with the rules and the interests of the owners — or face penalties. Transparency, answerability (the obligation to provide answers and justify actions), and controllability (the potential application of sanctions if the performance or justifications are found lacking) are fundamental elements of accountability relations.11 Governments’ accountability for the right to health stems from the understanding that they hold power in trust on behalf of the people and that their mandate includes an obligation to respect, protect, and fulfill the right to health. Failure to act in accordance with these obligations may, in a democracy, result in electorates replacing their governments. Elections are the ultimate democratic accountability mechanism, but are weak in the sense that they are infrequent — usually every four or five years — and are “blunt,” that is, because a multitude of issues are involved simultaneously, it is difficult to interpret the signals from the electorate with regard to a specific policy area, such as health. In most states, we find that the electoral process is complemented by an array of institutions that are geared toward checking misuse of power and influencing government policy on an ongoing basis. Some are formal and mandated to hold the government to account in terms of its legal obligations (for example, courts, Ombuds offices, and human rights commissions). Other mechanisms are informal and influence policy on the basis of social interests (for example, media pressure, opinion polls, advocacy, and other forms of social activism).12 Despite its potential as an accountability mechanism, litigation is not designed primarily to hold governments accountable. Claims are normally motivated by concrete health concerns that need to be remedied, and litigation provides an avenue for rights-holders to access treatment when the system is not delivering.
The right to health: Legal basis and material content
The commencement of litigation normally requires an allegation that a legal rule or right has been violated; it is not sufficient to claim merely that an important social good has been neglected by the government. To operate as a mechanism to advance the right to health, litigation requires a legal basis for health rights claims. The nature of the legal framework varies from country to country. The basis for litigation is clearest where explicit health rights are laid down in the national constitution and legislation, or where regional and global treaties recognizing the right to health are incorporated in domestic law. In the latter case, litigation may serve an accountability function vis-à-vis national governments, not only before the national courts, but also before intergovernmental bodies, such as the European Court of Human Rights or the Inter-American Court. Even without an explicit recognition of a right to health, litigation may succeed, either by inferring this from other rights (such as the right to life) or by relying on human rights instruments in international law.13
According to Article 25 of the Universal Declaration of Human Rights, “[e]veryone has the right to a standard of living adequate for the health and well-being of himself and of his family, including food, clothing, housing and medical care and necessary social services;” and Article 12 of the International Covenant on Economic, Social and Cultural Rights (ICESCR) states that parties recognize “the right of everyone to the enjoyment of the highest attainable standard of physical and mental health.”14 The material content of the right to health was vague, however, until the Committee on Economic, Social and Cultural Rights issued its General Comment 14 in May 2000, providing an authoritative interpretation of Article 12 in terms of states’ obligations — that is, what constitutes violations of the right to health and what implementation requires.15
The right to health is not a right to be healthy but should, rather, be understood in terms of a set of freedoms and entitlements:
[T]he right to control one’s health and body, including sexual and reproductive freedom, and the right to be free from interference, such as the right to be free from torture, non-consensual medical treatment and experimentation . . . the right to a system of health protection which provides equality of opportunity for people to enjoy the highest attainable level of health.16
Thus understood, the right to health depends on other rights — to food, housing, work, education, human dignity, life, non-discrimination, equality, the prohibition against torture, privacy, access to information, and the freedoms of association, assembly, and movement.17 Acknowledging resource constraints, the ICESCR provides for “progressive realization” of rights, but the Committee maintains that states, nevertheless, have immediate obligations, including taking “deliberate, concrete and targeted” steps toward the full realization of each right and ensuring that they are exercised without discrimination; states also have a “core obligation to ensure the satisfaction of, at the very least, minimum essential levels of each of the rights . . . including essential primary health care.”18 For current purposes, this interpretation delineates the substantive content of the governments’ obligations to the right to health, and our concern is the potential of litigation to secure accountability for these obligations.
Who should be held accountable for the right to health — and to whom do they owe accountability?
Our concern is the accountability of public authorities who are responsible for health-related services. This includes policy-making and administrative institutions at various levels and public (semi-) autonomous bodies responsible for health care delivery and insurance. Non-state actors (including employers, industry, pharmaceutical companies, medical facilities, practitioners, insurance providers, and donor institutions) also have obligations relating to the right to health — and they do face court cases — but they fall outside our present focus. However, governments’ obligations do include the proper regulation of the activities of private actors, with the view to protect the rights of the people, including their right to health.
States’ domestic responsibility for the human right to health extends not only to citizens but also to all persons in their territory, including asylum seekers and undocumented immigrants. States are obliged to give particular attention to vulnerable or marginalized groups, such as prisoners and minorities.19 States also have international obligations under the ICESCR to take steps toward realizing the right to health through international assistance and cooperation, but this, too, falls outside our current focus.20
How can litigation contribute?
Litigation can contribute toward holding governments accountable with respect to both “policy gaps” and “implementation gaps.”21 Policy gaps are discrepancies between states’ legal obligations under international law and national constitutions, and laws to respect, protect, and fulfill the right to health of their populations. Litigation may play a role in bridging these gaps and in bringing national health laws and policies in line with the health rights obligations created by human rights norms. Implementation or enforcement gaps are discrepancies between stated policy and implemented policy. Health rights litigation may serve to hold governments accountable to their laws and policies and aid implementation by empowering individuals and groups to enforce the laws more directly.
This does not mean that litigation is the best approach to advance the right to health in a society — nor that it necessarily contributes positively. The criticism voiced against court-centric approaches to health rights and, more generally, against litigation as a means to effect social change, should be taken seriously. One concern is that it may increase inequalities. Research indicates, for example, that poor people are less likely to litigate and that “the haves” tend to come out ahead in court.22 In addition, in the absence of sustained mobilization, pro-health rights rulings may be poorly implemented and lack effect.23 Even when disadvantaged groups succeed, litigation, due to its casuistic nature, is prone to privilege some groups over others, and thus reinforce inequalities. The casuistic nature of litigation also gives rise to another concern, namely that litigation may undermine long-term planning and rational priority setting in health policy, and that this, while strengthening the individual right to health of parts of the population, may weaken the overall justice of the system and the collective right to health.24 Related concerns regard the limited democratic legitimacy and technical competence of judges to decide on issues that can be both technically difficult and politically divisive. Furthermore, excessive judicialization of health policy (and social policy generally) may, it is feared, threaten democratic control and weaken the democratic institutions by rendering them irrelevant in core political matters. The judiciary itself may also be weakened if these cases crowd out other forms of judicial activity, create huge backlogs, or politicize the courts in ways that undermine their legitimacy.25 We will not go further into these debates, but it is important to bear in mind that the benevolence of litigation should not be taken for granted, and that the impact of litigation on government accountability on the right to health is an empirical question — which is why a framework for comparative analysis is needed.
