Homer D. Venters, Jennifer McNeely, and Allen S. Keller
Health and Human Rights 11/2
Published December 2009
Abstract
The detention of immigrants in the United States is a rapidly expanding endeavor with serious health consequences for the detainees. This detainee population represents non-criminal immigrants who are detained because of a visa violation or other immigration issue but who are not charged with any crime and do not enter the criminal justice system. HIV-positive detainees are especially vulnerable to lapses in proper medical care, and press reports have highlighted deaths and adverse medical outcomes among HIV-positive detainees. We have examined reports on detainee health issues published by numerous groups and conducted our own analysis of the health plan used to govern much of the specialty care for detainees who are HIV positive. We conclude that the system of immigration detention in the US fails to adequately screen detainees for HIV and delivers a substandard level of medical care to those with HIV. We provide several specific recommendations for improving screening and medical care among this highly vulnerable population.
Introduction
Since the beginning of the HIV epidemic, correctional settings have proven to be particularly challenging venues for competent, evidence-based diagnosis and treatment of HIV/AIDS. Much has been written about the burden of responsibility to provide appropriate HIV care to criminal arrestees and prisoners and about the difficulties in doing so. HIV became widely recognized as a pressing issue in American jails and prisons by 1987; however, multiple factors slowed institutional implementation of adequate testing for and treatment of HIV within the correctional setting.1 The mid-1980s marked the beginning of the American “War on Drugs,” a policy, implemented by individual states, that dramatically altered the correctional health demographics by incarcerating large numbers of drug users and other non-violent offenders who were at high risk for contracting HIV.2 In addition, even though correctional health workers recognized the presence of HIV in jails and prisons, in many cases, the response was poor. The 1976 landmark US Supreme Court Decision (Estelle v. Gamble) guaranteeing the right of incarcerated persons to receive medical care was barely a decade old, and many states had yet to come into compliance with this ruling. 3 As jails and prisons filled with persons infected with HIV and hepatitis C in the 1990s, correctional health became the venue for much of the nation’s HIV care. For example, by 1999, HIV infection rates reached almost 7% for male prisoners and 12% for female prisoners in New York State.4 Since 1987, the Centers for Disease Control (CDC) has regularly reported on HIV concerns in prisons, as have multiple professional societies, academic researchers, and Departments of Health and Corrections.5 Such routine reporting of HIV prevalence and testing data is an essential component of addressing HIV in any incarcerated setting.6 In contrast, relatively little is known about the type and quality of HIV care provided to immigration detainees.
Almost 400,000 people are detained annually by Immigration and Customs Enforcement (ICE) in the US. The detained population, with an average daily census of 30,000–33,000, is placed in state prisons, county jails, corporate detention centers, and a small number of facilities run by ICE.7 Despite the wide variety of physical settings, detainees are provided medical care under a common set of administrative ICE rules, and the ability of detainees to access much of this care is directed by one health plan. Because ICE is under no mandate to report basic statistics concerning detainee morbidity or mortality, little is known about the true impact of HIV among detainees or about the medical care afforded to those living with HIV/AIDS. The two broad categories of HIV-related activities within the ICE health care system that we have reviewed are screening for HIV and care for detainees living with HIV/AIDS.
Reporting by advocacy groups has brought to light numerous cases of substandard HIV care for detainees as well as instances of discrimination and harassment based on HIV status.8 Our own work with individual detainees has also revealed many impediments in securing both HIV testing and care. Given the lack of basic epidemiological data, it is difficult to assess the extent of these problems. Consequently, we have turned to the available sources of information concerning HIV care in ICE detention. One source of information from ICE is their response to a Freedom of Information Act request concerning HIV care. Additional information is found in reports by the Office of the Inspector General (OIG) of the Department of Homeland Security (DHS), reports by the Government Affairs Office (GAO) of the US Congress, and reports by advocacy groups presented at US Congressional hearings and to a UN Special Rapporteur.9
We have analyzed the information from these reports on HIV screening and care for ICE detainees in terms of the guidelines published by a leading correctional health accrediting body, the National Commission on Correctional Health Care (NCCHC).10 Based on the available evidence, we are gravely concerned that ICE detainees may be unnecessarily denied the HIV screening and care that they need and to which they are entitled. We are also concerned that ICE has done little to address a culture of stigma and harassment toward detainees living with HIV/AIDS. We provide specific recommendations for improving the standard of HIV screening and care, some specific to HIV and others bearing on other medical problems common among ICE detainees.
ICE health care
Since 1996, increasing numbers of immigrants have been detained in the US as non-criminal detainees. Most of these detainees are eventually deported, but the duration of their detention may range from weeks to years. The health care provided for ICE detainees is directed by a set of rules under the Detention Management Control Program of the Department of Homeland Security.11 This program creates procedures for ICE detention operations but does not carry the force of law. As a consequence, when an individual detention center, or ICE as an agency, fails to provide adequate care for detainees, there are few, if any, consequences. For example, we were recently involved in reviewing autopsy records for a detainee who succumbed to an infection of his heart and blood while in ICE custody.12 This detainee had initially complained for several days of urinary symptoms, and because of his complaints, he was placed into isolation, where his condition deteriorated. While this case is egregious and shocking, it is not the only case in which a detainee was denied life-saving medical care. Two years earlier, a detainee in the same facility died after deteriorating for weeks from kidney failure. Payments to this facility for detention of ICE detainees continued despite the fact that ICE found that this facility provided inadequate care to the detainee who died from kidney failure and, in general, failed to provide adequate care for detainees.
Particular medical policies and reimbursement guidelines are determined by the Division of Immigration Health Services (DIHS), recently incorporated into the DHS from the Health Resources and Services Administration of the US Department of Health and Human Services (HHS). The DIHS guidelines then became part of the overall set of ICE rules for detention operations. Each detention center has a medical unit where detainees should receive a medical screening upon arrival as well as a physical examination within two weeks of detention. The detention center medical unit also provides medical care for detainees who report for sick call. If detainees require care outside the detention center, the medical unit staff must obtain prior approval for this care from the DIHS unless it involves an emergency.13 The DIHS has a set of guidelines for reimbursement of medical care that functions much like a traditional HMO health plan in that potential reimbursement greatly influences delivery of care.14
Until recently, some ICE detainees were actually held because of their HIV status. A little-known aspect of US immigration law is the (now repealed) prohibition against entry for persons with HIV. This prohibition, codified in the Immigration and Nationality Act of 1993, was the product of xenophobia toward refugees from Haiti and other countries in the early 1990s.15 For immigrants in the US without citizenship who contracted HIV, this law required that they leave the US each year to reapply for an HIV waiver for reentry. Failure to conform to any aspect of this law could result in a person being detained and deported. One such ICE detainee had resided in the US for 22 years and contracted HIV from her husband, an American citizen.16 As part of the Congressional reauthorization of the President’s Emergency Plan for AIDS Relief (PEPFAR) in 2008, the HIV travel ban was finally eliminated, and the federal rules enacting this change have recently been adopted.17 However, there is no clear estimate of how many people were detained by ICE during the 15 years that this law was in force.
HIV Screening
The ideal standard for HIV screening among ICE detainees is not in question: routine universal screening for HIV is recommended for all US residents and should be offered to all detainees. In 2006, the CDC updated its general recommendations concerning HIV testing in favor of routine, opt-out screening.18 This was done in recognition of the high number of Americans unknowingly living with HIV (approximately 250,000), the poor ability of clinicians to accurately evaluate risk profiles, and the clear benefits to individual and public health of early detection and treatment. Even if treatment is initiated immediately, later diagnosis predicts a more complicated disease course and worse treatment outcomes.19
However, even before the CDC recommendations for universal HIV screening, there were clear and compelling reasons to institute testing for all ICE detainees. Although little is known about the demographics of ICE detainees, many are known to come from countries with high rates of HIV infection. While specific information about HIV prevalence among detainees is lacking, some information can be inferred from the characteristics of the much larger undocumented population in the US (all of whom are potentially and increasingly at risk for ICE detention). The increased risk for HIV among migrant populations is well documented. In a 2000 report, UNAIDS found that “[m]igrant populations have a greater risk for poor health in general and HIV infection in particular.”20 The inherently unstable social, employment, and housing status of migrant populations may confer greater risk of contracting HIV, and recognition of this possibility has recently prompted HIV researchers to advocate for the use of the GEM (Gender, Economics, Migration) criteria in assessing HIV risk.21
Migration not only confers increased risk for contracting HIV but also relegates migrants to a social stratum that is easily overlooked in any basic analysis of disease prevalence. The invisibility of migrants simultaneously increases their risk of contracting HIV and masks the results of this risk because they are not explicitly included in data collection. With respect to HIV, migrants — who likely constitute much of the ICE detainee population — are consequently folded into the larger categories of “foreign-born” persons or “immigrants.”
The large representation of the Latino/Hispanic community among undocumented immigrants in the US further argues for universal HIV testing for ICE detainees. Based on reporting by the Pew Hispanic Center, almost 60% of undocumented persons in the US are from Mexico.22 When persons from other Latin American nations are included, this proportion increases to roughly 75%. Hispanics are a group that has been disproportionately represented among HIV/AIDS cases since the beginning of the epidemic in the US. In addition to having a case rate almost four times that for Caucasians in the US, Hispanics are more likely to be concurrently diagnosed with HIV and AIDS, representing advanced progression of disease at the time of first diagnosis, a situation that is attributed to inadequate HIV screening in this population.23 Furthermore, HIV-positive Latino migrants in the US have relatively poor access to care and treatment.24
Despite clear rationale for offering universal HIV screening in detention centers, very few detainees are screened for HIV and there is no clear standard that determines who will be offered HIV testing. ICE health guidelines specify that routine mass testing for HIV will not be conducted, and address HIV testing in the following manner: “HIV testing will be approved if a provider determines that the HIV testing is indicated based on clinical evaluation or if the detainee requested the test and it is deemed necessary by the medical provider.”25 Aside from rejecting the current CDC recommendation of universal testing for HIV (euphemistically referred to as “mass testing”), this standard fails to identify the criteria that clinicians should be using to identify detainees for whom an HIV test is clinically indicated or necessary. The old CDC recommendation of screening based on risk factors may be what is intended by this standard, but no specific risk factors are provided. This type of clinical ambiguity (and the inevitable variation in implementation that stems from such an unclear policy) was a factor in the CDC’s change to recommending universal testing.