Assessing the success of health rights litigation
To know more about consequences of health rights litigation under different circumstances is also important from the perspective of health sector reform, both for better utilization of its constructive potential and for “defensive purposes.” Health rights litigation takes place, and increasingly so, in resource-poor countries and is likely to have significant implications for policy and spending. This trend may be positive from the perspective of the human right to health but, as noted above, it could also challenge systematic priority setting and equity and raises difficult ethical issues.
The analytical framework presented in the following section is aimed at understanding what enables litigation to succeed in securing accountability for the right to health. But first we must consider what is meant by “success” in this context.
Success in litigation can be evaluated from three different perspectives: success in court; success in the material sense; and success in the social sense. Victory in court represents the immediate criterion of success. If the litigant(s)’ claims are affirmed by the court and remedies are provided, the litigation, as such, has succeeded. But success in this narrow sense does not necessarily imply changes on the ground.Success in the material sense concerns the extent to which litigation improves the situation of the litigants (or those on behalf of which litigation is undertaken), with regard to the health condition in question. This criterion for success requires that we take into account the adequacy of the court’s orders as well as their implementation. Beyond its implications for litigants, litigation may also influence the right to health of other groups in society. Thus, the third criterion for evaluating the success of litigation is success in the social sense. To assess this, it is necessary to look at whether litigation changes policies and implementation in ways that make the health system more equitable and benefit members of society whose right to health is most at risk, or, instead, has the effect of skewing health spending in favor of already privileged patient groups and sectors of society.
Successful litigation, in the narrow sense of winning in court, is no guarantee of success in the material sense, of improving the litigants’ health conditions. Successful litigation may not even be conducive to success in the social sense, improving the health rights of the population in general and the most vulnerable, in particular.26 On the other hand, even if the case is lost in court, litigation may be successful in a broader sense of contributing materially toward the right to health of the litigants, or in society more broadly. Litigation may provide an effective focal point for social mobilization and give impetus to advocacy and policy processes regardless of the success of the case in court.27
The remainder of this paper outlines a framework for analysis in the context of this background. Such a framework may serve as a basis for systematic comparative studies of litigation aiming to secure the right to health.
Accountability for the right to health through litigation: A framework for analysis28
Studies of health litigation generally focus on judgments and court proceedings. While important, these investigations are not sufficient to understand when and how litigation functions as a mechanism to secure governments’ accountability for the right to health. We also need to understand why health cases come to the courts in some circumstances and not in others, and what happens (or not) once a judgment is passed.
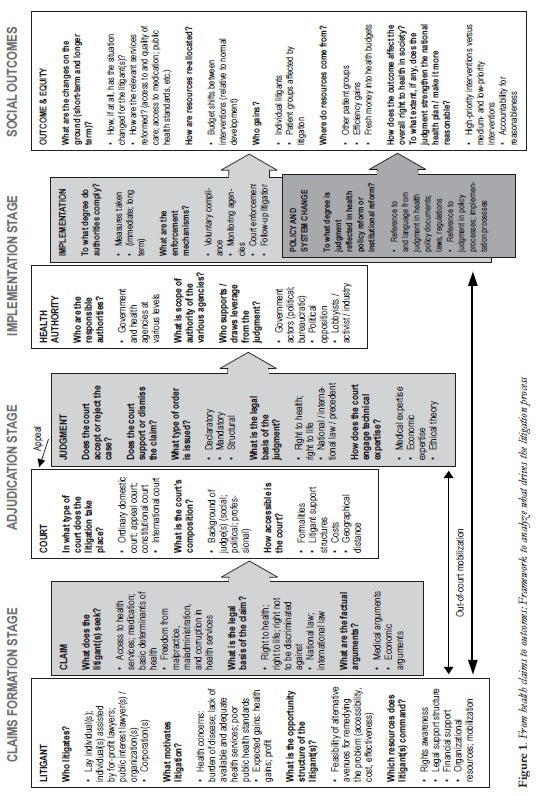
For analytical purposes, the litigation process should be conceived as four distinct but interrelated stages indicated in Figure 1 (see below). At the claims formation stage, the aim of the analysis is to understand the “input dynamics” influencing whether or not health rights claims come to the courts. At the adjudication stage, the aim is to explain why courts differ in their “output,” uncovering factors that influence how judges deal with health rights claims in their jurisprudence. At the implementation stage, the analysis seeks to understand government agencies’ responses to health rights judgments — what determines the extent to which relevant authorities comply with court orders, and whether the holding of a judgment is carried into legislation and policies. At the social outcome stage, the aim is to understand how litigation has affected the overall conditions in society with regard to the right to health. The analytical framework as it is outlined below discusses each stage separately. The four stages are named across the top of Figure 1, and the discussion of each stage corresponds to the text within the rectangular box or boxes immediately below its title.
The shaded boxes with arrows in Figure 1 indicate that the outcome of each stage of the litigation process is important for the next phase, while the slim, black arrows demonstrate that the litigation process also includes certain feedback loops. Out-of-court mobilization may influence adjudication and implementation processes. Claims may be triggered by social outcomes and implementation gaps, and they may be influenced by previous adjudication. The arrows also demonstrate that, since litigation is an iterative process — where the same case is taken to different courts on appeal and courts repeatedly hear similar cases — adjudication is influenced by earlier decisions (as well as by their political fate and social influence). As noted earlier, stages may be bypassed, as failed litigation may influence policy and social outcomes.
The rectangular boxes in Figure 1 identify key focal points and research questions that are important in uncovering the dynamics that drive litigation processes and that determine their outcome. Most questions are followed by bulleted lists that identify variables considered important in shaping the outcome. These are factors that differ between cases, across (and within) countries, and over time, and that are considered important to explain observed variation in health rights litigation and its effectiveness as an accountability mechanism. The variables indicate, in other words, where to look for answers to the research question. As Figure 1 indicates, each stage of the litigation process involves complex interactions between different actors and institutions; to adequately understand the processes requires a multidisciplinary analysis, drawing on legal and socio-legal analysis, political economy, and policy analysis, medical, and epidemiological knowledge, health economics and health systems analysis, as well as ethical analysis.
The general logic of the theoretical framework is applicable to analysis of all forms of social rights litigation.29 However, health rights litigation is special in ways that have implications for how it should be analyzed. The right to health is a particularly difficult right to pin down, both conceptually and practically, requiring special attention as to how judges and others engage various forms of expert knowledge. Health needs, and subsequent health rights claims, are inherently expansive; needs depend closely on what is possible to treat, the frontiers of which are ever-expanding. Hence the potential financial implications of granting health rights are enormous, placing increased pressure on enlarging budgets to an extent that is not generally the case for other social rights. This renders economic considerations more urgent (for the actors and in our analysis) and creates complex political dynamics that need to be understood. The political dynamics are further complicated by the fact that the right to health concerns life and death in very direct ways and is a particularly difficult ethical and moral terrain to navigate. Due to the technical nature of the field and the enormous economic interests involved, asymmetries of knowledge and power are particularly great when it comes to health and health litigation, and the analysis needs to take them into account and consider their implications. This includes giving consideration as to how international actors (such as pharmaceutical companies, donors, and NGOs) influence litigation processes.
Claims formation
Litigation cannot function as a mechanism to hold governments accountable for the right to health unless appropriate claims come before the courts, and the first stage of the analytical framework identifies conditions under which health rights claims arise.30
Activists may bring cases to advance governments’ accountability for their health rights obligations, but as noted earlier, this is rarely the direct motivation. Typically the impetus is the desire of a particular patient (or patient group) to remedy a concrete problem, or litigation may be driven by commercial interests. Accountability for the right to health may be strengthened as a by-product, but the material content of the accountability relationship depends on who litigates and the nature of their claims. What matters from an accountability perspective is thus not only the volume of health rights cases, but also the nature and composition of the caseload. As indicated in the first pair of rectangular boxes to the left in Figure 1, an effective framework to analyze claims formation must distinguish between the litigants and theirclaims. With regard to the litigants, the central questions that need to be clarified concern who the litigants are (lay individuals or professionals, activists or corporations); what motivates their claim; why they decide to take it to court; and what recourses enable them to do so.
What people claim is a function of what they need, but also of what they expect to gain through the litigation process.31 The analysis should take account of the health system (what is provided to whom and on what terms, and whether the system delivers to rights-holders) as well as the disease burden in society.
A central assumption is that the volume and nature of litigation depends on the opportunity structure faced by those with a health concern, whether a need of their own or a public health problem.32 The opportunity structure consists of the set of possible avenues for remedying the problem, including mechanisms internal to the health system; political mobilization; media pressure; Ombuds offices — and the courts. Choice of strategy depends on their relative availability, accessibility, cost, perceived effectiveness, and normative acceptability. People and organizations are assumed to pursue litigation when doing so is seen as the most promising route, given their available resources and the barriers that they face.33 All things being equal, health litigation is thus more likely where alternative avenues are closed, costly, or weak; and where access to a court is easy. A vital factor here is the legal opportunity structure, that is, the barriers and opportunities that a particular legal system presents to people with a health concern.34 The various aspects that determine the threshold of entry into the legal system are discussed further below in relation to the adjudication stage, but the accessibility of the court system is also relevant to claims formation in that they play into decisions regarding whether to litigate or not.
Particularly where the threshold is high, it is important to consider potential litigants’ ability to access resources that would enable them to bring claims to court. These include rights awareness; organizational strength and ability to mobilize; and access to legal assistance, technical expertise, and financial resources. If, as a practical matter, litigation is open only to the rich or to wealthy organizations and professional litigators, we may expect the accountability function of this litigation to differ from situations where the bulk of cases come from individuals or groups with fewer resources. Health rights litigation by professional institutions (pro bono lawyers or legal aid institutions) may form part of a “mobilization from below” by individuals or groups whose rights are violated. In other cases, the impetus comes from above, from international organizations with a long-term engagement in health rights, for whom the individual case is incidental. The latter may still be well served, but a growing involvement by international organizations in domestic health litigation requires attention to how this affects the volume and nature of cases (and the later stages of the litigation process). Lastly, the huge commercial interests operating in this field should not be overlooked. For example, in cases relating to inclusion of new drugs in public health schemes, the pharmaceutical industry has a clear interest.35 Direct involvement may be difficult to trace, but efforts should be made to shed light on possible links, as it may have a strong bearing on what comes before the courts, and drive litigation that, if successful, has vast financial implications.
Answering the question, “who litigates?” is key to understanding what drives health cases to the courts; but equally important from the perspective of accountability is what the litigant requests. The second analytical focus is the content of the claims and its relationship to the right to health. The first task is to determine what qualifies a claim as one that seeks to hold the government accountable for its obligations regarding the right to health. Both at the conceptual and practical levels the demarcation is challenging — for instance, regarding what should be included as basic determinants of health (such as environmental issues, food, water, housing, education); to what extent discrimination and malpractice cases should be included; and whether to include claims that seek to address corruption. These decisions are consequential for the remaining analysis and also have implications for the analytical framework. Different types of claims play out differently both in terms of adjudication and implementation, and may require attention to different variables. In the following discussion, the analytical framework is specified with a view to claims related to access to health services and medication.36
Once the demarcation of the claim is established, the analysis of the claim requires clarifying the legal basis for the litigation, that is, the rights on which the claim is based and the legal sources that are cited in their support. Is the argument “transnational” in the sense that it cites international human rights norms or precedents from other jurisdictions? Does it engage technical expertise (medical evidence, economic arguments, legal and ethical theory)? The analysis should be undertaken with a view to distinguish winning cases from those lost in court.
One objective of this analysis is to understand what distinguishes winning cases, and this distinction should also be seen in terms of the resources — legal and otherwise — that enable litigants to effectively argue their case. Access to (high quality) legal expertise, nationally or internationally, is important for the power of litigants’ voices. Where courts allow arguments from experts who are not party to the case (amicus curiae briefs), this may serve a similar function. The analysis should also consider the extra-legal resources of litigants, particularly in terms of out-of-court mobilization (such as demonstrations, media pressure), as “winning in the streets” may be important both for winning in court and for influencing policy impact and implementation.37
Claims should also be placed within the social context, considering the disease burden in the society as well as the health infrastructure and resources. Whether what is claimed can be considered high-priority treatment in the circumstances is important in order to analyze the social impact of litigation, as we shall see below.