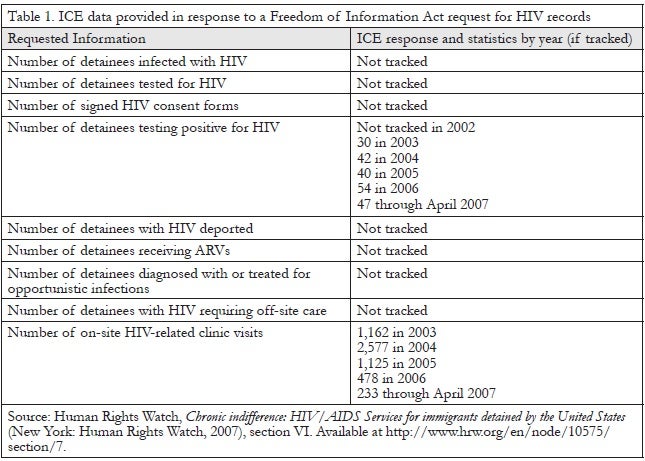
Not only do the ICE guidelines fail to specify the criteria by which detainees should be selected for HIV testing, the limited nature of the available data on tests performed on detainees prevents researchers and advocates from inferring the criteria used. In their response to the HIV Freedom of Information Act request in 2007, ICE reported numbers of positive HIV tests but, alarmingly, had no knowledge of the total number of tests performed or the reasons for testing (see Table 1). In contrast, ICE maintains a very aggressive screening and treatment standard for tuberculosis.
HIV screening with new and widely used rapid tests is simple and inexpensive and does not require sophisticated laboratory facilities.26 Most detention centers should have the ability to carry out the initial HIV screening tests on-site, although confirmatory testing and further care for those with a positive initial test may in some cases require referral to an outside facility. Because the correctional setting creates unique challenges in terms of consent and privacy, we propose that HIV testing be offered to all detainees by a trained HIV testing counselor or medical provider. Post-test notification and counseling for all detainees with a positive initial test should be performed by a medical provider who is also responsible for establishing follow-up medical care. This recommendation amounts to an “opt-in” method of testing, in which testing is offered to all patients but performed only for those who consent to the procedure. A more inclusive approach to HIV testing is the “opt-out” option, in which HIV testing is performed routinely on all patients, much like other blood tests or tests for tuberculosis, unless the patient raises a specific objection.
The CDC has recently published an updated set of guidelines for HIV testing in correctional settings that identifies opt-out screening for HIV as the ultimate goal in correctional settings and provides guidance on other forms of testing that may help facilities or institutions that are not yet ready for an opt-out program.27 These guidelines note that while all patients, whether incarcerated or not, should be afforded HIV testing, there are particular barriers to opt-out testing in correctional settings. Given the multiple deficiencies in detainee medical care, we believe that establishing consistent opt-in HIV testing throughout over 450 detention settings will be a considerable and difficult first step, though opt-out testing remains the ultimate goal for testing in these settings. While many medical settings, and even jails and prisons, may be ready to progress from opt-in to opt-out testing, current ICE practice falls far short of even opt-in testing. Because the ICE and DIHS guidelines fail to clearly identify who should be offered testing, many individual providers may rely on offering testing based on risk profiles, demographics, or unknown variables, all practices that the new CDC guidelines appropriately discourage as primary strategies because they miss a significant percentage of people with HIV.
HIV care
ICE detainees known to have HIV/AIDS are afforded a level of care at odds with accepted standards of practice, even for correctional settings. The relevant guidelines for this care stem from ICE’s own health standards and the guidelines for HIV care established by the National Commission on Correctional Health Care (NCCHC), a monitoring body from which some but not all ICE detention centers are required to seek accreditation.28 The ICE guidelines include HIV on a list of chronic diseases but, aside from the abovementioned language concerning testing, fail to further elaborate on any clinical, laboratory, or other aspects of diagnosis or treatment. In contrast, the NCCHC standards include a detailed set of recommendations for HIV care consistent with the standard of care for HIV treatment in the community.29 These standards and the contrasting reports by advocacy groups and governmental investigations bring into high relief the grim reality of HIV care for ICE detainees.
Initial evaluation
The NCCHC recommends that on arrival in a correctional setting, HIV-positive persons have a thorough medical history, physical examination, and laboratory tests. All HIV-positive detainees should be given influenza, pneumococcal, and hepatitis B vaccinations if they have not yet received them. In addition, every HIV-positive detainee should undergo the necessary tests to determine how far their disease has progressed. Disease progression categories reflect the severity of the disease and are crucial in helping clinicians in correctional settings identify detainees in need of more intensive medical monitoring and care.
For ICE detainees with HIV/AIDS, care on arrival at a detention center bears little resemblance to the NCCHC recommendations. HIV-positive detainees report being asked little about their history of opportunistic infections, CD4 counts, or co-morbidities. Review of medical records from HIV-positive detainees has revealed problems with all of the NCCHC-recommended aspects of the initial evaluation.30 In particular, detainees may not receive any laboratory testing, may not be screened for relevant co-infections (such as hepatitis B and C), and may not be asked about possible medication toxicities. More generally, inadequate health screening for ICE detainees has been reported by the DHS OIG and by advocacy groups. 31 An OIG investigation from 2007 reported deficiencies in providing both initial screenings and physical examinations within two weeks at many ICE detention centers (both public and private).
Treatment monitoring
After the initial health evaluation, the ongoing HIV care received by ICE detainees appears to stray even further from NCCHC guidelines. A crucial component of ongoing care for detainees with HIV is the frequency of follow-up visits, termed “chronic care” visits by ICE. In general, the NCCHC recommends monthly visits for any detainee on antiretroviral therapy (ART) unless the detainee is extremely stable for a prolonged amount of time. Additionally, the NCCHC recommendation that detainees have their HIV/AIDS progression categorized upon arrival is a key component of determining the appropriate frequency of follow-up visits. For detainees with worsening or poorly controlled disease, more frequent visits are recommended. Resistance mutations accumulate the longer a patient is left on a failing drug regimen, making early detection of ART failure essential.32 Under these guidelines, all detainees on ART should receive laboratory tests (CD4 count, viral load, and liver function) every one to three months, and every clinical visit should evaluate the patient for medication toxicity and for new opportunistic infections, malignancies, and other HIV-associated conditions. The NCCHC recommendations also mention conducting a Pap smear every six months in women with HIV and ophthalmologic exams every six months for all detainees with a CD4 count less than 100.33
In stark contrast, the ICE guidelines for HIV visits are simply an extension of the more broad policy on chronic care visits for any chronic disease, which severely restricts access to care for HIV-positive detainees. As evidenced in the ICE response to a 2007 Freedom of Information Act request regarding HIV care for detainees, the frequency of visits is left up to local clinicians, with no specific guidelines for which patients should be seen more or less frequently.34 ICE policies refer to visit frequencies ranging from 14 to 90 days without clarification on why a particular visit frequency was instituted. When asked about what standard applies, the warden of a county jail where ICE detainees are held replied, “I don’t know what standards apply. It’s hard to keep it all straight.” Based on interviews with HIV-positive ICE detainees, it is clear that many are not given the laboratory testing they require and that many remain uncertain about the results of the tests that are performed or about the status of their disease. The clinical consequence of this lack of standards may be poorly controlled HIV/AIDS and unnecessary opportunistic infections (and death) for detainees. Again, these ICE policies concern care delivered inside detention centers. This care is grossly insufficient and bears little resemblance to the care described in the very detailed HIV recommendations of the NCCHC. However, in the common event that a detainee needs his or her chronic care visit outside of the detention center, it is not the ICE policies that apply; in this case, it is the even more restrictive DIHS Covered Services Package that comes into effect.
Treatment authorization requests
Care outside detention centers requires that the detention center medical personnel request prior approval from the DIHS in the form of a treatment authorization request (TAR). Without a pre-approved TAR, the DIHS will not reimburse the local detention center for care. The introduction of the Covered Services Package made clear ICE’s institutional aversion to the care of chronic diseases such as HIV: “The DIHS Medical Dental Detainee Covered Services Package primarily provides health care services for emergency care. Emergency care is defined as ‘a condition that is threatening to life, limb, hearing or sight.’”35 The DIHS has altered the Covered Services Package several times, and the most recent changes, made in 2005, dramatically limited the scope of medical care for detainees. Prior to 2005, the Covered Services Package entitled detainees with chronic medical problems to “chronic care” visits every three months. In 2005, the Covered Services Package was revised to remove this minimum frequency of visits, and it now reads, “[w]e have clarified to providers that the DIHS does not mandate the frequency a detainee is seen or what testing needs to be done by the onsite physician. The responsibility will lie with the provider.”36 With these changes, the DIHS plan moves HIV care further from both accepted medical standards and the recommendations of the NCCHC. The net effect of these changes is to limit care for detainees with HIV.
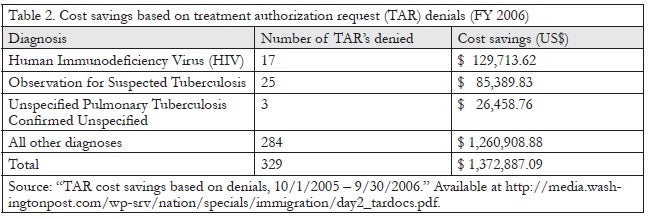
Evidence of this limitation in care for detainees can be found in an internal ICE memo recently made public. In this document, cost savings are presented in terms of TAR refusals.37 Specifically, the memo lists all 329 TAR refusals for fiscal year 2006 by diagnosis, the number of TAR’s refused in each diagnostic category, and cost savings. The most frequently refused TAR’s were for “other chest pain,” “observation of suspected tuberculosis,” “essential hypertension,” “acute pharyngitis,” “hematuria,” and “HIV.” These categories of refusals represented approximately 40% of all TAR refusals in fiscal year 2006, and no information is available about why the TAR’s were refused. However, when the cost savings of these refusals is considered, the greatest single category of cost savings was for “HIV” refusals, totaling about $130,000 saved out of a total of $1.37 million; that is, almost 10% of the total windfall from denial of care requested by onsite providers came from refusal of HIV-related care (Table 2). Although neither the reasons for these denials nor the original requests are available, the extremely limited care allowed by the Covered Services Package raises concerns that detainees were denied care that they genuinely needed and that their clinicians had requested.