Adjudication
Whether litigation is useful for securing the right to health depends on the outcome of the judicial process. The second stage of the analytical framework, adjudication, regards what happens in court. It aims to uncover factors influencing how judges deal with health rights claims and hence why courts differ in their “output.” This depends on the strength of the litigants’ voices, or how the case is argued (as represented by the arrow in the “claim” box), but also on the responsiveness and capability of the judges. As the “adjudication stage” section of Figure 1 indicates, an effective adjudication framework must distinguish between characteristics of the court itself and the way in which the judges deal with the litigants’ claims in their judgments.
The first hurdle of the adjudication process is to have the case accepted. The analysis aims to understand what makes some courts more accessible than others, and why some courts are responsive and willing to accept health rights claims, while others reject them as political matters outside their domain or dispose with them on narrow technical grounds. The second purpose of the analysis of the adjudication stage is to explain the observed differences in how courts solve the cases that they do accept.
With regard to the court, the analytic framework focuses on three aspects that there is reason to believe are particularly relevant to explain what makes some courts more responsible and accommodating to health rights claims. The first aspect is related to the nature of the court and its place in the court system. Do national courts differ from international judicial bodies, such as the Inter-American Court? Are special constitutional courts more likely to issue landmark health rights judgments? Are there differences between courts operating in civil and common law legal systems? The second aspect is related to the composition of the court and the background and competence of the judges, which is assumed to influence both the level of judicial independence and the responsiveness to health rights claims. The third aspect is that referred to above as the legal opportunity structure ¾ the barriers and opportunities that the legal system presents to litigants. The threshold of entry into the legal system is a key factor in this analysis and depends on rules of standing, procedural requirements, and costs. It also depends on whether litigants are responsible for presenting arguments and preparing evidence or are aided by the court itself.38
The second focal point in the analysis of the adjudication stage of the litigation process is on the output produced by the court. This is represented by the “judgment” box in Figure 1. How judges deal with health rights claims varies in several dimensions: whether the cases are accepted as within the courts’ jurisdiction; whether the judges uphold the claims; and which remedies they provide for in their orders. Judgments in health rights cases range from declaratory orders, where courts affirm the claim without issuing further directions; to mandatory orders, where specific remedies are authorized; to supervisory orders, those that require parties to report back within set time-frames. Increasingly, courts also develop “structural judgments,” in which they order authorities to initiate a process to develop new legislation, policies, and plans to remedy a rights violation within parameters set by the judges. As shown by the Colombian Constitutional Court’s recent landmark judgment, which goes far in ordering the health system to be restructured, orders may relate to the nature of the process as well as the outcome.39
The analysis of the substance of the judgments should also examine the legal sources and evidence that the judges rely on. Given the complex technical and ethical nature of many health cases and their economic implications, particular attention should be paid to how judgments engage relevant expertise and to what extent the impetus to do so comes from the court itself or from the arguments presented. Similarly, it is important to understand how external legal influence affects domestic health judgments. As noted earlier, this is a field with considerable transnational engagement, and the analysis should look for patterns of norm diffusion and inter-legality, where judgments combine and hybridize various sets of norms.40
The outcome of the analysis at this stage determines the success of litigation in the narrow sense. Where the judgment supports the claimants against the public authority, litigants have succeeded, in a formal sense, in holding the government accountable for health rights obligations. To what extent they can also reap material benefits from their victory depends on how the judgment is implemented.
Implementation
What happens after the court has handed down its decision depends in part on the judgment itself. As noted above, courts have a range of orders that are more or less restrictive vis-à-vis the government with regard to what should be done and when. All else being equal, detailed and restrictive orders are more likely to be implemented. The “implementation stage” in Figure 1 indicates a range of other factors that also are assumed to influence government’s implementation of court decisions in health rights cases. Here the framework distinguishes between two forms of implementation: narrow compliance with the judgment (noted as “implementation”) and long-term implementation that is seen in terms of the systemic impact or structural change on health policies and the health system (the smaller box within “implementation” that is labeled “policy and system change”). In some cases, courts issue structural orders where policy change and system change are prescribed in the judgment itself and clearly constitute a form of implementation. In other cases, and more commonly, judgments may set in motion or contribute towards reforms without a direct court order to this effect. This is indicated in the figure by the partial overlap of the two output arrows at the implementation stage.
The variables that are presumed to influence the way in which health judgments are implemented fall into two categories. The first concerns the characteristics of the implementing authorities and agents involved (illustrated by the “health authority” box in Figure 1). The second concerns the factors that relate to the process through which they are implemented (contained in the two shaded boxes with output arrows under “implementation”).
With regard to the authorities themselves, the analysis must first clarify who they are, that is, which political and administrative bodies carry responsibility for implementing the judgment. Health policy and administration structures are often complex and it is important to identify those agencies that are responsible for implementing various aspects of the judgment, and to determine their respective scope of authority. It is also important to inquire into who has an interest in the judgment’s implementation (or in preventing it from being implemented) and in using it as a leverage to change policy. The context and nature of the case determine which processes of health policy or system change are most relevant to analyze. Variables must be specified for the concrete analysis, but in each case two sets of actors should be identified: the public authorities who are central in shaping the relevant health policies/systems, and the external actors (political opposition, activists, industry lobby, etc.) who seek to influence the process. To what extent do any of these actors “carry” the case in the sense that they make the judgment or litigation effort relevant to the litigation and policy processes? And if so, for what reason? Both actors within government and agencies involved in implementation and other political actors may use the judgment as leverage for their views and interests. So also may activists (including litigants themselves and local and international NGOs) who mobilize around the issue, as well as actors who have economic interests in the process (for example, international pharmaceutical companies, donors, and medical professionals).
To analyze the implementation process, it is important first to establish which measures have been taken to implement the judgment, and then to seek to establish why these measures have been taken — or not. One aspect of this step in the analysis framework is assessing to what extent compliance is voluntary or is a result of operative enforcement mechanisms. Voluntary compliance is assumed to be more likely when the judgment fits the authorities’ political or ideological views or interests; but compliance is also presumably influenced by the political-legal culture (i.e., with a strong culture of legalism, compliance is likely even when judgments run counter to the implementing authorities’ preferences); and by the available resources and institutional capacity of the relevant authorities.
Enforcement mechanisms include actions by courts themselves, such as when officials are charged with contempt of court for failing to implement orders, but also include actions by monitoring agencies, ad hoc commissions, Ombuds offices, and human rights commissions. The hypothesis here is that the presence and vitality of official enforcement mechanisms have a positive impact on compliance. Equally significant for consideration are unofficial “enforcement mechanisms.” These are actions by litigants or others in support of the judgment, such as follow-up litigation where implementation is lacking; monitoring and reporting; and shaming of institutions and officials through the media, demonstrations, and advocacy.