Access to medications
Another key aspect of ongoing care for people with HIV is the ability to receive medications consistently. Antiretroviral (ARV) regimens typically require 95% adherence to achieve full viral suppression and to prevent the development of resistance.38 Individuals who develop resistance to their HIV medications are not only at risk for opportunistic infections and other serious HIV-associated illnesses; they may also become resistant to entire classes of HIV medications, making future treatment more complicated, much more expensive, and potentially futile.
Investigation by Human Rights Watch found that detainees in numerous detention centers were unable to reliably and regularly receive their ARV medications.39 One detainee from Jamaica kept a medication diary, and for the month of July 2007, he received his full complement of ARV medicines only 65% of the time. Other detainees have reported receiving their correct medicines between 50% and 75% of the time. Numerous HIV-positive detainees have reported going days and weeks without their medications when being transferred between facilities. The problem is not simply that detention centers are slow to order and deliver medicines to detainees upon arrival. Detainees who actually have their medicines in hand (even when transferring between correctional facilities) report ICE confiscation of their medicine.40 One detainee who initiated ARV medications while held at Rikers Island Jail (not in the custody of ICE) saw her CD4 count climb from less than 50 to over 400. But when she was transferred to ICE custody with her ARVs in hand, her medicines were confiscated, and she went several days without them. She also went six months without any laboratory testing. When this detainee finally did obtain laboratory tests, she was told that her viral load was no longer suppressed, but no resistance testing was ordered.41
Detainees also appear to face difficulties in receiving appropriate prophylactic medications. It is standard to provide patients with low CD4 counts with prophylaxis, typically with inexpensive and well-tolerated medications, to prevent the development of common and deadly opportunistic infections such as PCP pneumonia, toxoplasmosis, and Mycobacterium avium-intracellulare (MAI) infection. However, this standard is often not met in ICE detention settings. One detainee who was transferred from Rikers Island Jail into ICE detention with a CD4 count below 100 was not offered any prophylactic medication. Another detainee died after her prophylactic medication was discontinued upon detention. In the latter case, the detainee knew of her low CD4 count and understood the importance of her medication. She regularly asked ICE medical staff for her medication, but despite the pleas of the detainee and her attorney, no prophylactic medicine was given. This detainee contracted pneumonia, which may have been caused by opportunistic infection with PCP pneumonia, and her condition deteriorated over several weeks. She was transferred to a hospital only when her fellow detainees staged a mass protest demanding that she receive care.42
Our own advocacy work with approximately 60 detainees over the past five years supports the existence of these problems with obtaining medications. In particular, we have become involved when detainees who are stable on a particular regimen first arrive or are transferred into a detention center. If a detainee’s medications are not stocked at the facility, they may wait up to a week to receive them. Some detention centers, such as the Varick Street facility in Manhattan, serve primarily as transfer hubs, where detainees spend a short amount of time while going from one detention center to another. Detainees may arrive at such a transfer hub to find that their medication is not available, and then upon transfer to the next facility, they often face the same problem. Consequently, the common act of transferring detainees between detention centers can have significant health consequences for detainees with HIV (and for those with many other chronic medical problems).
Confidentiality and harassment
Confidentiality is a basic standard in medical care and is particularly important in HIV treatment, given the history of stigmatization of and discrimination against people living with HIV/AIDS. In correctional settings, security concerns are often used to preclude effective patient confidentiality. These two goals are not mutually exclusive, but correctional settings do represent unique challenges, as noted in the recent CDC guidelines and in the NCCHC HIV recommendations, which caution that “the major barrier to care in correctional settings is the difficulty in maintaining confidentiality.”43 Accordingly, the NCCHC recommends that all correctional institutions establish clear, detailed plans to ensure confidential treatment for detainees, especially those requiring daily medications.
This has not been done in most ICE facilities, and it presents a major challenge to appropriate care for detainees with HIV. An ICE detainee held at Bergen County Jail in New Jersey reported that detainees congregate around a pill cart to receive their medicines and that medical charts, including that of this detainee, are sometimes left open for all to see.44 This same detainee was asked by an ICE officer, “Are you the one that’s HIV positive?” while standing with a group of detainees. Knowledge of this detainee’s HIV status quickly spread among other detainees. Similar breaches of confidentiality in medication delivery have been reported in other facilities. In another detention center, an HIV-positive detainee stated, “There is no order to it and no private space. The other detainees are too interested in my condition and ask me why I take so many meds.” A detainee held in another facility, who was originally trained as a pharmacist, reported that “[t]here seemed to be no system for giving us the AIDS drugs.” This detainee reported that once his HIV status and sexual orientation became known, he was subjected to verbal, physical, and sexual abuse that relented only when his attorney was able to secure a transfer to another facility. Unfortunately, he was transferred without any medication, and he had to wait two and a half weeks to resume his medicines after arriving at the new facility. Against ICE policies, this detainee was charged fees for some of his sick call requests. Other detainees have reported being charged for their HIV medicines and have been incorrectly been told that, because they were not residents of a particular state, their HIV medicines would not be obtainable. Such cases suggest a lack of action by ICE to prevent harassment, discrimination, and breaches of confidentiality concerning HIV-positive detainees.
Human rights and legal consequences
There is little doubt that detaining authorities have an obligation to provide basic medical care to detainees. Human rights organizations have cited multiple sources of international law in asserting a legal basis for detainee medical care, including the International Covenant on Civil and Political Rights and components of the UN Convention Relating to the Status of Refugees. The US Government is a party to both of these agreements.45 A promising recent development is the wide interest of the US Congress and the Obama Administration in passage of a bill that would define and guarantee a right to medical care for all detainees.
Because the legal right to medical care for ICE detainees has yet to be established, a number of advocacy groups have pursued litigation against the federal government in cases of death or adverse medical outcomes. There are some rights that flow to detainees based on protections of the US Constitution. While Estelle v. Gamble established a right to medical care for prisoners based on protection from cruel and unusual punishment (Eighth Amendment), immigrant detainees theoretically enjoy the protection against punishment before due process (Fifth Amendment) that is guaranteed to any persons in the custody of the US Government.46 Recently, a US Federal District Court allowed a suit against ICE to proceed in the case of a detainee who died of penile cancer after ICE deemed the request for a biopsy of a bleeding penile lesion to be “elective.” In the judge’s opinion in this case, the government’s own records “bespeak of conduct that transcends negligence by miles. It bespeaks of conduct that, if true, should be taught to every law student as conduct for which the moniker ‘cruel’ is inadequate.”47 One comprehensive approach to litigation would involve certification of a group of detainees (or all detainees) as a class, allowing a class action suit against ICE for inadequate medical care. We have recently written an amicus brief in support of such a motion for a case in US Federal Court.
In some instances, local county or municipal officials may take up advocacy on behalf of detainees. In a case in 2004, the DIHS refused a detainee a physician-recommended test for bladder cancer. The detainee, held in a county jail in Pennsylvania, appealed the DIHS refusal to a county solicitor, who determined that the procedure was clearly required and within the obligation of the DIHS to reimburse. Upon this decision, ICE quickly transferred the detainee to another county jail where the ruling of the county solicitor was not enforceable.48
In our own advocacy efforts, we have attempted to use the basic tools of human rights in seeking medical care for detainees. Operating in a substantial information vacuum, we have relied on advocacy groups, families of detainees, and detainees themselves to complement what ICE reports publicly about the health care afforded to detainees. Because some information is released about individual detainee deaths (by families, advocacy groups, and ICE), we started our analysis by looking for systemic problems that may be reflected in individual deaths.49 We have also had mixed success in adapting the medical asylum evaluation/affidavit for use on behalf of ICE detainees who are not applying for asylum. The most comprehensive instances have involved review of medical records (requested by the detainee) followed by a visit to the detention center to collect a history from and perform a physical examination of the detainee. The results of these visits are used to create a document that the detainee may use to ask for medical parole from detention, better medical care while detained, or to secure care after deportation. In cases of medical parole, each instance of success required that we also secure outside medical care for detainees in the community, which has been particularly difficult to do in cases involving poor mental health. Unfortunately, in a few cases (including a person with HIV), detainees for whom we advocated were abruptly transferred to remote facilities, thousands of miles away and far from medical and legal advocacy.
Recommendations
Our review of ICE care for detainees with HIV reveals several important failures in care. These appeared to include inadequate initial screening, ongoing care that was confusing and lacked standardization, and barriers to required care outside ICE facilities. In addition, ICE appears not to have undertaken effective efforts to maintain a confidential environment, free from harassment, for HIV-positive detainees. Some of the recommendations offered below are specific to HIV care, while others address larger, more systemic issues with the ICE health care system.
- Screening. ICE should offer routine HIV testing to all detainees. Detainees found to have positive tests should be counseled and evaluated for treatment by qualified medical providers, based on the current medical standards of the NCCHC and the CDC. Before deportation, HIV-positive detainees undergoing treatment should have discharge planning and follow-up care established.
- Care. ICE must ensure that detainees with HIV who require treatment are provided appropriate care, including regular exams, laboratory tests, and antiretroviral medications in accordance with NCCHC guidelines. Because the quality of ICE health care for HIV-positive detainees is in question, ICE should perform a system-wide needs assessment of current HIV care to determine whether appropriate HIV care can reasonably be delivered at current ICE detention centers. In order to ensure NCCHC compliance and a generally acceptable level of HIV care, ICE will likely need to invest further resources in medical care and consider medical parole in cases where acceptable care cannot be delivered. Under no circumstances should any detainee be asked to pay for any form of medical care, including HIV treatment.
- Health statistics. ICE should record, monitor, and report (to a public health agency outside of the DHS, such as the CDC or HHS) information about individual HIV tests as well as statistics concerning the percentage of positive tests, the stage of HIV at diagnosis, treatment initiation, and follow up. In addition, ICE should track all detainees on ARVs to ensure that there is no interruption of their medication, from the day of detention, through any transfers, and until release, parole, or deportation. Every facility that houses ICE detainees should report these statistics to ICE, who in turn should analyze the data and report a population-level analysis of these basic HIV variables.
- Confidentiality and harassment. ICE should provide all personnel training to minimize harassment of HIV-positive detainees and ensure confidentiality. This training should not be limited to medical staff. In addition, ICE should assess the level of confidentiality available to HIV-positive detainees when receiving treatment or other forms of care. If ICE is unable to ensure that confidentiality will be ensured in a facility, HIV-positive detainees should not be detained there.