To assess the potential of litigation as a strategy to advance the right to health in society, it is necessary to go beyond an assessment of direct compliance and consider the dynamics that shape the structural impact of litigation (the “policy and system change” box in Figure 1). This analysis is fraught with more uncertainty than compliance assessments although, as noted above, the distinction between compliance and policy/system impact may be blurred in practice, particularly with structural judgments where the order is to undertake a policy process or systemic change. Changes that seem to respond to litigation may also be influenced by parallel processes and/or forces. Regardless of what happens in court, health policies and systems continuously develop in response to a variety of factors that include demographic changes; the burden of disease; technological, economic, and ideological changes; international trends; political mobilization; and advocacy. It is important to consider such potentially confounding factors in order to avoid attributing too much (or too little) to litigation. Through interviews, observation, and reviews of policy documents, the analysis should uncover how a judgment or litigation process — including prospects of future litigation — enters into the deliberations and influences health policy and practices.
The analysis of the implementation stage of the litigation process enables an assessment of the material success of litigation as a strategy to advance accountability for the right to health, but only with respect to the specific litigants or groups concerned. How health litigation affects the right to health in society more broadly (the social outcome) requires a different focus.
Social outcome
Of ultimate concern is the impact of health litigation on the ground: on the health of various parts of the population, on the quality of and access to health services, and on the basic determinants of health. This is the focus of the “social outcomes” section of the analytical framework, summarized in the “outcome & equity” box furthest to the right in Figure 1. Such impact is notoriously difficult to assess. Even more than for changes in policies and systems, possible confounding social factors make it very difficult to establish credible links. A more realistic strategy may be to identify process indicators relating to outcomes where there is reason to expect distributional effects of particular judgments or litigation processes. Budget processes may be one example, policy rollout another. What are the gains, and who benefits? If resources are re-allocated, where do they come from — and who loses? How are weak and vulnerable groups affected?
The concrete indicators and focus of analysis will depend on the context and types of health rights litigation. The following discussion focuses on budgetary implications and distribution effects among social and diagnostic groups.
Useful information may, for example, be provided through interrupted time series where budget trends are compared over time, before and after a significant judgment that is assumed to have had an impact on resource allocation (for example, a ruling ordering public provision of an expensive drug). While such an analysis may indicate a shifting of resources between interventions and patient groups, other factors may also cause budgets to change. To compare budget trends in similar countries may be useful to provide some control for “normal” budgetary developments. Expansion in some areas of the health budget is not necessarily at the expense of other budgeted areas. “Fresh money” may come from other parts of the national budget, from donors, or from efficiency gains. Similarly, an absence of changes may not mean that nothing has happened, as resources flows may be adjusted within budget categories. Examination of budget data should thus be complemented with qualitative analysis of budget processes to get a better sense of how and why the budgets change and the link to litigations. A multi-disciplinary approach is thus called for that combines economics with policy analysis.
This last step of our analytical framework examines whether health rights litigation contributes to the overall equity of the system, in the sense of strengthening the right to health in society at the collective level. As defined above, the right to health includes equitable distribution of all health facilities, goods, and services; and implementation of a national public health strategy and plan of action.41 Additionally, countries increasingly develop national health plans that seek, at least in theory, to prioritize resources in ways that are reasonable and balance the rights of various sections of the population.42
Litigation may relate to such plans in various ways. If litigation shifts resources between groups of patients (for example, by introducing new medication or interventions, or by improving access and quality of care), this could weaken — or strengthen — national health plans, depending on the reasonableness of the original plan as well as the nature of the shift. One way to appreciate this is to analyze whether the relevant interventions constitute high- or low-priority treatment under the circumstances. The classification of medical intervention into priority groups (high, medium, low, and experimental) estimates the cost (relative to GDP per capita) of quality-adjusted life years gained, and thus provides a basis for comparison.43 If litigation carries health interventions in the high-priority category, it is likely to strengthen the reasonableness of the national health plan. Support for inclusion of low-priority interventions (typically very expensive drugs or experimental treatment) is more likely to detract from the collective right to health as manifested in the national health plans by drawing resources away from high-priority care. Judgments such as the structural order of the Colombian Constitutional Court discussed above, which order a participatory process of health reform to move toward a more reasonable health system, aim to strengthen accountability for the collective right to health.44
Concluding reflections
The growth of health rights litigation indicates that it works — for some people. Our concern has been whether litigation has potential as a strategy to hold governments accountable for their obligations regarding the human right to health, not only with regard to individual claimants, but also for the population at large. To know under which conditions — legal, political, and social — litigation can advance the right to health in society generally, and for disadvantaged groups in particular, is of academic interest, but it is also important for health reform and activism.
In conclusion, this paper has argued that there exists an inadequate knowledge base for assessing the accountability potential of health rights litigation and has offered analytical tools that can remedy this by serving as a basis for systematic comparative studies. These may be broad multi-disciplinary studies analyzing selected litigation processes across the various phases, or they may be comparative studies with a more narrow focus on particular aspects of the litigation process. Such studies, based on the factors outlined here, can help us move well beyond assumptions and anecdotes to answer the questions, “to what extent does litigation succeed in obtaining its goals?” and “to what extent does it succeed in securing accountability for the human right to health?”
Siri Gloppen, PhD, is Professor in the Department of Comparative Politics, University of Bergen, and Senior Researcher at the Chr. Michelsen Institute, Bergen, Norway.
Please address correspondence to the author at CMI, P.O. Box 6033, Postterminalen, 5020 Bergen, Norway, email: siri.gloppen@cmi.no.