- General health care for ICE detainees. ICE must define and guarantee medical care for detainees as a matter of law. Many of the cases presented here of HIV-positive detainees involve violations of existing ICE guidelines. As the GAO and the OIG have revealed, ICE is unaware of many violations of its own policy that occur in its facilities. Without a legal mandate to enforce these “guidelines,” detainee health care, including care for HIV-positive detainees, will continue to suffer.
- Medical parole. ICE should endeavor to avoid detention when persons are seriously ill and require a high level of medical care. In addition, until detention policies are improved to guarantee an acceptable level of medical care, detainees who require even moderate levels of medical care, such as daily medication, should be considered for medical parole unless ICE can affirmatively establish the ability of a detention center to provide such care.
- Treatment authorization request process. ICE and the DIHS should standardize the TAR process, including criteria for approval and denial. In addition, a transparent appeals process that includes mandatory review of TAR denials by physicians should be instituted.
Our examination of ICE detention policies and practices reveals a system that is unable to provide the HIV screening and care that detainees deserve. These deficiencies appear to be systemic and are unlikely to be addressed without the fundamental changes suggested above. To detain someone in a system in which they will likely receive medical care that is well below existing community standards is a violation of the most basic aspects of the social contract and of concepts of human rights. Because the ethical reasons for providing adequate medical care to detainees with HIV have not yet prevailed, it appears critical that legal protections be immediately established. The lack of accountability for providing HIV care in detention is further enabled by widespread secrecy concerning medical outcomes within the vast system of immigrant detention operated by ICE and the Department of Homeland Security. A great many more medical, legal, and public health resources must be brought to bear on this inadequate system of medical care.
Homer D. Venters, MD, is Clinical Instructor at the NYU School of Medicine and an attending physician at the Bellevue/NYU Program for Survivors of Torture.
Jennifer McNeely, MD, is Clinical Instructor at the NYU School of Medicine and an attending physician at the Bellevue HIV clinic.
Allen S. Keller, MD, is Associate Professor at the NYU School of Medicine and the founder and director of the NYU Center for Health and Human Rights.
Please address correspondence to the authors c/o Homer D. Venters, VA NY Harbor 15N–028BN, 423 E 23rd St., New York, NY, USA, 10010, email: homer.venters@med.nyu.edu.
References
1. C. G. Beckwith, S. Atunah-Jay, J. Cohen, et al., “Feasibility and acceptability of rapid HIV testing in jail,” AIDS Patient Care and STDs 21/1 (2007), pp. 41–47.
2. K. M. Blankenship, A. B. Smoyer, S. J. Bray, and K. Mattocks, “Black-white disparities in HIV/AIDS: The role of drug policy and the corrections system,” Journal of Health Care for the Poor and Underserved 16/4 Supp. A (2005), pp. 140–156.
3. N. N. Dubler, C. M. Bergmann, and M. E. Frankel, “Management of HIV infection in New York State prisons,” Columbia Human Rights Law Review 21/2 (1990), pp. 363–400.
4. S. J. Klein, D. A. O’Connell, B. S. Devore, et al., “Building an HIV continuum for inmates: New York State’s criminal justice initiative,” AIDS Education and Prevention 14/5 Supp. B (2002), pp. 114–123.
5. Centers for Disease Control (CDC), “Public health service guidelines for counseling and antibody testing to prevent HIV infection and AIDS,” Morbidity and Mortality Weekly Report 36/31 (1987), pp. 509–515; T. M. Hammett, “HIV/AIDS and other infectious diseases among correctional inmates: Transmission, burden, and an appropriate response,” American Journal of Public Health 96/6 (2006), pp. 974–978.
6. H. Dean, A. Lansky, and P. Flemming, “HIV surveillance methods for the incarcerated population,” AIDS Education and Prevention 14/5 Supp. B (2002), pp. 65–74.
7. Office of Inspector General, Department of Homeland Security, Treatment of immigration detainees housed at immigration and customs enforcement facilities (Washington, DC: US Department of Homeland Security, 2006). Available at http://trac.syr.edu/immigration/library/P1598.pdf.
8. Human Rights Watch, Chronic indifference: HIV/AIDS services for immigrants detained by the United States (New York: Human Rights Watch, 2007). Available at http://www.hrw.org/en/reports/2007/12/05/chronic-indifference; D. Priest and A. Goldstein, “Careless detention: Medical care in immigrant prisons; System of neglect,” Washington Post (May 11, 2008). Available at http://www.washingtonpost.com/wp-srv/nation/specials/immigration/cwc_d1p1.html.
9. Detention and Deportation Working Group and Lutheran Immigration and Refugee Service and Detention Watch Network, Briefing materials for the United Nations Special Rapporteur on the human rights of migrants (2007). Available at http://www.aclu.org/pdfs/humanrights/detention_deportation_briefing.pdf.
10. National Commission on Correctional Health Care, NCCHC clinical guideline for health care in correctional settings: HIV infection (Chicago, IL: NCCHC, 2006). Available at http://www.ncchc.org/resources/clinicalguides/Adult_HIV.pdf.