References
1. International treaties and other international instruments recognizing the right to health include the Universal Declaration of Human Rights (UDHR), G.A. Res. 217A (III), UN GAOR, Res. 71, UN Doc. No. A/810 (1948), Article 25. Available at http://www.un.org/Overview/rights.html; the International Covenant on Economic, Social and Cultural Rights (ICESCR), G.A. Res. 2200 (XXI), UN GAOR, 21st Sess., Supp. No. 16, at 49, UN Doc. No. A/6316 (1966), Article 12. Available at http://www.unhchr.ch/html/menu3/b/a_cescr.htm; the International Convention on the Elimination of All Forms of Discrimination against Women, G.A. Res. 34/180, UN GAOR, 34th Sess., Supp. No. 46, at 193, UN Doc. No. A/34/46 (1979), Articles 11 and 12. Available athttp://www.unhchr.ch/html/menu3/b/e1cedaw.htm; the International Convention on the Elimination of All Forms of Racial Discrimination, G.A. Res. 2106A (XX) (1965), Article 5(e)(iv). Available athttp://www.unhchr.ch/html/menu3/b/d_icerd.htm; the Convention on the Rights of the Child (CRC), G.A. Res. 44/25, UN GAOR, 44th Sess., Supp. No. 49, at 166, UN Doc. No. A/44/25 (1989), Article 24. Available at http://www.unhchr.ch/html/menu3/b/k2crc.htm; the European Social Charter, October 18, 1961, 529 U.N.T.S. 89, Article 11. Available athttp://conventions.coe.int/treaty/en/treaties/html/035.htm; the African Charter on Human and Peoples’ Rights, June 27, 1981, O.A.U. Doc. CAB/LEG/67/3 rev. 5, 21 I.L.M. 58 (1982), Article 16. Available at http://www1.umn.edu/humanrts/instree/z1afchar.htm; the Additional Protocol to the American Convention on Human Rights in the Area of Economic, Social and Cultural Rights (Protocol of San Salvador) (1988), Article 10. Available at http://www.oas.org/juridico/English/Treaties/a-52.html; and the Convention on the Rights of Persons with Disabilities (ICRPD), G.A. Res. 61/106 UN GAOR, 61st Sess. UN Doc. No A/61/611 (13 December 2006), Article 25. Available at http://www.un.org/disabilities/default.asp?navid=12&pid=150.
2. The framework has been developed as part of a research program, Right to Health through Litigation? Can Court Enforced Health Rights Improve Health Policy and Priority Setting in Poor Countries? Available at http://www.cmi.no/research/project/?1128=right-to-health-through-litigation, funded by the Norwegian Research Council and hosted by the Chr. Michelsen Institute, Bergen, Norway, and is undertaken by a multidisciplinary group of researchers (in law, medicine, political science, economics, anthropology, and ethics), and partner institutions including the Faculty of Medicine, University of Bergen; Harvard Law School’s Human Rights Program; the Centre for Advanced Legal Studies, University of the Witwatersrand; and Ain o Salish Kendra (ASK), Bangladesh. Thanks to the research group for input into the framework and this article, and to Amy Senier, Sarah Scorcer, and Mindy Roseman for literature review.
3. For a status report on health rights litigation, see P. Hunt, Report of the Special Rapporteur on the Right of Everyone to the Enjoyment of the Highest Attainable Standard of Physical and Mental Health (New York: United Nations General Assembly, 2007). Available at http://www2.essex.ac.uk/human_rights_centre/rth/docs/council.pdf.
4. Ibid. See also, A. E. Yamin, “Protecting and Promoting the Right to Health in Latin America: Selected Experiences from the Field,” Health and Human Rights: An International Journal 5/1 (2000), pp. 116–148. For health rights litigation before international tribunals, see, for example, L. Cabal, M. Roa et al., “What Role Can International Litigation Play in the Promotion and Advancement of Reproductive Rights in Latin America?” Health and Human Rights: An International Journal 7/1 (2003), pp. 50–88; and M. F. Tinta, “Justiciability of Economic, Social, and Cultural Rights in the Inter-American System of Protection of Human Rights: Beyond Traditional Paradigms and Notions,” Human Rights Quarterly 29/2 (2007), pp. 431–459. For health litigation in high-income countries, see, for example, C. M. Flood, “Just Medicare: The Role of Canadian Courts in Determining Health Care Rights and Access,” The Journal of Law, Medicine and Ethics 33/4 (2005), pp. 669–680; C. Shalev and D. Chinitz, “Joe Public v. the General Public: The Role of The Courts in Israeli Health Care Policy,” Journal of Law, Medicine and Ethics 33/4 (2005), pp. 650–659; W. E. Pamet and R. A. Danard, “The New Public Health Litigation,” Annual Review of Public Health 21 (2000), pp. 437–454. Available at http://www.ncbi.nlm.nih.gov/pubmed/10884960; and P. D. Jacobson and S. Soliman, “Litigation as Public Health Policy: Theory or Reality?” Journal of Law, Medicine and Ethics 30/2 (2002), pp. 224–238.
5. B. M. Wilson and J. C. Rodriguez Cordero, “Legal Opportunity Structures and Social Movements: The Effects of Institutional Change on Costa Rican Politics,” Comparative Political Studies 39/3 (2006), pp. 325–351. Abstract available at http://cps.sagepub.com/cgi/content/abstract/39/3/325; B. M. Wilson, “Claiming Individual Rights through a Constitutional Court: The Example of Gays in Costa Rica,” International Journal of Constitutional Law 5/2 (2007), pp. 242–257. Abstract available at http://icon.oxfordjournals.org/cgi/content/abstract/5/2/242; R. Uprimny Yepes, “The Enforcement of Social Rights by the Colombian Constitutional Court: Cases and Debates,” in R. Gargarella, P. Domingo, and T. Roux (eds), Courts and Social Transformation in New Democracies: An Institutional Voice for the Poor? (Aldershot, UK: Ashgate Publishing Limited, 2006).
6. See A. E. Yamin and O. Parra-Vera, “How do courts set health policy? The case of the Colombian Constitutional Court,” PLoS Medicine 6/2 (2009), e1000032; doi:10.1371/journal.pmed.1000032.
7. M. Desai and K. B. Mahabal, Health Care Case Law in India: A Reader (Mumbai: Centre for Enquiry into Health and Allied Themes, 2007). Available athttp://www.cehat.org/humanrights/caselaws.pdf; A. Dhanda, “The Right to Treatment of Persons with Psychosocial Disabilities and the Role of the Courts,” International Journal of Law and Psychiatry28/2 (2005), pp. 155–170; S. B. Shah, “Illuminating the Possible in the Developing World: Guaranteeing the Human Right to Health in India,” Vanderbilt Journal of Transnational Law 32/2 (1999), pp. 434–486; A. M. Sood, Litigating Reproductive Rights: Using Public Interest Litigation and International Law to Promote Gender Justice in India (New York: Center for Reproductive Rights, 2006). Available at http://www.reproductiverights.org/pub_bo_litigatingreprorights.html. Health-related cases have been litigated in neighboring countries, partly relying on Indian case law; see, for example,Dr. Mohuiddin Farooque v. Bangladesh, on the right to safe food (WP 92 of 1996, Supreme Court of Bangladesh). Available at http://www.unep.org/padelia/publications/Jud.Dec.Nat.pre.pdf, pages 37-45; On prisoners’ right to health care in Sri Lanka, see W. R. Sanjeewa AAL (for Gerald Perera) v. Sena Suraweera (Inspector) and ors. (SCFR 328/2002 [Apr. 4. 2003] Supreme Court of Sri Lanka). Available at http://www.alrc.net/doc/mainfile.php/cl_srilanka/199/.
8. A. Hassim, M. Heywood, and J. Berger, Health and Democracy (Johannesburg: Aids-Law Project). Available at http://alp.immedia.co.za/index.php?option=com_content&task=view&id=53&Itemid=4; E. C. Christiansen, “Adjudicating Non-Justiciable Rights: Socio-Economic Rights and the South African Constitutional Court,” Columbia Human Rights Law Review 38/2 (2007); D. Brand and C. H. Heyns, Socio-economic Rights in South Africa (Pretoria: PULP, 2005); World Bank, Realizing Rights through Social Guarantees: An Analysis of New Approaches to Social Policy in Latin America and South Africa, Report No. 40047 (Washington, DC: World Bank, Social Development Department, 2008). Available at http://siteresources.worldbank.org/EXTSOCIALDEVELOPMENT/; S. Gloppen, “Social Rights Litigation as Transformation: South African Perspectives,” in P. Jones and K. Stokke (eds), Democratising Development: The Politics of Socio-Economic Rights in South Africa (Leiden, The Netherlands: Brill Academic Publishers, 2005), pp. 153–180.
9. On the global spread of cases regarding HIV/AIDS, see UNAIDS, “Courting Rights: Case Studies in Litigating the Human Rights of People Living with HIV,” UNAIDS Best Practice Collection(Geneva: UNAIDS, Canadian HIV/AIDS Legal Network, 2006). Available at http://data.unaids.org/Publications/IRC-pub07/jc1189-courtingrights_en.pdf. See also, International Commission of Jurists,Courts and the Legal Enforcement of Economic, Social and Cultural Rights: Comparative Experiences of Justiciability (Geneva: ICJ, 2008). Available at http://www.ldf.ps/documentsShow.aspx?ATT_ID=703.
10. H. V. Hogerzeil, M. Samson, J. V. Casanovas and L. Rahmani-Ocora, “Is Access to Essential Medicines As Part of the Fulfilment of the Right to Health Enforceable through the Courts?” Lancet368/9532 (2006), pp. 305–311.
11. On concepts of accountability, see A. Schedler, L. Diamond, and M. F. Plattner (eds), The Self-Restraining State: Power and Accountability in New Democracies (Boulder, CO: Lynne Rienner, 1999); S. Mainwaring and C. Welna (eds), Democratic Accountability in Latin America (Oxford: Oxford University Press, 2003).
12. P. Newell and J. Wheeler (eds), Rights, Resources and the Politics of Accountability: Claiming Citizenship (London: Zed Books, 2006); S. Gloppen, R. Gargarella, and E. Skaar, Courts and Democratization. Accountability Function of Courts in New Democracies (London: Frank Cass, 2004); A. M. Goetz and R. Jenkins, Reinventing Accountability: Making Democracy Work for Human Development (Basingstoke, UK: Palgrave Macmillan, 2004).
13. In Costa Rica and India, among other countries, a right to health has been constructed from the right to life.
14. The right to health is also recognized in a number of other international instruments (see note 1).
15. Committee on Economic, Social and Cultural Rights (ESC Committee), General Comment No. 14, The Right to the Highest Attainable Standard of Health, UN Doc. E/C.12/2000/4 (2000). Available athttp://www.unhchr.ch/tbs/doc.nsf/(symbol)/E.C.12.2000.4.En.
16. Ibid., para. 8.
17. See Commission on Social Determinants of Health (CSDH), “Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health,” Commission on Social Determinants of Health — Final Report (Geneva: World Health Organization, 2008). Available at http://www.who.int/social_determinants/final_report/en/.
18. This is specified to include the right of access to health facilities, goods, and services on a non-discriminatory basis; access to the minimum essential food that is nutritionally adequate and safe; access to basic shelter, housing, sanitation, and an adequate supply of safe and potable water; access to essential drugs; equitable distribution of all health facilities, goods, and services; and implementation of a national public health strategy and plan of action. See General Comment No. 14 (see note 15, para. 43).
19. See General Comment No. 14 (see note 15), para. 34.
20. See General Comment No. 14 (see note 15), para. 38.
21. For this distinction, see T. Staer, Can the Judiciary Manage the Environment? A Case Study of Judicial Activism in India (Oslo: Masters Thesis, Center for Development and the Environment, University of Oslo, November 2006).
22. For critical analyses of the potential of law and courts to effect social change, see M. Galatner, “Why Haves Come Out Ahead: Speculations on the Limits of Social Change,”Law and Society Review9/1 (1974), pp. 95–160; G. N. Rosenberg, The Hollow Hope: Can Courts Bring about Social Change? (Chicago, IL: University of Chicago, 1991); D. A. Bell, Silent Covenants: Brown v. Board of Education and the Unfulfilled Hopes for Racial Reform (Oxford and New York: Oxford University Press, 2004).
23. See, for example, “Litigating Economic, Social and Cultural Rights: Achievements, Challenges and Strategies,” COHRE Report (Geneva: Centre on Housing Rights and Evictions Report, 2003). Available at http://www.cohre.org/store/attachments/COHRE%20Litigating%20ESC%20Rights%202003.pdf; M. R. Anderson, “Access to Justice and Legal Process: Making Legal Institutions Responsive to Poor People in LDCs,” IDS Working Paper 178 (Sussex, UK: Institute of Development Studies, 2003). Available at http://www.ntd.co.uk/idsbookshop/details.asp?id=729; C. R. Epp, The Rights Revolution: Lawyers, Activists, and Supreme Courts in Comparative Perspective (Chicago, IL: University of Chicago Press, 1998); M. Heywood, “Preventing Mother-to-Child HIV Transmission in SA: Background, Strategies and Outcomes of the TAC Case against the Minister of Health,” South African Journal on Human Rights 19/2 (2003), pp. 278–315.
24. In our interviews with health administrators and decision-makers in San Jose, Costa Rica, in June 2008, this concern was widely voiced.