11. Office of Inspector General (see note 7).
12. N. Bernstein, “Another jail death, and mounting questions,” New York Times (January 27, 2009).
13. Office of Inspector General (see note 7).
14. N. Bernstein, “Few details on immigrants who died in custody,” New York Times (May 5, 2008).
15. A. Sullivan, “Phobia at the gates,” Washington Post (May 14, 2008).
16. Human Rights Watch (see note 8).
17. K. Dailey, “Goodbye to an old ban,” Newsweek (July 28, 2008).
18. B. Branson, “Current HIV epidemiology and revised recommendations for HIV testing in health-care settings,” Journal of Medical Virology 79/Supp. 1 (2007), pp. S6–S10.
19. C. L. Galletly, S. D. Pinkerton, and A. E. Petroll, “CDC recommendations for opt-out testing and reactions to unanticipated HIV diagnoses,” AIDS Patient Care and STDs 22/3 (2008), pp. 189–193.
20. UNESCO/UNAIDS, Migrant populations and HIV/AIDS (Paris, France: UNESCO, 2000). Available at http://data.unaids.org/Publications/IRC-pub01/JC397-MigrantPop_en.pdf.
21. S. L. Dworkin and A. A. Ehrhardt, “Going beyond ‘ABC’ to include ‘GEM’: Critical reflections on progress in the HIV/AIDS epidemic,” American Journal of Public Health 97/1 (2007), pp. 13–18.
22. J. S. Passel, Estimate of the size and characteristics of the undocumented population (Washington, DC: Pew Hispanic Center, 2005). Available at http://pewhispanic.org/files/reports/44.pdf.
23. S. Deren, M. Shedlin, C. U. Decena, and M. Mino, “Research challenges to the study of HIV/AIDS among migrant and immigrant Hispanic populations in the United States,” Journal of Urban Health 82/2 Supp. 3 (2005), pp. iii13–iii25.
24. M. T. Serrano, N. H. Smith, and W. X. Shandera, “Epidemiology of human immunodeficiency virus infection in Central Americans treated in Harris County, Texas Hospital District facilities,” American Journal of Tropical Medicine and Hygiene 57/6 (1997), pp. 678–682.
25. Human Rights Watch (see note 8), emphasis in original.
26. R. MacGowan, A. Margolis, A. Richardson-Moore, et al., “Voluntary rapid human immunodeficiency virus (HIV) testing in jails,” Sexually Transmitted Diseases 36/2 Supp. (2009), pp. S9–S13.
27. Centers for Disease Control and Prevention, HIV testing implementation guidance for correctional settings (2009). Available at http://www.cdc.gov/hiv/topics/testing/resources/guidelines/correctional-settings/index.htm.
28. National Commission on Correctional Health Care (see note 10).
29. Ibid.
30. Human Rights Watch (see note 8).
31. Office of Inspector General (see note 7); Detention and Deportation Working Group (see note 9).
32. Panel on Antiretroviral Guidelines for Adults and Adolescents, Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (Washington, DC: US Department of Health and Human Services, 2008). Available at http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf.
33. National Commission on Correctional Health Care (see note 10).
34. Human Rights Watch (see note 8), section VI (discussion of the ICE response to the Freedom of Information Act request) and Appendix (text of Freedom of Information Act request).
35. Division of Immigration Health Services, DIHS medical dental detainee covered services package (Washington, DC: DIHS, 2005).
36. Division of Immigration Health Services, Summary of changes to the DIHS detainee covered services package (Washington, DC: DIHS, 2005).
37. D. Priest and A. Goldstein, “Careless detention: Medical care in immigrant prisons,” Washington Post (May 11, 2008). Available at http://www.washingtonpost.com/wp-srv/nation/specials/immigration/index.html (under “Document Archive”).
38. D. L. Paterson, S. Swindells, J. Mohr, et al., “Adherence to protease inhibitor therapy and outcomes in patients with HIV infection,” Annals of Internal Medicine 133/1 (2000), pp. 21–30.
39. Human Rights Watch (see note 8).
40. S. Patel and T. Jawetz, Conditions of confinement in immigration detention facilities (New York: Women’s Commission for Refugee Women and Children, 2007).
41. Human Rights Watch (see note 8).
42. Ibid.; Bernstein (see note 12).
43. National Commission on Correctional Health Care (see note 10).
44. Human Rights Watch (see note 8).
45. Detention and Deportation Working Group (see note 9).
46. Human Rights Watch (see note 8).
47. H. Weinstein, “Judge calls immigration officials’ decision ‘beyond cruel,’” Los Angeles Times (March 13, 2008).
48. T. Jawetz/American Civil Liberties Union National Prison Project, “Presentation on medical care and deaths in ICE custody, for a hearing on ‘Detention and removal: Immigration detainee medical care’ before the House Subcommittee on Immigration, Citizenship, Refugees, Border Security, and International Law, October 4, 2007” (Washington, DC, October 4, 2007). Available at http://judiciary.house.gov/hearings/pdf/Jawetz071004.pdf.
49. H. Venters, D. Dasch-Goldberg, A. Rasmussen, and A. S. Keller, “Into the abyss: Mortality and morbidity among detained immigrants,” Human Rights Quarterly 31/2 (2009), pp. 474–495.