25. See, for example, R. Sieder, L. Scholden, and A. Angell (eds), Judicialization of Politics in Latin America (New York: Palgrave Macmillan, 2005). See also, See also, S. Gloppen, “Courts and Social Transformation: An Analytical Framework,” in Gargarella et al. (see note 5), pp. 35–59.
26. In addition, professional public interest litigators may have interests of their own in the case (for example, long-term jurisprudential development; professional prestige; or funding) that may diverge from the interests of the litigants or influence the selection of cases. For more on this, see Gloppen (see note 8).
27. For a more detailed discussion in relation to public interest litigation generally, see S. Gloppen, “Public Interest Litigation, Social Rights, and Social Policy,” in A. A. Dani and A. deHaan (eds), Inclusive States: Social Policy and Structural Inequalities (Washington, DC: World Bank Publications, 2008) pp. 343–368. See also, Gloppen (see note 8).
28. This builds on and expands the “courts and social transformation” framework developed and applied in Gargarella et al. (see note 5); Gloppen (see notes 8 and 24, respectively); S. Gloppen and F. E. Kanyongolo, “Courts and the Poor in Malawi,” International Journal of Constitutional Law 5/2 (2007), pp. 258–293. Abstract available at http://icon.oxfordjournals.org/cgi/content/abstract/5/2/258; Staer (see note 21); A. Skjævestad, The Mapuche People’s Battle for Indigenous Land: Litigation as a Strategy to Defend Indigenous Land Rights (Bergen, Norway: Chr. Michelsen Institute, CMI WP 3, 2008). Available at http://www.cmi.no/publications/file/?3002=the-mapuche-peoples-battle-for-indigenous-land.
29. See Gloppen in Gargarella et al. (see note 25).
30. Where courts have the competence to try cases on their own initiative, they may in theory also take on cases regarding the right to health, in which case the input analysis will differ from what is set out here.
31. In terms of individual litigants, the expected gain could be either a health gain or an economic gain, if the individual would have bought the treatment anyway. The expected gain is influenced by the probability of winning the case. Here, one possible hypothesis is that the probability of winning is larger the smaller the total economic implications for public budgets (ceteres paribus). For instance, one would presume that a right to AIDS medication would be easier to secure in a country with low HIV-prevalence rates, all other factors being equal. It is implicit in this hypothesis that the right to health (normally) is not viewed as an absolute right, but rather a right that is traded off against other benefits.
32. The concept of opportunity structure was adapted from the sociology of cultural deviance to studies of political mobilization. Particular successes of social movements are often explained in terms of their political opportunity structure. See, for example, D. S. Meyer, “Protest and Political Opportunities,” Annual Review of Sociology 30 (2004), pp. 125–145.
33. Processes of claims formation are discussed in more detail in Gloppen (see notes 25 and 24, respectively).
34. On the idea of legal opportunity structure, see Wilson and Cordero (see note 5) and E. A. Andersen, Out of the Closets and into the Courts: Legal Opportunity Structure and Gay Rights Litigation (Ann Arbor, MI: University of Michigan Press, 2005).
35. Such cases are found in many countries as indicated by Hogerzeil et al. (see note 10) and constitute a significant part of the caseload in the countries where health litigation is most widespread, such as in Colombia and Costa Rica.
36. While these are paradigmatic health rights cases, they are not necessarily the most important for the right to health, and the framework should be developed to accommodate other types of litigation.
37. See Heywood (see note 23); Epp (see note 23); and Gloppen (see note 8).
38. Some courts will take “raw claims” off the street and themselves build cases. This was pioneered by the Indian Supreme Court in its “apostolic jurisdiction” and is most pronounced in Costa Rica, where the constitutional court employs around 60 laterados, lawyers who consider the merit of peoples’ amparos (protection writs) and prepare them into cases. See Gargarella et al. (see note 5) and Wilson and Rodriguez Cordero (see note 5).
39. Corte Constitucional de Colombia, Sala Segunda de Revisión, Sentencia T-760. July 2008. See discussion in Yamin and Parra Vera (see note 6).
40. This may include international law, national constitutional and statutory law from various jurisdictions, as well as religious and traditional law. For the concept of inter-legality, see B. S. Santos, Toward a New Legal Common Sense: Law, Globalization, and Emancipation (London: Butterworths, 2002).
41. See General Comment No. 14 (see note 15), para. 15.
42 . See, for example, Choices in Health Care. A Report by the Government Committee on Choices in Health Care (The Netherlands: Ministry of Welfare, Health and Cultural Affairs, 1992); Norges Offentlige Utredninger, Guidelines for Priority Setting in the Norwegian Health Care System [Norwegian] (Oslo: Universitetsforlaget, 23, 1987); Norges Offentlige Utredninger, Priority Setting Revisited [Norwegian](Oslo: Statens forvaltningstjeneste. Statens trykking, 1997); F. Honingsbaum, J. Calltorp, C. Ham, and S. Holmström, Priority Setting Processes for Healthcare in Oregon, USA; New Zealand; the Netherlands; Sweden; and the United Kingdom (Oxford: Radcliffe Medical Press, 1995); D. C. Hadorn and A.C. Holmes, “The New Zealand Priority Criteria Project, Part 1: Overview,” BMJ (British Medical Journal) 314/7074 (1997), pp. 131–134; C. M. Feek, W. McKean, L. Henneveld, G. Barrow, W. Edgar, and R. J. Paterson, “Experience with Rationing Health Care in New Zealand,” BMJ (British Medical Journal) 318 (1995), pp. 1346–1348; O. F. Norheim, “Rights to Specialized Health Care in Norway: A Normative Perspective,” Journal of Law, Medicine and Ethics 33/4 (2005), pp. 641–649; and O. F. Norheim, et al, “Adoption of New Health Care Services in Norway (1993–1997): Specialists’ Self-Assessment According to National Criteria for Priority Setting,” Health Policy 56 (2001), pp. 65–79.
43. See note 42 for examples of such analysis.
44. See S. Gruskin and N. Daniels, “Process Is the Point: Justice and Human Rights: Priority Setting and Fair Deliberative Process,” American Journal of Public Health 98 (2008), pp. 1573–1577; N. Daniels, “Accountability for Reasonableness,” BMJ (British Medical Journal) 321 (2000), pp. 1300–1301; and N. Daniels, Just Health: Meeting Health Needs Fairly (New York: Cambridge University Press, 2008). For the Colombian judgment, see Yamin and Parra Vera (see note 6).